Abstract
Rev Bras Ter Intensiva. 2009;21(4):359-368
DOI 10.1590/S0103-507X2009000400005
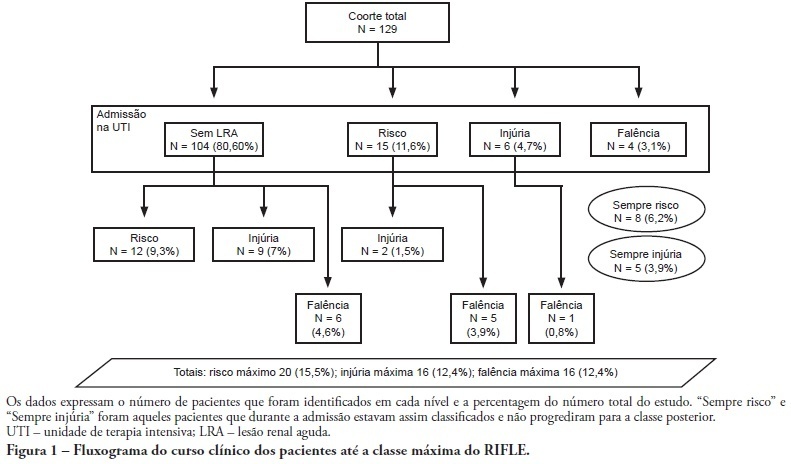
OBJECTIVE: To correlate the RIFLE classification with mortality and length of stay both in the intensive care unit and hospital. METHODS: A prospective, observational, longitudinal cohort study, approved by the Institution's Ethics Committee. Data were collected for all patients staying longer than 24 hours in the intensive care unit of Hospital Universitário Polydoro Ernani de São Thiago - Universidade Federal de Santa Catarina from September 2007 to March 2008, followed-up either until discharge or death. Patients were divided in two groups: with or without acute kidney injury. The acute kidney injury group was additionally divided according to the RIFLE and sub-divided according to the maximal score in Risk, Injury of Failure. Loss and End-stage classes were not included in the study. APACHE II and SOFA were also evaluated. The t Student and Chi-Square tests were used. A P<0.05 was considered statistically significant. RESULTS: The sample included 129 patients, 52 (40.3%) with acute kidney injury according to RIFLE. Patients were more severely ill in this group, with higher APACHE and SOFA scores (P<0.05). Compared to the without kidney injury group, the kidney injury severity caused increased intensive care unity (Risk 25%; Injury 37.5%; Failure 62.5%) and in-hospital (Risk 50%; Injury 37.5%; Failure 62.5%) mortality, and longer intensive care unit stay (P<0.05). CONCLUSION: The RIFLE system, according to the severity class, was a marker for risk of increased intensive care unit and in-hospital mortality, and longer intensive care unit stay. No relationship with in-hospital length of stay was found.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):391-397
DOI 10.1590/S0103-507X2009000400009
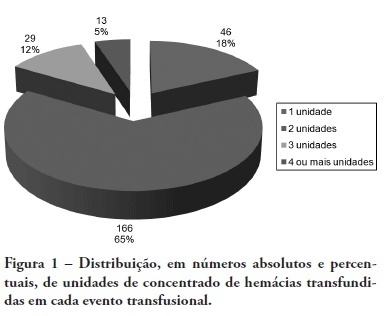
BACKGROUND: The anemia is a common problem upon admission of the patients in the intensive care unit being the red blood cell transfusion a frequent therapeutic. The causes of anemia in critical patients who under go red blood cell transfusion are several: acute loss of blood after trauma, gastrointestinal hemorrhage, surgery amongst others. Currently, few studies are available regarding the use of blood components in patients at intensive care unit. Although blood transfusions are frequent in intensive care unit, the optimized criteria for handling are not clearly defined, with no available guidelines. OBJECTIVES: To analyze the clinical indications of the use of the red blood cell in the intensive care unit. METHODS: The clinical history of the patients admitted in the intensive care unit were analyzed, revisiting which had have red blood cell transfusion in the period between January 1st 2005 and December 31 2005. The study was accepted by the Research Ethics Committee - Comitê de Ética em Pesquisa (CEP) - of the University of South of Santa Catarina (UNISUL). RESULTS: The transfusion rate was 19,33, and the majority of the patients were of the male gender. Their age prevalence was of 60 years old or older. The mortality rate among patients who under went red blood cell transfusion died was of 38,22%. The transfusions criterias were low serum hemoglobin (78%) and the hemoglobin pre - transfusion was 8,11 g/dL. CONCLUSIONS: Politrauma and sepsis/sepsis chock were the pre diagnosis criteria. A low hemoglobin level is the main clinical criteria with average hemoglobin pre - transfusion was 8,11 g/dL.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):453-460
