Abstract
Crit Care Sci. 2024;36:e20240208en
DOI 10.62675/2965-2774.20240208-en
To evaluate the association between driving pressure and tidal volume based on predicted body weight and mortality in a cohort of patients with acute respiratory distress syndrome caused by COVID-19.
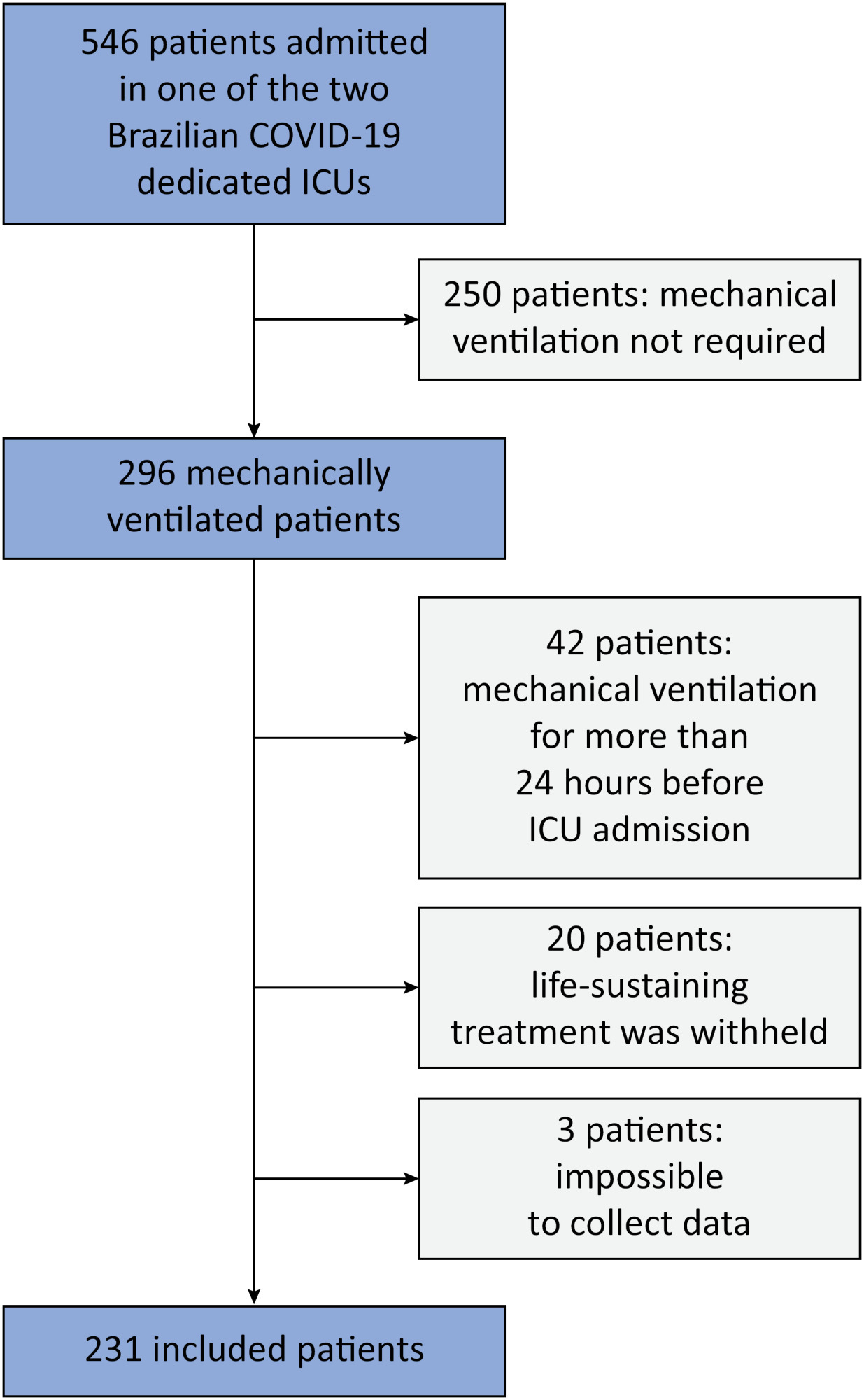
This was a prospective, observational study that included patients with acute respiratory distress syndrome due to COVID-19 admitted to two intensive care units. We performed multivariable analyses to determine whether driving pressure and tidal volume/kg predicted body weight on the first day of mechanical ventilation, as independent variables, are associated with hospital mortality.
