Abstract
Rev Bras Ter Intensiva. 2018;30(1):28-34
DOI 10.5935/0103-507X.20180008
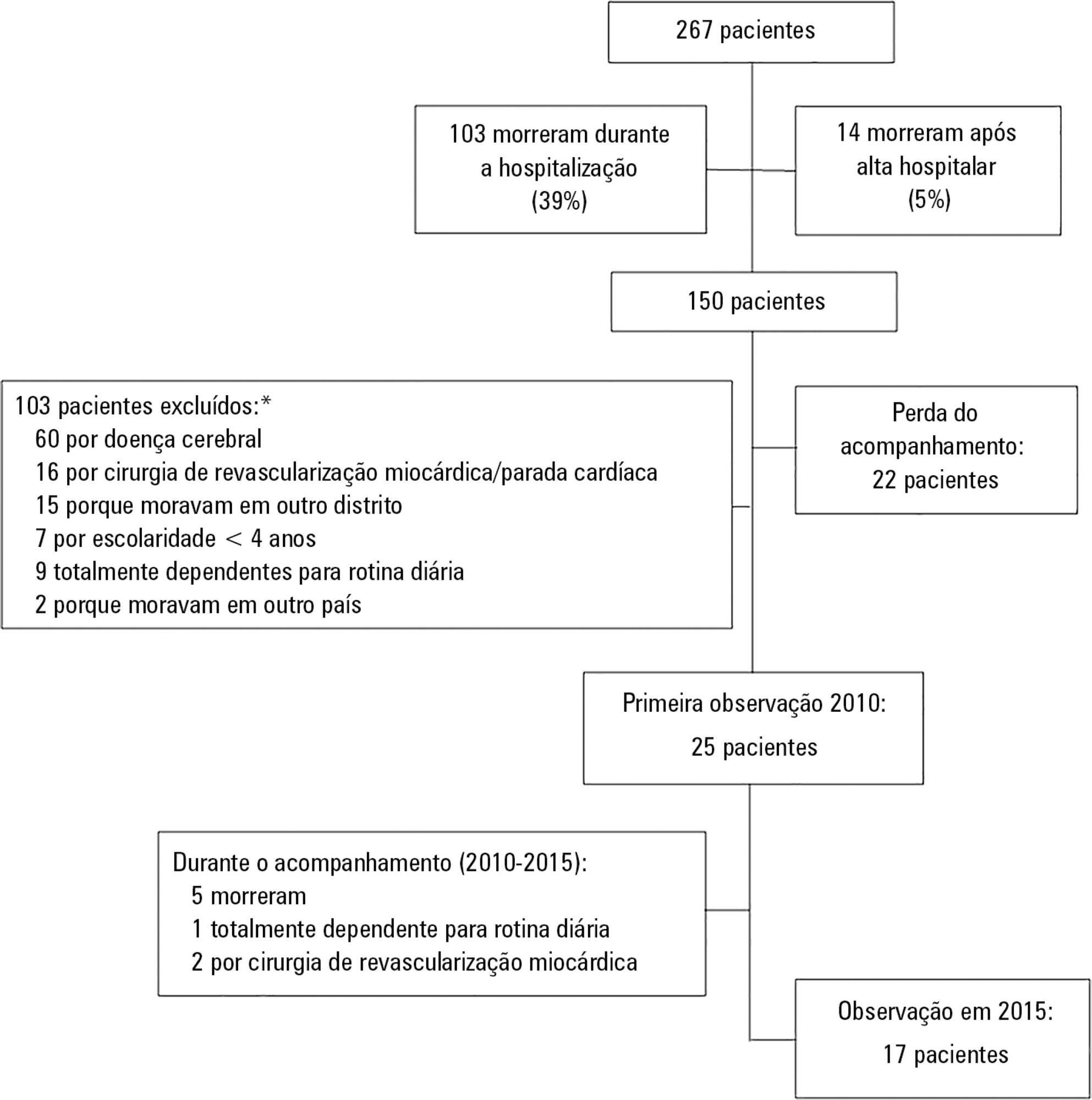
To investigate the longterm psychological outcome in survivors of critical illness after intensive care unit discharge.