DOI 10.1590/S0103-507X2009000400017
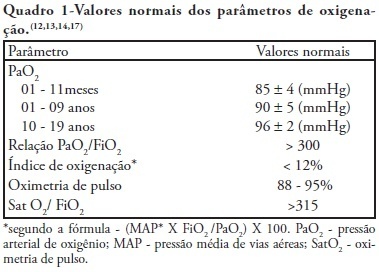
Recent changes were introduced in acute hypoxemic respiratory failure children ventilation methods. There are evidences that less aggressive ventilation strategies can improve severe pulmonary injury survival. Experimental trials evidenced a relationship between inappropriate ventilatory measures and delayed acute pulmonary injury improvement, or even worsening. From this, a protective ventilatory measure arises in combination with alveolar recruitment maneuver. This association is believed in clinical practice to determine importantly reduced morbidity and mortality as well as reduced mechanic ventilation-induced injuries. It is indicated for acute lung injury patients, generally from pneumonia or sepsis, with severe hypoxemia. Its main contraindications are homodynamic instability, pneumothorax and intracranial hypertension. Experimental trials showed beneficial maneuver effects on both oxygenation and alveolar collapse. Adult studies showed improved pulmonary function with hypoxemia reversion. In children, the maneuver lead to significant inspired oxygen fraction and alveolar collapse reductions, less oxygen dependency, improved pulmonary complacency, and reduced bronchopulmonary dysplasia. However, studies in children are limited. Additional investigation is warranted on this matter, and its clinical application evidence. A literature review was conducted based on textbooks and MEDLINE, Pubmed, Cochrane library, SciELO, and Ovid databases, from 1998 to 2009, both in Portuguese and English. Publications on alveolar recruitment maneuver both in adults and children, review articles, experimental and clinical trials were included using the key words: protective ventilatory strategy, alveolar recruitment maneuver, pediatrics and mechanic ventilation.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):255-261
DOI 10.1590/S0103-507X2009000300004
Currently, aging of the population is a widespread global phenomenon. Therefore, the assessment of prognosis in elderly patients is needed. This study aims to identify risk factors in a population of elderly patients admitted in the intensive care unit METHODS: A prospective study in the intensive care unit of a general tertiary hospital was carried out for five months. Patients with 65 years or more of age, who stayed in the intensive care unit for 24 hours or more were included and those at the-end-of-life, patients readmitted to intensive care unit during the same hospital stay were excluded. RESULTS: In this study 199 patients were involved, with a mean age of 75.4±6.8 years, and 58.8% were female. Mortality was 57.3%. The mean APACHE II, SOFA, MODS and Katz index (assessment of daily activities) were respectively 20.0±5.8, 6.8±3.9, 2.4±1.9 and 5.3±1.6. Most patients were postoperative 59.3% and 41.6% were under invasive mechanical ventilation. At regression analysis, the independent determinants of higher mortality were: older age (76.9±6.7 years death versus 73.3±6.5 years discharge, P<0.001, OR=1.08, CI 95% 1.01-1. 