Abstract
Rev Bras Ter Intensiva. 2012;24(1):35-42
DOI 10.1590/S0103-507X2012000100006
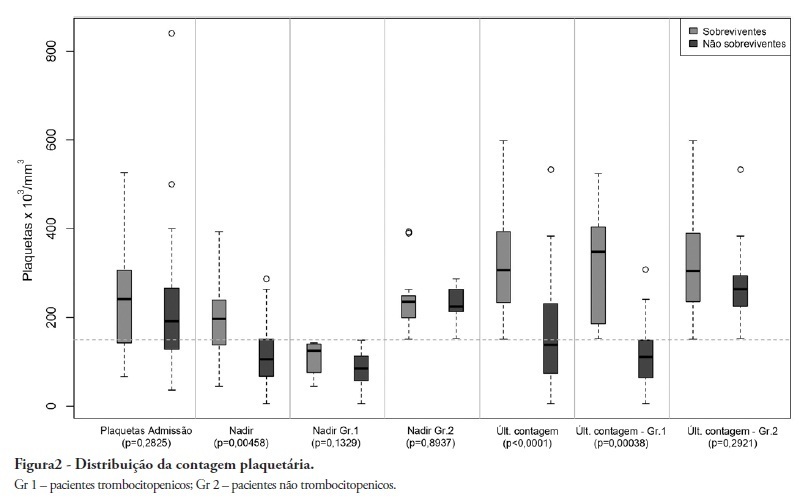
OBJECTIVE: To demonstrate an association between thrombocytopenia and platelet behavior in predicting mortality in septic patients. METHODS: Patients with criteria for sepsis at admission or at any time during hospitalization were selected; patients hospitalized for less than 24 hours were excluded. Thrombocytopenia was defined as a platelet count lower than 150.000/mm³, and recovery was defined as returning to levels above 150.000/mm³ after showing thrombocytopenia. We assessed the admission prognosis variables (APACHE II), platelet counts during the hospitalization and outcomes. RESULTS: Of the 56 patients included, 34 developed thrombocytopenia during sepsis (Group 1) and had a 76.4% mortality rate. The mortality rate among patients not showing thrombocytopenia (Group 2) was 40.9% (RR 1.87; 95% CI 1.12 - 3.12; p = 0.0163). In 44.1% of Group 1 patients, the platelet counts drops by >50% compared with the admission counts; 93.3% of these patients eventually died (RR 1.48; 95% CI 0.93 - 2.36; p = 0.0528). Among the Group 1 patients showing recovered platelet counts, 53.3% survived; 100% of the patients with unrecovered thrombocytopenia died (RR 2.14; 95% CI 1.35 - 3.39; p = 0.0003). Among the patients with APACHE II scores > 22, the thrombocytopenic patients had an 81.8% mortality rate (p = 0.25), while no deaths occurred among the non-thrombocytopenic patients. For the patients with APACHE II scores ≤ 22, the mortality rate of the thrombocytopenic patients was 74% (p = 0.0741), versus 42.8% for the non-thrombocytopenic patients. CONCLUSION: For this sample of septic patients, thrombocytopenia and its progression, defined as a >50% drop or failure to recover platelet count, were shown to be markers of poor prognosis.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):297-303
DOI 10.1590/S0103-507X2011000300007
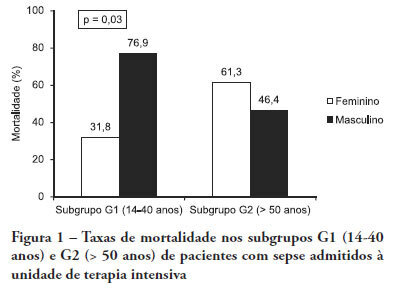
OBJECTIVE: Comparative assessment of the mortality rates of two septic patients' ages and/or gender subgroups, admitted to the intensive care unit of a university hospital. METHODS: From December 2005 to April 2008, from a total of 628 patients, 133 were admitted to the intensive care unit with sepsis and included into two age subgroups: (G1) 14 - 40 years old and (G2) more than 50 years old. Patients aged between 41 and 50 years old (n = 8) were excluded. Demographic data, prognostic indicators (APACHE II score, organ dysfunction and circulatory shock) and outcome (mortality) were analyzed. RESULTS: Of the G1 patients (n = 44), 27 were female (61.4%), and in G2 (n = 81), 40 were female (49.4%). For both groups, mean APACHE II scores, multi-organ dysfunction and progression to circulatory shock rates were not significantly different between female and male patients. For G1, overall mortality rate was lower in female than in male patients (P = 0.04), while for G2, the opposite trend was observed. CONCLUSIONS: In this sample, reproductive age female patients younger than 40 years old showed lower mortality rates compared with age-matched male patients; for patients older than 50 years old, male patients had lower mortality rates than female patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):304-311
DOI 10.1590/S0103-507X2011000300008
OBJECTIVES: Ascending aortic dissection has a poor prognosis if it is not promptly corrected surgically. Even with surgical correction, postoperative management is feared because of its complicated course. Our aim was to describe the incidence of postoperative complications and identify the 1 and 6-month mortality rate of our ascending aortic dissection surgical cohort. Secondarily, a comparison was made between ascending aortic dissection patients and paired-matched patients who received urgent coronary artery bypass graft surgery. METHODS: A retrospective analysis of a prospectively-collected database from February 2005 through June 2008 revealed 12 ascending aortic dissection and 10 elective ascending aortic aneurysm repair patients. These patients were analyzed for demographic and perioperative characteristics. Ascending aortic dissection patients were compared to paired-matched coronary artery bypass graft surgery patients according to age (± 3 years), gender, elective/urgent procedure and surgical team. The main outcome was in-hospital morbidity, defined by postoperative complications, intensive care unit admission and hospital length of stay. RESULTS: Twenty-two patients received operations to correct ascending aortic dissections and ascending aortic aneurysms, while 246 patients received coronary artery bypass graft