A prospective cohort of survivors admitted to a mixed intensive care unit between January and September 2010 was evaluated six months and five years after hospital discharge. The Dementia Rating Scale-2, the Hospital Anxiety and Depression Scale, the Posttraumatic stress syndrome 14-questions inventory, the Euro Quality of Life 5 Dimensions (EQ-5-D), and the Visual Analogue Scale (EQ VAS) were assessed at both follow-up periods.
Of 267 patients, 25 patients were evaluated at 6 months after discharge (62 ± 16 years); 12 (48%) presented cognitive impairment, 6 (24%) anxiety, 4 (16%) depression, and 4 (16%) post-traumatic stress disorder. Among those re-evaluated five years after discharge (n = 17; 65 ± 15 years), the frequency of cognitive impairment dropped from 8 (47%) to 3 (18%) (p = 0.063), due to improvement in these patients over time, and other patients did not acquire any dysfunction after discharge. At five years after discharge, only two patients (12%) reported anxiety, and none had depression or post-traumatic stress disorder. No differences were found between the six-month and five-year follow-ups regarding EQ-5-D and EQ VAS.
Survivors do not show a progressive decline in cognitive function or quality of life within five years after intensive care unit discharge. Psychopathological symptoms tend to decrease with time.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):42-49
DOI 10.5935/0103-507X.20180009
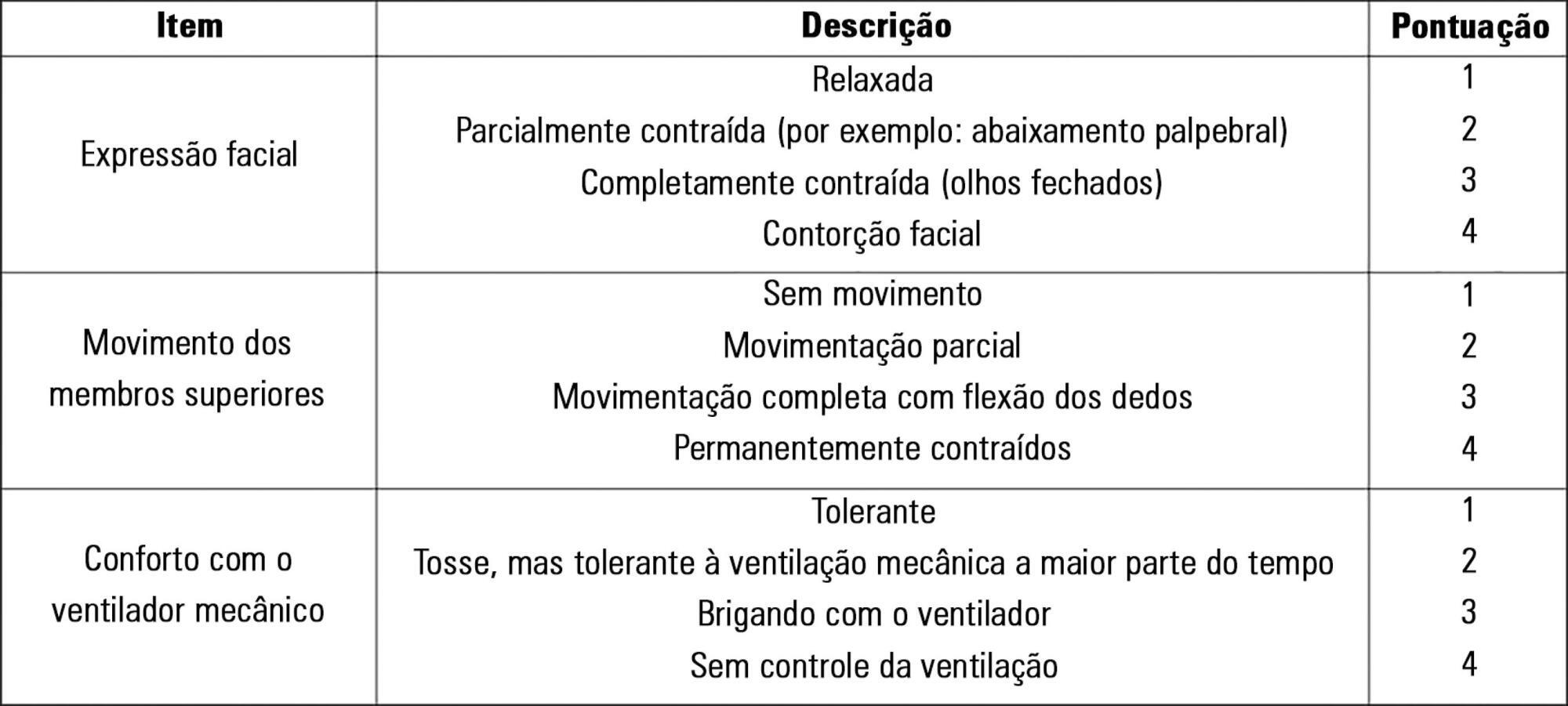
To evaluate the validity and reliability of the Brazilian version of the Behavioral Pain Scale (BPS-Br) in victims of traumatic brain injury.