16), the Katz index (4.9±1.9 deaths versus 5.7±0.9 discharge, p=0.001, OR=0.66, CI 95% 0.45-0.98), hyperglycemia (158.1±69.0 death versus 139.6±48.5 discharge p=0.041; OR=1.02; CI 95% 1.01-1.03) and need for mechanical ventilation at admission to the intensive care unit (57.0% death versus 20.5% discharge p <0.001, OR=3.57, CI 95% 1.24-10.3). CONCLUSION: Elderly patients admitted to the intensive care unit that have difficulties in performing daily activities, hyperglycemia and who are under invasive mechanical ventilation had a worse hospital prognosis.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):262-268
DOI 10.1590/S0103-507X2009000300005
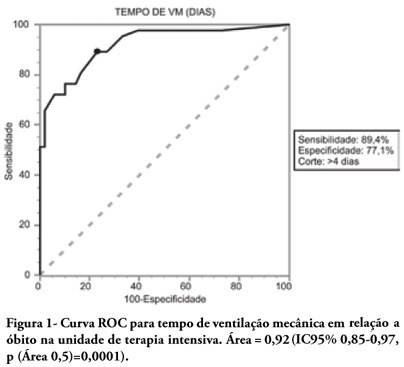
OBJECTIVES: To describe the population of aged as compared to young patients under mechanical ventilation and to analyze the mortality risk factors of this group in an intensive care unit. METHODS: This was a prospective observational trial in patients over 18 years of age, admitted in an intensive care unit and under mechanical ventilation, during one year. Patients were divided into two groups according to age: Group 1 - patients over 65 years old; and Group 2, 65 years old or younger. RESULTS: eighty one mechanic ventilation patients were included, 62 aged and 18 younger, mean ages from aged was 76 years, while in the younger it was 56 years. As compared to the control, aged patients had longer mechanic ventilation time , higher intensive care unit and hospital mortality: 63.1% versus 26.3% and 74.2% versus 47.4% (P<0.05), respectively. In addition, the aged under mechanic ventilation had increased desintubation failures, difficult ventilatory weaning and deaths directly related to respiratory dysfunction. The mechanic ventilation time was an independent risk factor for death in the intensive care unit in aged patients (OR= 2.7, p=0.02). The area under the ROC curve of mechanic ventilation about intensive care unit death was 0.92 (95% CI 0.85-0.97, p (area 0.5)=0.0001), cutoff point of 4 days, sensitivity 89.4% and specificity 77.1%. CONCLUSIONS: Mechanic ventilation patients over 65years of age have a worse prognosis than the younger, and the longer the mechanic ventilation time, the higher will be intensive care mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):306-309
DOI 10.1590/S0103-507X2009000300011
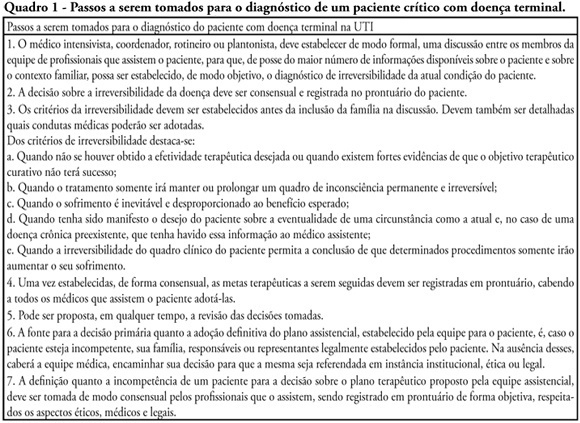
Withholding of treatment in patients with terminal disease is increasingly common in intensive care units, throughout the world. Notwithstanding, Brazilian intensivists still have a great difficulty to offer the best treatment to patients that have not benefited from curative care. The objective of this comment is to suggest an algorithm for the care of terminally ill patients. It was formulated based upon literature and the experience of experts, by members of the ethics committee and end-of-life of AMIB - Brazilian Association of Intensive Care.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):231-236
DOI 10.1590/S0103-507X2009000300001