surgeries. Ascending aortic dissection patients were notably similar to ascending aortic aneurysm brackets, except for longer mechanical ventilation times and lengths of stay in the hospital. After matching coronary artery bypass graft surgery patients to an ascending aortic dissection group, the following significantly worse results were found for the Aorta group: higher incidence of postoperative complications (91% vs. 45%, p=0.03), and longer hospital length of stay (19 [11-41] vs. 12.5 [8.5-13] days, p=0.05). No difference in mortality was found at the 1-month (8.3%) or 6-month (16.6%) postoperative care date. CONCLUSION: Ascending aortic dissection correction is associated with an increased incidence of postoperative complications and an increased hospital length of stay, but 1 and 6-month mortality is similar to that of paired-matched coronary artery bypass graft surgery patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):87-95
DOI 10.1590/S0103-507X2011000100014
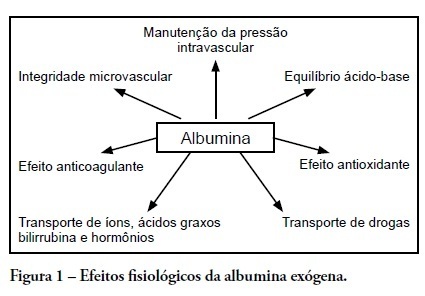
Human albumin has been used as a therapeutic agent in intensive care units for more than 50 years. However, clinical studies from the late 1990s described possible harmful effects in critically ill patients. These studies' controversial results followed other randomized controlled studies and meta-analyses that showed no harmful effects of this colloid solution. In Brazil, several public and private hospitals comply with the Agência Nacional de Vigilância Sanitária (the Brazilian Health Surveillance Agency) recommendations for appropriate administration of intravenous albumin. This review discusses indications for albumin administration in critically ill patients and analyzes the evidence for metabolic and immunomodulatory effects of this colloid solution. We also describe the most significant studies from 1998 to the present time; these reveal an absence of incremental mortality from intravenous albumin administration as compared to crystalloid solutions. The National Health Surveillance Agency indications are discussed relative to the current body of evidence for albumin use in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):229-235
DOI 10.1590/S0103-507X2010000300003
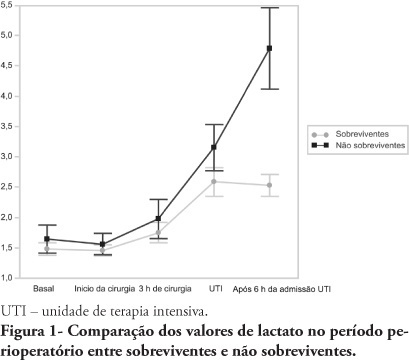
OBJECTIVES: An increased lactate level is classically considered a marker for poorer prognosis, however little information is available on intraoperative lactate's kinetics and its connection with prognosis. This study aimed to evaluate the time when perioperative lactate is most relevant for prognosis. METHODS: This was an observational prospective study conducted in a tertiary hospital. Patients with requested intensive care unit postoperative stay, aged > 18 years, undergoing major surgery were included. Palliative surgery patients and those with heart and/or severe liver failure were excluded. Arterial lactate levels were measured immediately before the surgery start (T0), after anesthesia induction (T1), 3 hours after the surgery start (T2), intensive care unit admission (T3) and 6 hours after the intensive care unit admission (T4). RESULTS: Sixty seven patients were included. The mean lactate values for the patients' T0, T1, T2 and T4 were 1.5 ± 0.8 mmol/L, 1.5 ± 0.7 mmol/L, 1.8 ± 1.2 mmol/L, 2.7 ± 1.7 mmol/L and 3.1 ± 2.0 mmol/L, respectively. The hospital mortality rate was 25.8%, and surviving and non-surviving patients lactate values in the intensive care unit were 2.5 ± 1. and 4.8 ± 2.8 mmol/L (P < 0.0001), respectively. The other times measurements showed no statistically significant differences between the groups. CONCLUSIONS: In surgical patients, intraoperative arterial lactate levels failed to show a predictive value; however during the postoperative period, this assessment was shown to be useful for hospital mortality prediction.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):133-137
DOI 10.1590/S0103-507X2010000200006
STUDY OBJECTIVE: Obese patients seem to have worse outcomes and more complications during intensive care unit (ICU) stay. This study describes the clinical course, complications and prognostic factors of obese patients admitted to an intensive care unit compared to a control group of nonobese patients. DESIGN: Retrospective observational study. SETTING: A 10-bed adult intensive care unit in a university-affiliated hospital. METHODS: All patients admitted to the intensive care unit over 52 months (April 01/2005 to November 30/2008) were included. Obese patients were defined as those with a body mass index (BMI) ≥ 30 Kg/M2. Demographic and intensive care unit related data were also collected. An clinical and demographical matching group of eutrophic patients selected from the data base as