Observational prospective study with paired and repeated measures conducted at two intensive care units (clinical and surgical) of a large general hospital. The convenience sample consisted of adult victims of moderate or severe penetrating or blunt craniocerebral trauma who were sedated and mechanically ventilated. A total of 432 paired observations were performed by independent evaluators simultaneously, prior to eye cleaning, during eye cleaning, during tracheal aspiration and after tracheal aspiration. Sociodemographic, clinical, trauma-related, sedoanalgesia and physiological parameter data (heart rate, systolic and diastolic blood pressure) were collected. The discriminant validity was tested using the Friedman and Wilcoxon paired tests. The intraclass correlation coefficient and Cohen's Kappa coefficient were used to evaluate the reliability. The Spearman correlation test was used to test the association between clinical variables and BPS-Br scores during tracheal aspiration.
There was a significant increase in the physiological parameters during tracheal aspiration, but without correlation with the BPS-Br scores. Pain was significantly more intense during tracheal aspiration (p < 0.005). Satisfactory interobserver agreement was found, with an intraclass correlation coefficient of 0.95 (0.90 - 0.98) and Kappa coefficient of 0.70.
Brazilian version of the Behavioral Pain Scale scores increased during tracheal aspiration. The Brazilian version of the scale was valid and reliable for pain assessment of traumatic brain injury victims undergoing tracheal aspiration.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):144-152
DOI 10.5935/0103-507X.20180028
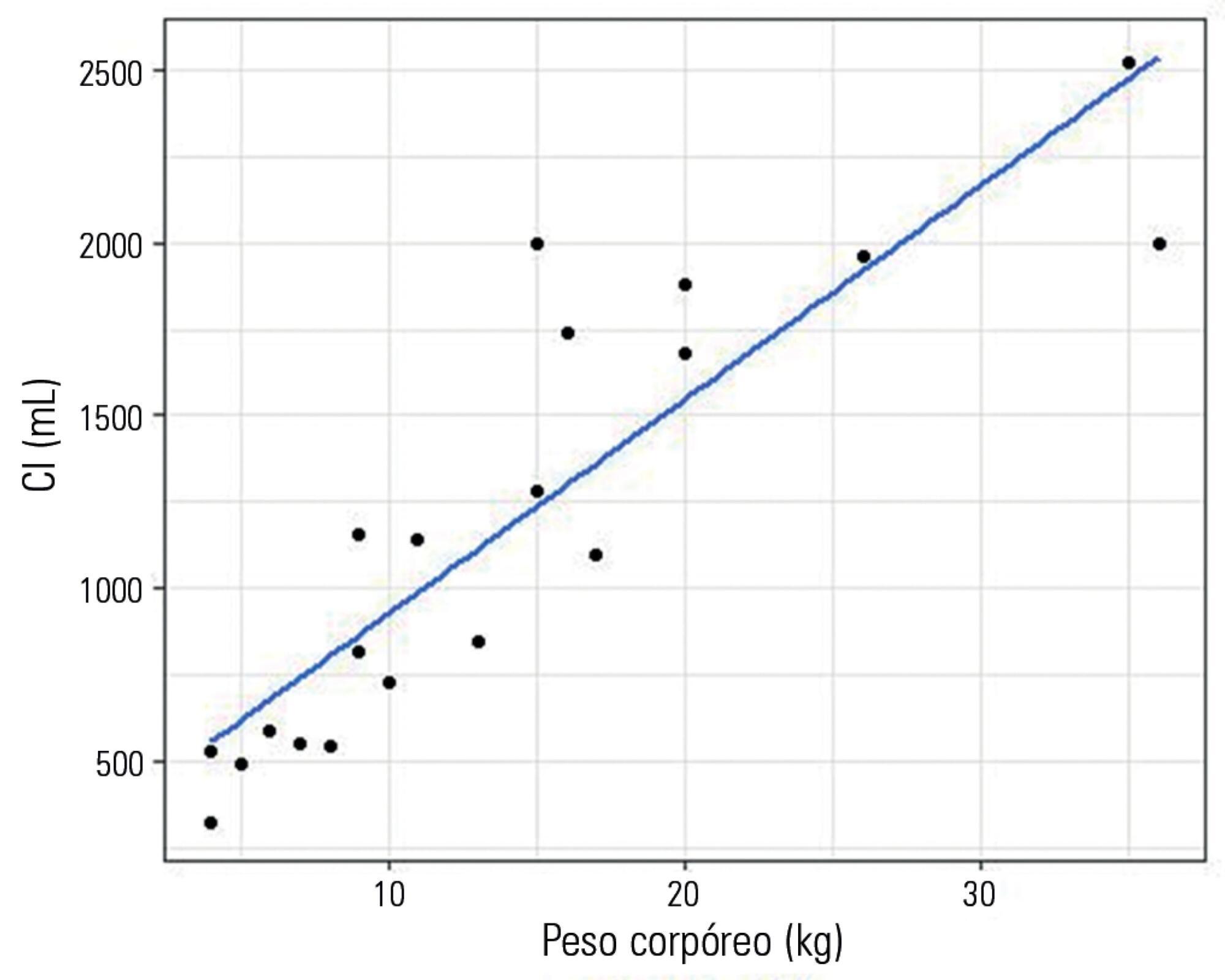
To evaluate a novel physiological approach for setting the tidal volume in mechanical ventilation according to inspiratory capacity, and to determine if it results in an appropriate mechanical and gas exchange measurements in healthy and critically ill dogs.