OBJECTIVE: This study aimed to analyze outcome, clinical and epidemiological characteristics and severity factors in adult patients admitted with a diagnosis of infection by virus A (H1N1) to public and private intensive care units, in Paraná, Brazil. METHODS: Cohort study of medical charts of patients older than 12 years admitted to 11 intensive care units in 6 cities in the state of Parana, Brazil, during a period of 45 days, with diagnosis of swine influenza. The diagnosis of infection with A (H1N1) was made by real time polymerase chain reaction (RT-PCR) of nasopharyngeal secretion, or strong clinical suspicion when other causes had been ruled out (even with negative RT-PCR). Descriptive statistics were performed, analysis by the Chi square test was used to compare percentages and the Student's t test for continuous variables with univariate analysis, assuming a significance level of p <0.05. RESULTS: There were 63 adult patients admitted with a diagnosis of H1N1, 37 (58.7%) being RT-PCR positive. Most patients were young adults (65% under 40 years of age) with no gender predominance and high incidence of obesity (27.0% with Body Mass Index > 30). Mean of the Acute Physiologic Chronic Health Evaluation II (APACHE II) score was 15.0 + 8.1. Mortality in the intensive care unit was 39.7%. The main factors associated with mortality were: positive RT-PCR, low levels of initial PaO2/FiO2, high initial levels of urea and lactate dehydrogenase, required level of positive end expiratory pressure, need for the prone position and vasopressors. CONCLUSIONS: Adult patients with A (H1N1) virus infection admitted to intensive care units had a high risk of death, particularly due to respiratory impairment. Positive RT-PCR, urea and lactic dehydrogenase, low initial PaO2/FiO2 and high levels of PEEP were correlated with higher mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):247-254
DOI 10.1590/S0103-507X2009000300003
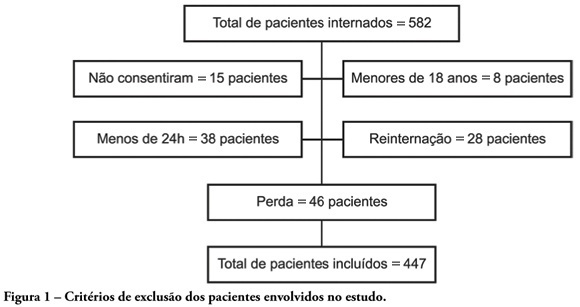
OBJECTIVES: Availability of state-of-the-art technology at intensive care units has often turned into a tool aggravating suffering by prolonging the end-of-life process. Distinguishing therapeutic persistence from therapeutic obstinacy has become a great challenge for present-day medicine. The aim of this study was to assess the benefit-harm relation in the use of life-sustaining therapies by means of an evolutionary system of individual prognostic assessment. METHODS: A cohort, prospective, observational study at the intensive care unit of the São Francisco De Paula University Hospital of UCPel, Pelotas RS from March 2006 to August 31, 2007. Individual prognostic assessments were recorded by using an evolutionary system, the UNICAMP II index, associated with albumin transferrin and lymphocytes serum levels, life- sustaining therapies and the outcome. Statistical analysis was carried out by the Student's t-test, ANOVA test, Chi-square test, Fisher's exact test, Spearman's correlation test and area under the receiver-operating characteristic curve. A p value < 0.05 was considered statistically significant. RESULTS: Four hundred forty seven patients were assessed during the study. Prevalence of death was significantly higher among those who received life-sustaining therapies at a later stage of the intervention, and those whose prognostic index and nutritional status worsened at an early stage of intervention. CONCLUSION: Assessment of individual evolutionary prognostic proved to be a useful method to objectively subsidize ethical decisions related to therapeutic persistence and therapeutic obstinacy.