comparator for mortality and morbidity outcomes. The Mann-Whitney test was used for numeric data comparisons and the Chi Square test for categorical data comparisons. RESULTS: Two hundred nineteen patients were included. The obese group (n=73) was compared to the eutrophic group (n= 146). Most of this group BMI ranged between 30 - 35 Kg/M2. Only ten patients had body mass index ≥40 Kg/M2. Significant differences between the obese and eutrophic groups were observed in median APACHE II score (16 versus 12, respectively; p<0.05) and median intensive care unit length of stay (7 versus 5 days respectively; p<0,05). No significant differences were seen regarding risk of death, mortality rate, mechanical ventilation needs, days free of mechanical ventilation and tracheostomy rates. The observed mortality was higher than the APACHE II-predicted for both groups, but the larger differences were seen for morbid obese patients (BMI ≥40 Kg/M2). CONCLUSIONS: Obesity did not increase the mortality rate, but improved intensive care unit length of stay. The current prognostic scoring systems do not include BMI, possibly underestimating the risk of death, and other quality of care indexes in obese patients. New studies could be useful to clarify how body mass index impacts the mortality rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):138-143
DOI 10.1590/S0103-507X2010000200007
BACKGROUND: The elderly population is increasing all over the world. The need of intensive care by the elderly is also increasing. There is a lack of studies investigating the risk factors for death among critically ill elderly patients. This study aims to investigate the factors associated with death in a population of critically ill elderly patients admitted to an intensive care unit in Brazil. METHODS: This is a retrospective cohort study including all elderly patients (>60 years) admitted to an intensive care unit in Fortaleza, Brazil, from January to December 2007. A comparison between survivors and nonsurvivors was done and the risk factors for death were investigated through univariate and multivariate analysis. RESULTS: A total of 84 patients were included, with an average age of 73 ± 7.6 years; 59% were female. Mortality was 62.8%. The main cause of death was multiple organ dysfunction (42.3%), followed by septic shock (36.5%) and cardiogenic shock (9.7%). Complications during intensive care unit ICU stay associated with death were respiratory failure (OR=61, p<0.001), acute kidney injury (OR=23, p<0.001), sepsis (OR=12, p<0.001), metabolic acidosis (OR=17, p<0.001), anemia (OR=8.6, p<0.005), coagulation disturbance (OR=5.9, p<0.001) and atrial fibrillation (OR=4.8, p<0.041). Independent risk factors for death were age (OR=1.15, p<0.005), coma (OR=7.51, p<0.003), hypotension (OR=21.75, p=0.003), respiratory failure (OR=9.93, p<0.0001) and acute kidney injury (OR=16.28, p<0.014). CONCLUSION: Mortality is high among critically ill elderly patients. Factors associated with death were age, coma, hypotension, respiratory failure and acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):11-18
DOI 10.1590/S0103-507X2010000100004
OBJECTIVE: This study aimed to evaluate the outcome of cirrhotic patients admitted to Intensive Care Unit. METHODS: We conducted a prospective cohort of cirrhotic patients admitted to two intensive care unit between June 1999 to September 2004. We collected demographic, comorbid conditions, diagnosis, vital signs, laboratory data, prognostic scores and evolution in intensive care unit and hospital. The patients were divided in groups: non surgical, non liver surgery, surgery for portal hypertension, liver surgery, liver transplantation, and urgent surgery. RESULTS: We studied 304 patients, which 190 (62.5%) were male. The median of age was 54 (47-61) years. The mortality rate in intensive care unit and hospital were 29.3 and 39.8%, respectively, more elevated than in the other patients admitted critically ill patients (19.6 and 28.3%; p<0.001). Non surgical patients and those submitted to urgent surgery presented high mortality rate in the intensive care unit (64.3 and 65.4%) and in the hospital (80.4 and 76.9%). The variables related to hospital mortality were [Odds ratio (confidence interval 95%)]: mean arterial pressure [0.985 (0.974-0.997)]; mechanical ventilation in the first 24 h [4.080 (1.990-8.364)]; confirmed infection in the first 24 h [7.899 (2.814-22.175)]; acute renal failure [5.509 (1.708-17.766)] and APACHE II score (points) [1.078 (1.017-1.143)]. CONCLUSIONS: Cirrhotic patients had higher mortality rate compared to non cirrhotic critically ill patients. Those admitted after urgent surgery and non surgical had higher mortality rate.