Twenty healthy animals were included in the study to assess the tidal volume expressed as a percentage of inspiratory capacity. For inspiratory capacity measurement, the mechanical ventilator was set as follows: pressure control mode with 35cmH2O of inspired pressure and zero end-expiratory pressure for 5 seconds. Subsequently, the animals were randomized into four groups and ventilated with a tidal volume corresponding to the different percentages of inspiratory capacity. Subsequently, ten critically ill dogs were studied.
Healthy dogs ventilated with a tidal volume of 17% of the inspiratory capacity showed normal respiratory mechanics and presented expected PaCO2 values more frequently than the other groups. The respiratory system and transpulmonary driving pressure were significantly higher among the critically ill dogs but below 15 cmH2O in all cases.
The tidal volume based on the inspiratory capacity of each animal has proven to be a useful and simple tool when setting ventilator parameters. A similar approach should also be evaluated in other species, including human beings, if we consider the potential limitations of tidal volume titration based on the calculated ideal body weight.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):153-159
DOI 10.5935/0103-507X.20180030
To investigate prognostic factors among critically ill patients with community-acquired bacterial meningitis and acute kidney injury.
A retrospective study including patients admitted to a tertiary infectious disease hospital in Fortaleza, Brazil diagnosed with community-acquired bacterial meningitis complicated with acute kidney injury. Factors associated with death, mechanical ventilation and use of vasopressors were investigated.