We included 231 patients. The mean age was 64 (53 - 74) years, and the mean Simplified Acute and Physiology Score 3 score was 45 (39 - 54). The hospital mortality rate was 51.9%. Driving pressure was independently associated with hospital mortality (odds ratio 1.21, 95%CI 1.04 - 1.41 for each cm H2O increase in driving pressure, p = 0.01). Based on a double stratification analysis, we found that for the same level of tidal volume/kg predicted body weight, the risk of hospital death increased with increasing driving pressure. However, changes in tidal volume/kg predicted body weight were not associated with mortality when they did not lead to an increase in driving pressure.
In patients with acute respiratory distress syndrome caused by COVID-19, exposure to higher driving pressure, as opposed to higher tidal volume/kg predicted body weight, is associated with greater mortality. These results suggest that driving pressure might be a primary target for lung-protective mechanical ventilation in these patients.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):144-152
DOI 10.5935/0103-507X.20180028
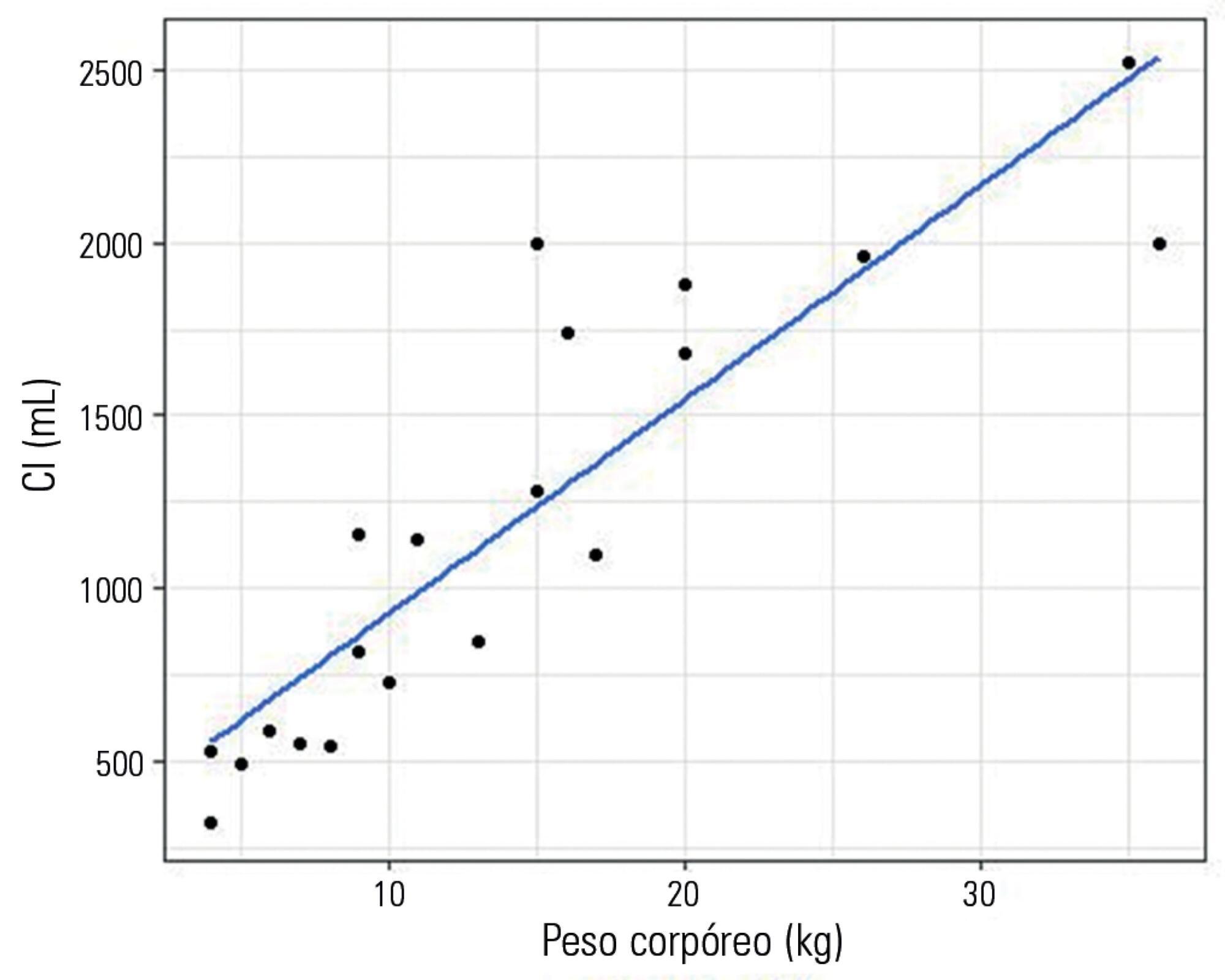
To evaluate a novel physiological approach for setting the tidal volume in mechanical ventilation according to inspiratory capacity, and to determine if it results in an appropriate mechanical and gas exchange measurements in healthy and critically ill dogs.
