Abstract
Rev Bras Ter Intensiva. 2010;22(2):144-152
DOI 10.1590/S0103-507X2010000200008
OBJECTIVE: To know and compare the patterns of antimicrobials use in intensive care units (ICUs) based on the Anatomical Therapeutic Chemical/Defined Daily Dose (ATC/DDD) system. METHODS: a prospective cohort study was conducted in three medical-surgical intensive care units, two of them in public hospitals and one in a private hospital. Simple random, independent samples of patients admitted from 10/2004 to 09/2005 to the selected intensive care units were used. The antibiotics use was assessed using the ATC/DDD system. The amount of antibacterials used in each intensive care unit, in grams, was transformed in daily defined dose (DDD). The number of DDDs was divided by the number of patient-days, multiplied by one thousand, to obtain the average density of consumption (DC) per thousand patient-days (DDD1000). RESULTS: 1,728 patients-days and 2,918.6 DDDs were examined in the three intensive care units, corresponding to an average density of consumption of 1,689.0 DDD1000. The median number of DDDs of antibiotics use in the public hospitals’ intensive care units was significantly higher (p=0.002) versus the private hospital’s intensive care unit. The consumption of antibiotics in the private hospital’s intensive care unit (DC=2,191.7 DDD1000) was significantly higher (p<0.001) versus the intensive care units of public hospitals (1,499.5 DDD1000). The most used antibiotics groups in the three intensive care units were 3rd generation cephalosporins, penicillins/betalactamases inhibitors, carbapenems and fluorquinolones. CONCLUSION: The pattern of antibiotics use in the three examined intensive care units was not uniform. The private hospital’s intensive care unit used a significantly larger amount versus the public hospitals’ intensive care units. Nevertheless, the most used antibiotics groups were similar in the three intensive care units.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):112-117
DOI 10.1590/S0103-507X2010000200003
OBJECTIVES: Communication issues between healthcare professionals in intensive care units may be related to critically ill patients’ increased mortality. This study aimed to evaluate if communication issues involving assistant physicians and routine intensive care unit physicians would impact critically ill patients’ morbidity and mortality. METHODS: This was a cohort study that included non-consecutive patients admitted to the intensive care unit for 18 months. The patients were categorized in 3 groups according to their assistant doctors’ versus routine doctors communication uses: DC - daily communication during the stay (>75% of the days); EC - eventual communication (25 to 75% of the days); RC - rare communication (< 25% of the days). Demographic data, severity scores, reason for admission to the intensive care unit and interventions were recorded. The consequences of the medical professionals communication failures (delayed procedures, diagnostic tests, antibiotics, ventilatory weaning, vasopressors) and medical prescriptions inadequacies (no bed head elevation, no stress ulceration and deep venous thrombosis drug prophylaxis), and their relationship with the patients outcomes were analyzed. RESULTS: 792 patients were included, and categorized as follows: DC (n=529); EC (n=187) and RC (n=76). The mortality was increased in the RC patients group (26.3%) versus the remainder groups (DC = 13.6% and EC = 17.1%; p<0.05). A multivariate analysis showed that delayed antibiotics [RR 1.83 (CI95%: 1.36 -2.25)], delayed ventilatory weaning [RR 1.63 (CI95%: 1.25-2.04)] and no deep venous thrombosis prophylaxis [RR 1.98 (CI95%: 1.43 - 3.12)] contributed independently for the increased mortality. CONCLUSION: The failure in the assistant and routine intensive care doctors communication may increase the patients’ mortality, particularly due to delayed antibiotics and ventilation weaning, and lack of deep venous thrombosis prophylaxis prescription.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):133-137