Forty-one patients were included, with a mean age of 41.6 ± 15.5 years; 56% were males. Mean time between intensive care unit admission and acute kidney injury diagnosis was 5.8 ± 10.6 days. Overall mortality was 53.7%. According to KDIGO criteria, 10 patients were classified as stage 1 (24.4%), 18 as stage 2 (43.9%) and 13 as stage 3 (31.7%). KDIGO 3 significantly increased mortality (OR = 6.67; 95%CI = 1.23 - 36.23; p = 0.028). Thrombocytopenia was not associated with higher mortality, but it was a risk factor for KDIGO 3 (OR = 5.67; 95%CI = 1.25 - 25.61; p = 0.024) and for mechanical ventilation (OR = 6.25; 95%CI = 1.33 - 29.37; p = 0.02). Patients who needed mechanical ventilation by 48 hours from acute kidney injury diagnosis had higher urea (44.6 versus 74mg/dL, p = 0.039) and sodium (138.6 versus 144.1mEq/L; p = 0.036).
Mortality among critically ill patients with community-acquired bacterial meningitis and acute kidney injury is high. Acute kidney injury severity was associated with even higher mortality. Thrombocytopenia was associated with severer acute kidney injury. Higher urea was an earlier predictor of severer acute kidney injury than was creatinine.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):160-165
DOI 10.5935/0103-507X.20180034
To compare the prevalence of malnutrition during two time periods in a pediatric intensive care unit.
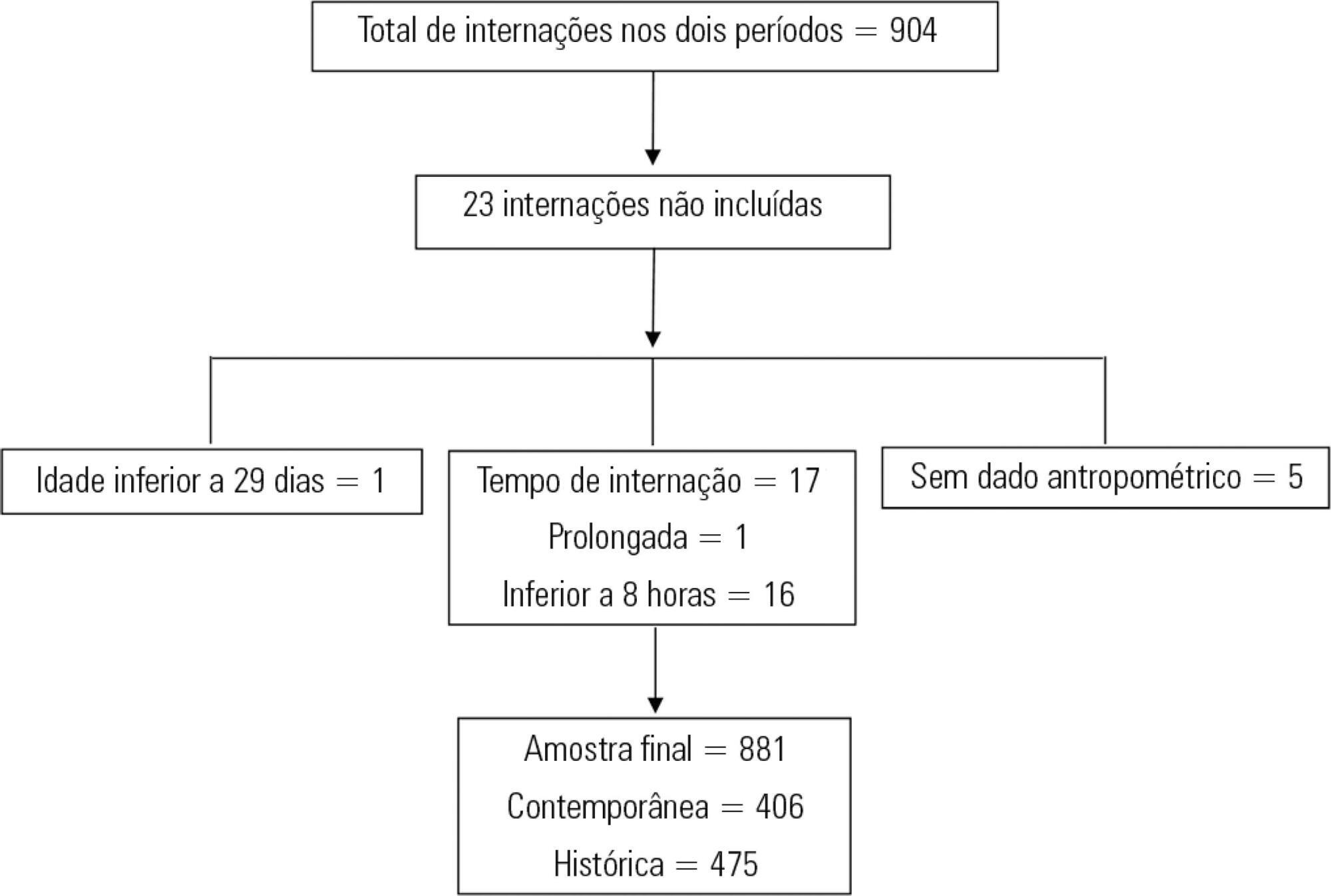