Twenty healthy animals were included in the study to assess the tidal volume expressed as a percentage of inspiratory capacity. For inspiratory capacity measurement, the mechanical ventilator was set as follows: pressure control mode with 35cmH2O of inspired pressure and zero end-expiratory pressure for 5 seconds. Subsequently, the animals were randomized into four groups and ventilated with a tidal volume corresponding to the different percentages of inspiratory capacity. Subsequently, ten critically ill dogs were studied.
Healthy dogs ventilated with a tidal volume of 17% of the inspiratory capacity showed normal respiratory mechanics and presented expected PaCO2 values more frequently than the other groups. The respiratory system and transpulmonary driving pressure were significantly higher among the critically ill dogs but below 15 cmH2O in all cases.
The tidal volume based on the inspiratory capacity of each animal has proven to be a useful and simple tool when setting ventilator parameters. A similar approach should also be evaluated in other species, including human beings, if we consider the potential limitations of tidal volume titration based on the calculated ideal body weight.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):212-218
DOI 10.1590/S0103-507X2009000200015
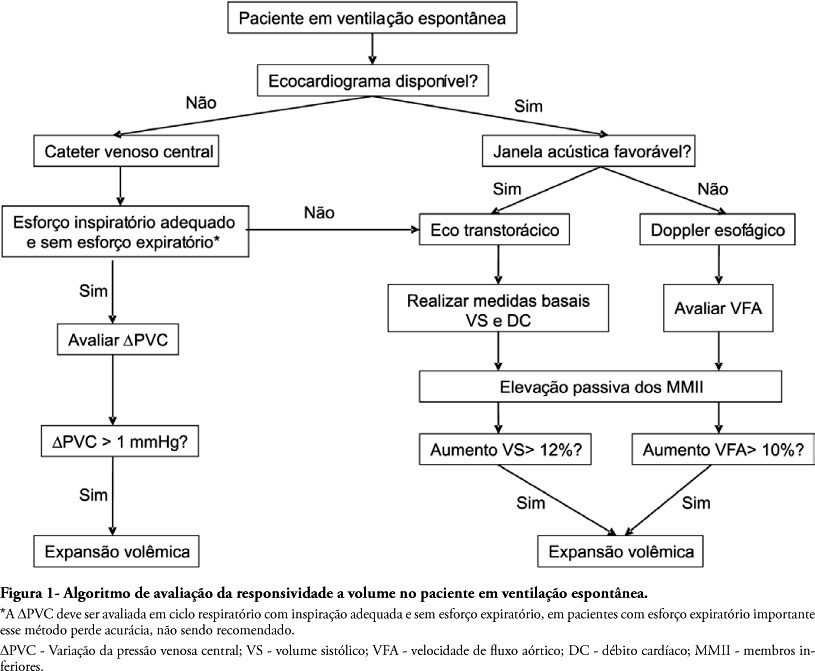
To assess fluid responsiveness in patients under spontaneous breathing activity ventilation remains a challenge for intensive care physicians. Much of the knowledge on heart-lung interactions and dynamic indexes of fluid responsiveness may not be useful for these patients. Historically, the most frequently used variables to guide fluid responsiveness on this population have been the static preload indexes. However, more recently, dynamic indexes from less invasive devices are being often used, even though their usefulness on spontaneously-breathing subjects remains controversial. The purpose of this article was to review evidences on the assessment of fluid responsiveness in patients under spontaneous ventilation. A search in literature showed poor evidence for use of static variables, such as filling pressures and ventricular end-diastolic volumes. Dynamic indexes, such as pulse pressure variation and other indexes had not been appropriately tested during spontaneous ventilation. Favorable results were found with central venous pressure variation and with transthoracic echocardiography or transesophageal Doppler dynamic indexes, especially when associated to passive lower limb elevation. We conclude that although central venous pressure variation and echocardiography variables could aid bedside clinicians in assessing fluid responsiveness during spontaneous ventilation, more studies on this subject are definitely required.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):254-260
DOI 10.1590/S0103-507X2008000300008
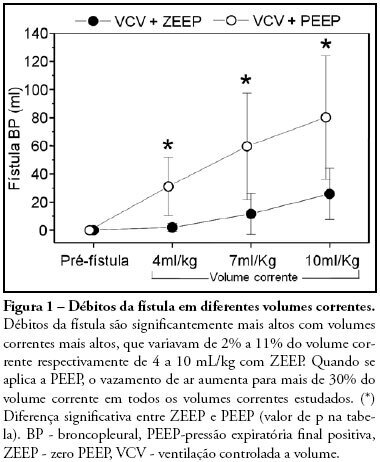