DOI 10.1590/S0103-507X2010000200006
STUDY OBJECTIVE: Obese patients seem to have worse outcomes and more complications during intensive care unit (ICU) stay. This study describes the clinical course, complications and prognostic factors of obese patients admitted to an intensive care unit compared to a control group of nonobese patients. DESIGN: Retrospective observational study. SETTING: A 10-bed adult intensive care unit in a university-affiliated hospital. METHODS: All patients admitted to the intensive care unit over 52 months (April 01/2005 to November 30/2008) were included. Obese patients were defined as those with a body mass index (BMI) ≥ 30 Kg/M2. Demographic and intensive care unit related data were also collected. An clinical and demographical matching group of eutrophic patients selected from the data base as comparator for mortality and morbidity outcomes. The Mann-Whitney test was used for numeric data comparisons and the Chi Square test for categorical data comparisons. RESULTS: Two hundred nineteen patients were included. The obese group (n=73) was compared to the eutrophic group (n= 146). Most of this group BMI ranged between 30 - 35 Kg/M2. Only ten patients had body mass index ≥40 Kg/M2. Significant differences between the obese and eutrophic groups were observed in median APACHE II score (16 versus 12, respectively; p<0.05) and median intensive care unit length of stay (7 versus 5 days respectively; p<0,05). No significant differences were seen regarding risk of death, mortality rate, mechanical ventilation needs, days free of mechanical ventilation and tracheostomy rates. The observed mortality was higher than the APACHE II-predicted for both groups, but the larger differences were seen for morbid obese patients (BMI ≥40 Kg/M2). CONCLUSIONS: Obesity did not increase the mortality rate, but improved intensive care unit length of stay. The current prognostic scoring systems do not include BMI, possibly underestimating the risk of death, and other quality of care indexes in obese patients. New studies could be useful to clarify how body mass index impacts the mortality rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):138-143
DOI 10.1590/S0103-507X2010000200007
BACKGROUND: The elderly population is increasing all over the world. The need of intensive care by the elderly is also increasing. There is a lack of studies investigating the risk factors for death among critically ill elderly patients. This study aims to investigate the factors associated with death in a population of critically ill elderly patients admitted to an intensive care unit in Brazil. METHODS: This is a retrospective cohort study including all elderly patients (>60 years) admitted to an intensive care unit in Fortaleza, Brazil, from January to December 2007. A comparison between survivors and nonsurvivors was done and the risk factors for death were investigated through univariate and multivariate analysis. RESULTS: A total of 84 patients were included, with an average age of 73 ± 7.6 years; 59% were female. Mortality was 62.8%. The main cause of death was multiple organ dysfunction (42.3%), followed by septic shock (36.5%) and cardiogenic shock (9.7%). Complications during intensive care unit ICU stay associated with death were respiratory failure (OR=61, p<0.001), acute kidney injury (OR=23, p<0.001), sepsis (OR=12, p<0.001), metabolic acidosis (OR=17, p<0.001), anemia (OR=8.6, p<0.005), coagulation disturbance (OR=5.9, p<0.001) and atrial fibrillation (OR=4.8, p<0.041). Independent risk factors for death were age (OR=1.15, p<0.005), coma (OR=7.51, p<0.003), hypotension (OR=21.75, p=0.003), respiratory failure (OR=9.93, p<0.0001) and acute kidney injury (OR=16.28, p<0.014). CONCLUSION: Mortality is high among critically ill elderly patients. Factors associated with death were age, coma, hypotension, respiratory failure and acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):11-18
DOI 10.1590/S0103-507X2010000100004
OBJECTIVE: This study aimed to evaluate the outcome of cirrhotic patients admitted to Intensive Care Unit. METHODS: We conducted a prospective cohort of cirrhotic patients admitted to two intensive care unit between June 1999 to September 2004. We collected demographic, comorbid conditions, diagnosis, vital signs, laboratory data, prognostic scores and evolution in intensive care unit and hospital. The patients were divided in groups: non surgical, non liver surgery, surgery for portal hypertension, liver surgery, liver transplantation, and urgent surgery. RESULTS: We studied 304 patients, which 190 (62.5%) were male. The median of age was 54 (47-61) years. The mortality rate in intensive care unit and hospital were 29.3 and 39.8%, respectively, more elevated than in the other patients admitted critically ill patients (19.6 and 28.3%; p<0.001). Non surgical patients and those submitted to urgent surgery presented high mortality rate in the intensive care unit (64.3 and 65.4%) and in the hospital (80.4 and 76.9%). The variables related to hospital mortality were [Odds ratio (confidence interval 95%)]: mean arterial pressure [0.985 (0.974-0.997)]; mechanical ventilation in the first 24 h [4.080 (1.990-8.364)]; confirmed infection in the first 24 h [7.899 (2.814-22.175)]; acute renal failure [5.509 (1.708-17.766)] and APACHE II score (points) [1.078 (1.017-1.143)]. CONCLUSIONS: Cirrhotic patients had higher mortality rate compared to non cirrhotic critically ill patients. Those admitted after urgent surgery and non surgical had higher mortality rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):19-26
DOI 10.1590/S0103-507X2010000100005
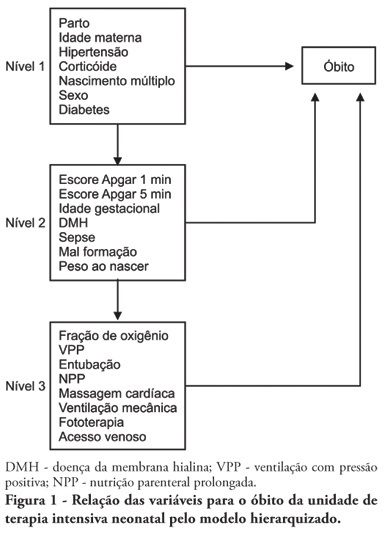
OBJECTIVE: To identify risk factors associated with death of infants admitted to neonatal intensive care unit of Taubaté University Hospital. METHODS: It is a longitudinal study with information obtained from medical records of newborns admitted to the neonatal intensive care unit of Taubaté University Hospital. Type of outcome, discharge or death, was dependent variable. The independent variables were maternal and gestational variables: maternal age, hypertension, diabetes, corticosteroid therapy and delivery; variables of the newborn: birth weight, gestation length, Apgar score in the first and fifth minutes of life, multiple birth, congenital malformations and sex; hospitalar variables: report of mechanical ventilation, positive pressure ventilation, reports of prolonged parenteral nutrition, sepsis, intubation, cardiac massage, phototherapy, hyaline membrane disease, oxygen and fraction of inspired oxygen. It was built a model in three hierarchical levels for the survival analysis by the Cox model; it was used the software Stata v9 and the final model contained variables with p <0.05. The risks were estimated by measure effect known as hazard ratio (HR) with confidence intervals of 95%. The newborns transferred during hospitalization to another service were excluded from the study. RESULTS: There were admitted during the study period 495 