This was a retrospective cross-sectional study of patients admitted to the pediatric intensive care unit of a university hospital during two one-year periods with an interval of four years between them. Nutritional evaluation was conducted based on weight and height measured at admission. The body mass index-for-age was the parameter chosen to evaluate nutritional status, as classified according to the World Health Organization, according to age group.
The total sample size was 881 (406 in the contemporary sample and 475 in the historical sample). There was a significant reduction in malnutrition in the contemporary sample (p = 0.03). Malnourishment in patients in the historical sample was significantly associated with mortality and length of stay, while malnourishment in patients in the contemporary sample was not associated with worse outcomes.
There was a significant reduction in malnutrition among patients in the same pediatric intensive care unit when comparing the two time periods. Our findings of a change in nutritional profile in critically ill patients corroborate the nutritional status data of children and adolescents worldwide.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):166-173
DOI 10.5935/0103-507X.20180022
To assess the predictors of de novo atrial fibrillation in patients in a non-cardiac intensive care unit.
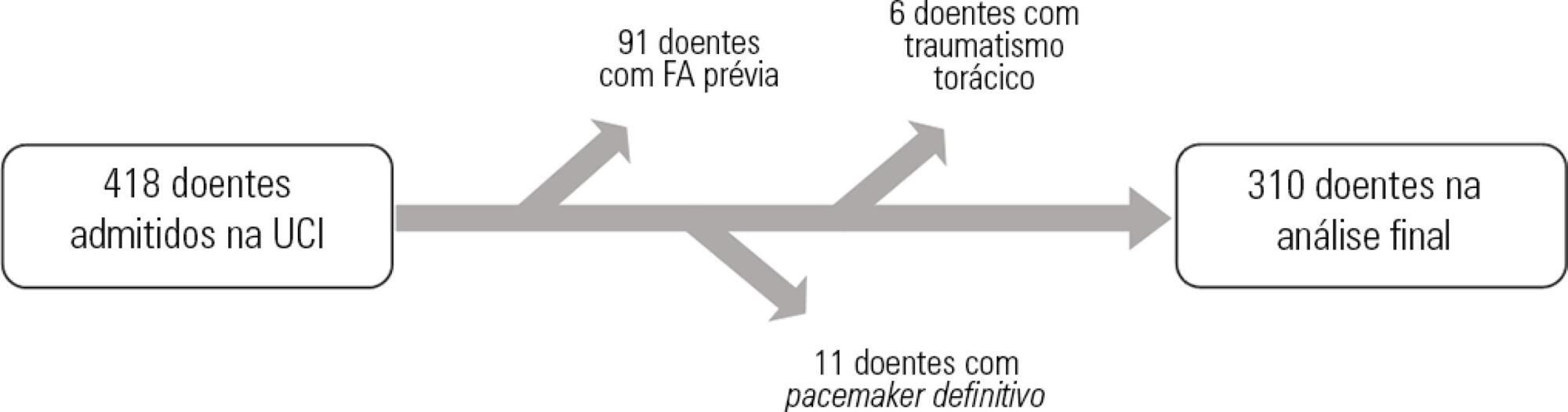
A total of 418 hospitalized patients were analyzed between January and September 2016 in a non-cardiac intensive care unit. Clinical characteristics, interventions, and biochemical markers were recorded during hospitalization. In-hospital mortality and length of hospital stay in the intensive care unit were also evaluated.