OBJECTIVES: The present study was designed to identify the effect of positive end expiratory pressure (PEEP) and the ideal pulmonary tidal volume to ventilate animals with a surgically produced bronchopleural fistula, aiming to reduce fistula output without affecting gas exchange. METHODS: Hemodynamic and respiratory assessment of gas exchange was obtained in five, healthy, young, mechanically ventilated Large White pigs under volume controlled ventilation with FiO2 of 0.4 and an inspiration:expiration ratio of 1:2, keeping respiratory rate at 22 cpm. A bronchopleural fistula was produced by resection of the lingula. Underwater seal drainage was installed and the thorax was hermetically closed. Gas exchange and fistula output were measured with the animals ventilated sequentially with tidal volumes of 4 ml/kg, 7 ml/kg and 10 ml/Kg alternating zero of positive end expiratory pressure (ZEEP) and PEEP of 10 cmH2O, always in the same order. RESULTS: These findings are attributed to reduced alveolar ventilation and ventilation/perfusion abnormalities and were attenuated with larger tidal volumes. PEEP increases air leak, even with low volume (of 2.0 ± 2.8mL to 31 ± 20.7mL; p= 0.006) and decreases alveolar ventilation in all tidal volumes. Alveolar ventilation improved with larger tidal volumes, but increased fistula output (10 mL/kg - 25.8 ± 18.3mL to 80.2 ± 43.9mL; p=0.0010). Low tidal volumes result in hypercapnia (ZEEP - Toneloto MGC, Terzi RGG, Silva WA, Moraes AC, Moreira MM 83.7± 6.9 mmHg and with PEEP 10 - 93 ± 10.1mmHg) and severely decreased arterial oxygen saturation, about of 84%. CONCLUSIONS: The tidal volume of 7 ml/Kg with ZEEP was considered the best tidal volume because, despite moderate hypercapnia, arterial oxygen saturation is sustained around 90%, alveolar ventilation improves and the fistula output is reduced when compared with a tidal volume of 10ml/Kg. A low tidal volume results in hypercapnia and severe desaturation. Finally, at any tidal volume, PEEP increases the fistula leak and decreases alveolar ventilation.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):126-130
DOI 10.1590/S0103-507X2006000200004
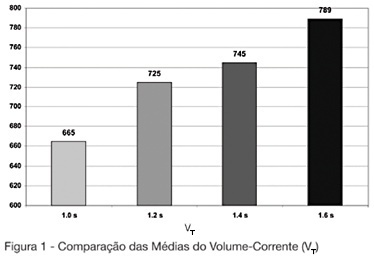
BACKGROUND AND OBJECTIVES: The mechanical ventilator support is one of the main used modalities of support in intensive therapy. In the modality of predetermined pressure, the maximum pressure is regulated, but the current volume (V T) is a complex function of the applied pressure and its speed to reach the pressure-target, of the available breathing time and the resistance to the breath. This paper has as objective to evaluate the influences of the increment of the breathing time in the pulmonary ventilation. METHODS: The study was carried through in the Adult ICU of the Regional Hospital of Mato Grosso do Sul, located in Campo Grande. They had been enclosed individuals adult, both genders, between 16 and 84 years, submitted to the mechanical ventilation in controlled pressure mode or in controlled-watched mode. The breathing time was adjusted in 1 sec, developing in 0.2 sec until the boundary-value of 1.6 sec. The tidal volume (V T) and the volume minute (V E) had been evaluated of 13 patients in the breathing times of 1s; 1.2s; 1.4s and 1.6s. RESULTS: In the mean of V T and V E an increasing increase was observed after-increment of the breathing time. We did not find in consulted literature, data which correlated the breathing time with alterations in the current volume. CONCLUSIONS: The increment of the breathing time in the ventilation for pressure control can have influence in the determination of the current volume offered to the patient.