newborns, with 129 deaths (26.1%). In the final model, only the variables of steroid use (HR 1.64, 95% CI 1.02-2.70), malformation (HR 1.93, CI 95% 1,05-2,88), very low birth weight (HR 4.28, 95% CI 2,79-6,57) and Apgar scores lower than seven of no1 min (HR 1.87, 95% CI 1,19-2,93) and 5 min (HR 1.74, 95% CI 1,05-2,88) and the variables phototherapy (HR 0.34; 95% CI 0,22-0,53) and endotracheal intubation (HR 2.28, 95% CI 1 .41-3, 70). CONCLUSION: Factors related primarily to the newborn and the hospitalar internment (except therapy with corticosteroids) were identified as associated to mortality highlighting a possible protective factor of phototherapy and the risk of infants with very low birth weight.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):33-39
DOI 10.1590/S0103-507X2010000100007
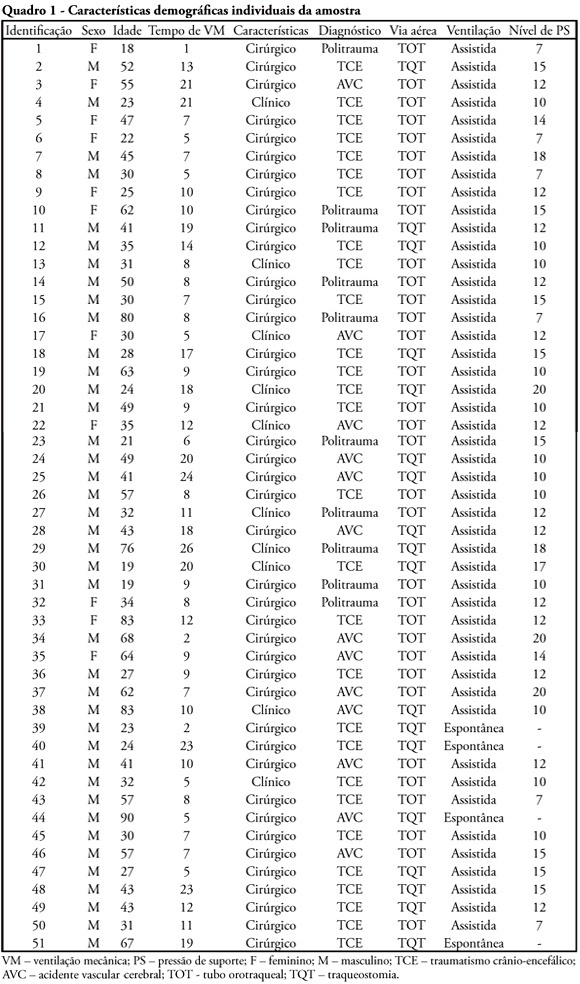
OBJECTIVE: To verify if the maximal inspiratory pressure values with 40 seconds occlusion time are greater than with the 20 seconds occlusion time, and the impacts on the following patient's physiological variables: respiratory rate, pulse oxygen saturation, heart rate and blood pressure, before and after the measurements. METHODS: This was a transversal prospective randomized study. Fifty-one patients underwent maximal inspiratory pressure measurement, measured by one single investigator. The manometer was calibrated before each measurement, and then connected to the adapter and this to the unidirectional valve inspiratory branch for 20 or 40 seconds. RESULTS: The values with 40 seconds occlusion (57.6 ± 23.4 cmH2O) were significantly higher than the measurements taken with 20 seconds occlusion (40.5 ± 23.4 cmH2O; p=0.0001). The variables changes between the before and after measurement respiratory and hemodynamic parameters monitoring showed: heart rate variation for the 20 seconds occlusion 5.13 ± 8.56 beats per minute and after 40 seconds occlusion 7.94 ± 12.05 beats per minute (p = 0.053), versus baseline. The mean blood pressure change for 20 seconds occlusion was 9.29 ± 13.35 mmHg and for 40 seconds occlusion 15.52 ± 2.91 mmHg (p=0.021). The oxygen saturation change for 20 seconds occlusion was 1.66 ± 12.66%, and for 40 seconds 4.21 ± 5.53% (p=0.0001). The respiratory rate change for 20 seconds occlusion was 6.68 ± 12.66 movements per minute and for 40 seconds 6.94 ± 6.01 (p=0.883). CONCLUSION: The measurement of maximal inspiratory pressure using a longer occlusion (40 seconds) produced higher values, without triggering clinically significant stress according to the selected variables.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):77-84
DOI 10.1590/S0103-507X2010000100013
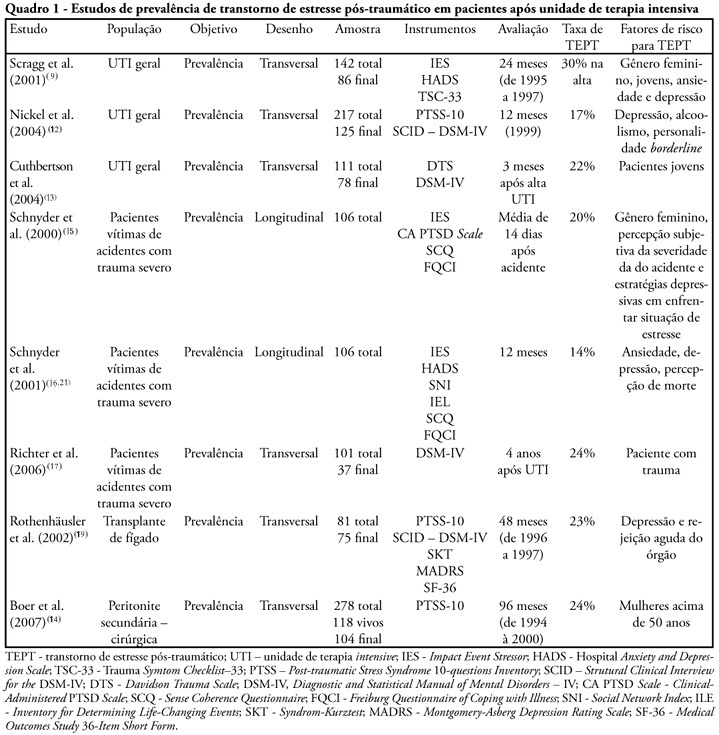
Post-traumatic stress disorder has been detected in patients after treatment in intensive care unit. The main goal of this study is to review the psychological aspects and therapeutic interventions on those patients after their treatment on intensive care unit. Thirty eight articles have been included. The prevalence of post-traumatic stress disorder has varied from 17% up to 30% and the incidence from 14% to 24%. The risk factors were: previous anxiety historic, depression or panic, having delusional traumatic memories (derived from psychic formations as dreams and delirium), belief effects, depressive behavior, stressing experiences and mechanical ventilation. High doses of opiates, symptoms caused by sedation or analgesia reduction and the use of lorazepam were related with the increase of delirium and delusional memory. The disorder sintomatology can be reduced with hydrocortisone administration, with daily sedation interruption. No other effectiveness psychological intervention study was found.