A total of 310 patients were included. The mean age of the patients was 61.0 ± 18.3 years, 49.4% were male, and 23.5% presented de novo atrial fibrillation. The multivariate model identified previous stroke (OR = 10.09; p = 0.016) and elevated levels of pro-B type natriuretic peptide (proBNP, OR = 1.28 for each 1,000pg/mL increment; p = 0.004) as independent predictors of de novo atrial fibrillation. Analysis of the proBNP receiver operating characteristic curve for prediction of de novo atrial fibrillation revealed an area under the curve of 0.816 (p < 0.001), with a sensitivity of 65.2% and a specificity of 82% for proBNP > 5,666pg/mL. There were no differences in mortality (p = 0.370), but the lengths of hospital stay (p = 0.002) and stay in the intensive care unit (p = 0.031) were higher in patients with de novo atrial fibrillation.
A history of previous stroke and elevated proBNP during hospitalization were independent predictors of de novo atrial fibrillation in the polyvalent intensive care unit. The proBNP is a useful and easy- and quick-access tool in the stratification of atrial fibrillation risk.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):174-180
DOI 10.5935/0103-507X.20180023
To compare the neuropsychomotor development in the first year of life of premature infants with and without bronchopulmonary dysplasia.
A cross-sectional retrospective study was conducted between January 1, 2014, and December 30, 2015, with premature infants weighing < 1,500g at birth and diagnosed with bronchopulmonary dysplasia at the corrected ages of 6 and 9 months, assessed using the DENVER II Developmental Screening Test. Quantitative variables were described as the means, medians and standard deviations. Variables with normal distribution were tested using Student's t test; otherwise, the Mann-Whitney test was used, considering significance at p-value < 0.05. Qualitative variables were expressed as frequencies and percentages. Logistic regression was used with odds ratio analysis to evaluate the effects of other variables as risk factors for changes in neuropsychomotor development.
Infants with bronchopulmonary dysplasia showed greater developmental delay compared with those without bronchopulmonary dysplasia (p-value = 0.001). The factors associated with a higher incidence of changes in neuropsychomotor development, in addition to bronchopulmonary dysplasia, were antenatal steroid, gender, birth weight, 5-minute Apgar score, Score for Neonatal Acute Physiology-Perinatal Extension, duration of oxygen therapy, duration of mechanical ventilation and length of hospital stay. Other variables may also have influenced the result, such as drug use by mothers of infants with bronchopulmonary dysplasia.
Bronchopulmonary dysplasia associated with other pre- and postnatal factors may be considered a risk factor for delayed neuropsychomotor development in the first year of life in premature infants born weighing less than 1,500g.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):181-186
DOI 10.5935/0103-507X.20180032
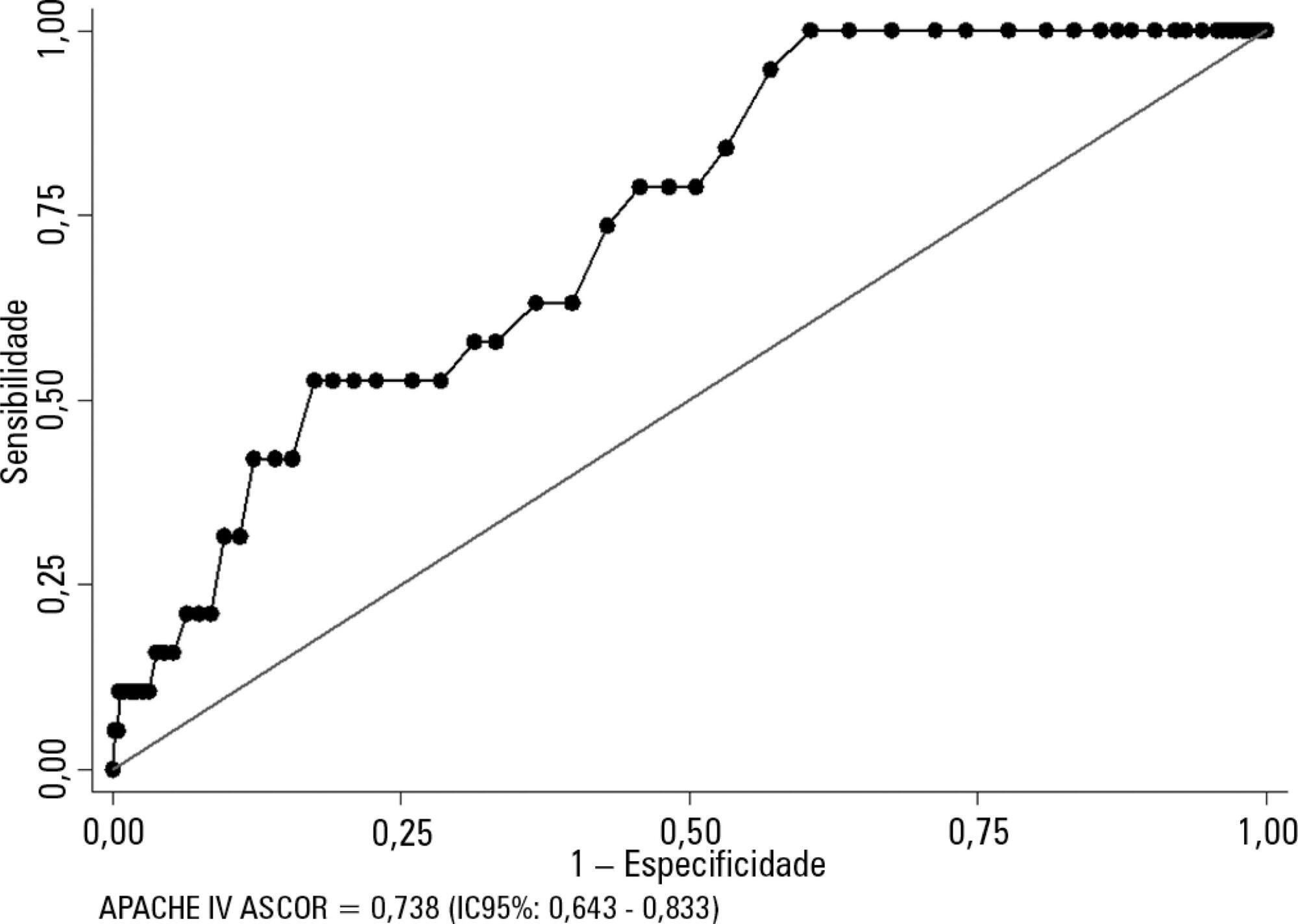
To evaluate the calibration and discrimination of APACHE IV in the postoperative period after kidney transplantation.
This clinical cohort study included 986 hospitalized adult patients in the immediate postoperative period after kidney transplantation, in a single center in southern Brazil.
Kidney transplant patients who died in hospital had significantly higher APACHE IV values and higher predicted mortality. The APACHE IV score showed adequate calibration (H-L 11.24 p = 0.188) and a good discrimination ROC curve of 0.738 (95%CI 0.643 - 0.833, p < 0.001), although SMR overestimated mortality (SMR = 0.73; 95%CI: 0.24 - 1.42, p = 0.664).
The APACHE IV score showed adequate performance for predicting hospital outcomes in the postoperative period for kidney transplant recipients.