Abstract
Rev Bras Ter Intensiva. 2014;26(2):122-129
DOI 10.5935/0103-507X.20140018
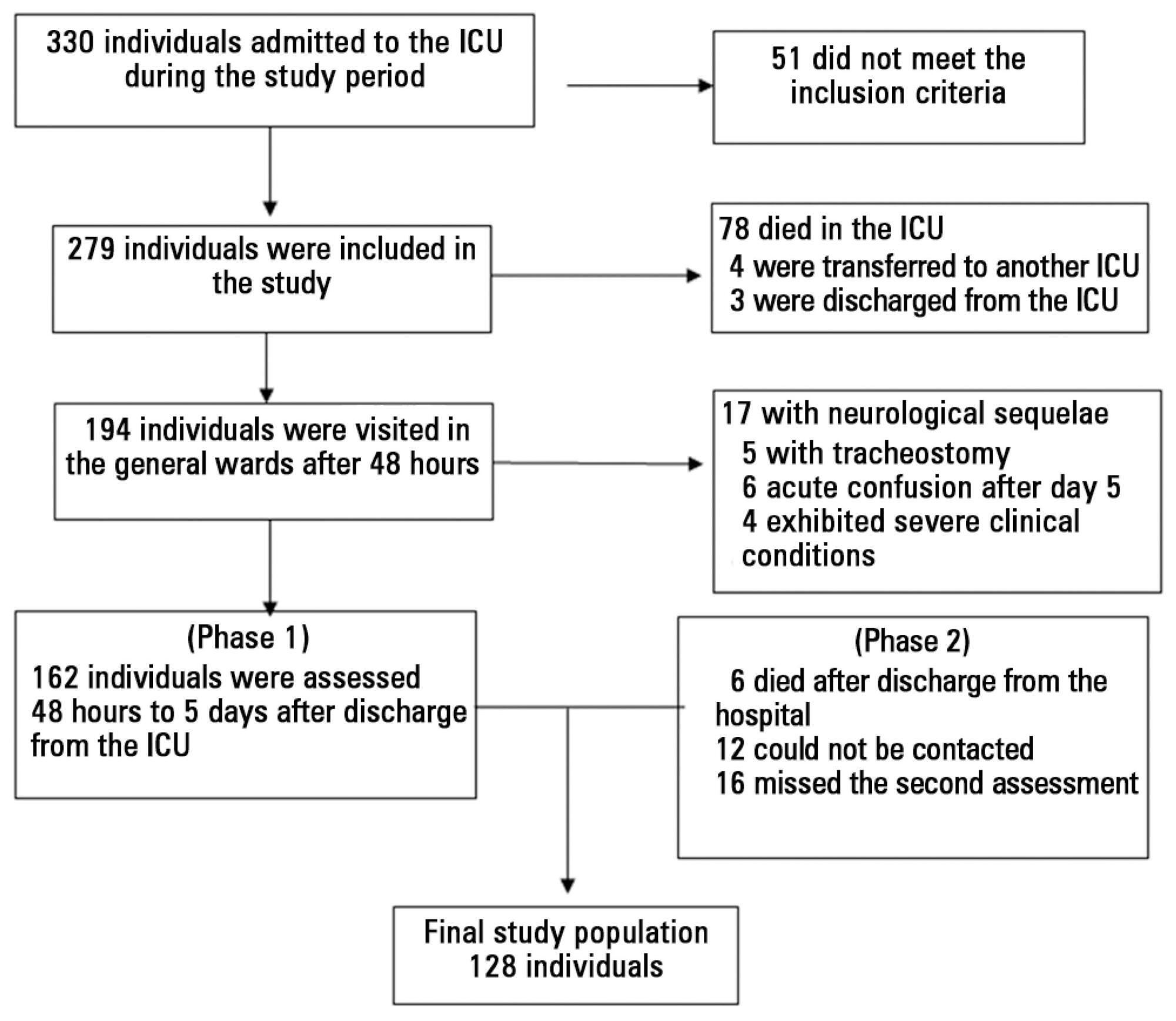
To investigate the relationship between sedation and the memories reported by patients subjected to mechanical ventilation following discharge from the intensive care unit.
This prospective, observational, cohort study was conducted with individuals subjected to mechanical ventilation who remained in the intensive care unit for more than 24 hours. Clinical statistics and sedation records were extracted from the participants' clinical records; the data relative to the participants' memories were collected using a specific validated instrument. Assessment was performed three months after discharge from the intensive care unit.
A total of 128 individuals were assessed, most of whom (84.4%) reported recollections from their stay in the intensive care unit as predominantly a combination of real and illusory events. The participants subjected to sedation (67.2%) at deep levels (Richmond Agitation-Sedation Scale [RASS] -4 and -5) for more than two days and those with psychomotor agitation (33.6%) exhibited greater susceptibility to occurrence of illusory memories (p>0.001).
The probability of the occurrence of illusory memories was greater among the participants who were subjected to deep sedation. Sedation seems to be an additional factor that contributed to the occurrence of illusory memories in severely ill individuals subjected to mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):148-154
DOI 10.5935/0103-507X.20140022
Patients with traumatic brain injury are particularly susceptible to sepsis, which may exacerbate the systemic inflammatory response and lead to organ dysfunction. The influence of clinical variables on the mortality of intensive care unit patients with traumatic brain injury and sepsis was investigated.
The present investigation was a retrospective study involving 175 patients with traumatic brain injury who were treated in a period of 1 year at a reference hospital for trauma and who had sepsis, severe sepsis, or septic shock. Demographic and clinical data were obtained, and the SOFA score was calculated at the time sepsis was found and after 72 hours.
There was a predominance of young men with severe traumatic brain injury, multiple head injuries, sepsis with a pulmonary focus, prolonged hospital stay, and high mortality (37.7%). Circulatory and respiratory failure had a high incidence, but renal and coagulation failure were less frequent, and liver failure was not observed. After logistic regression, the presence of septic shock and respiratory failure 72 hours after the sepsis diagnosis was associated with higher mortality, with an odds ratio of 7.56 (95%CI=2.04-27.31, p=0.0024) and 6.62 (95%CI=1.93-22.78, p=0.0027), respectively. In addition, there was a higher mortality among patients who had no organ failure on D1 but who developed the condition after 72 hours of sepsis and in those patients who already had organ failure at the time sepsis was diagnosed and remained in this condition after 72 hours.
Septic shock and progressive organ (particularly respiratory) dysfunction increases the mortality of patients with traumatic brain injury and sepsis.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):21-27
DOI 10.5935/0103-507X.20140004
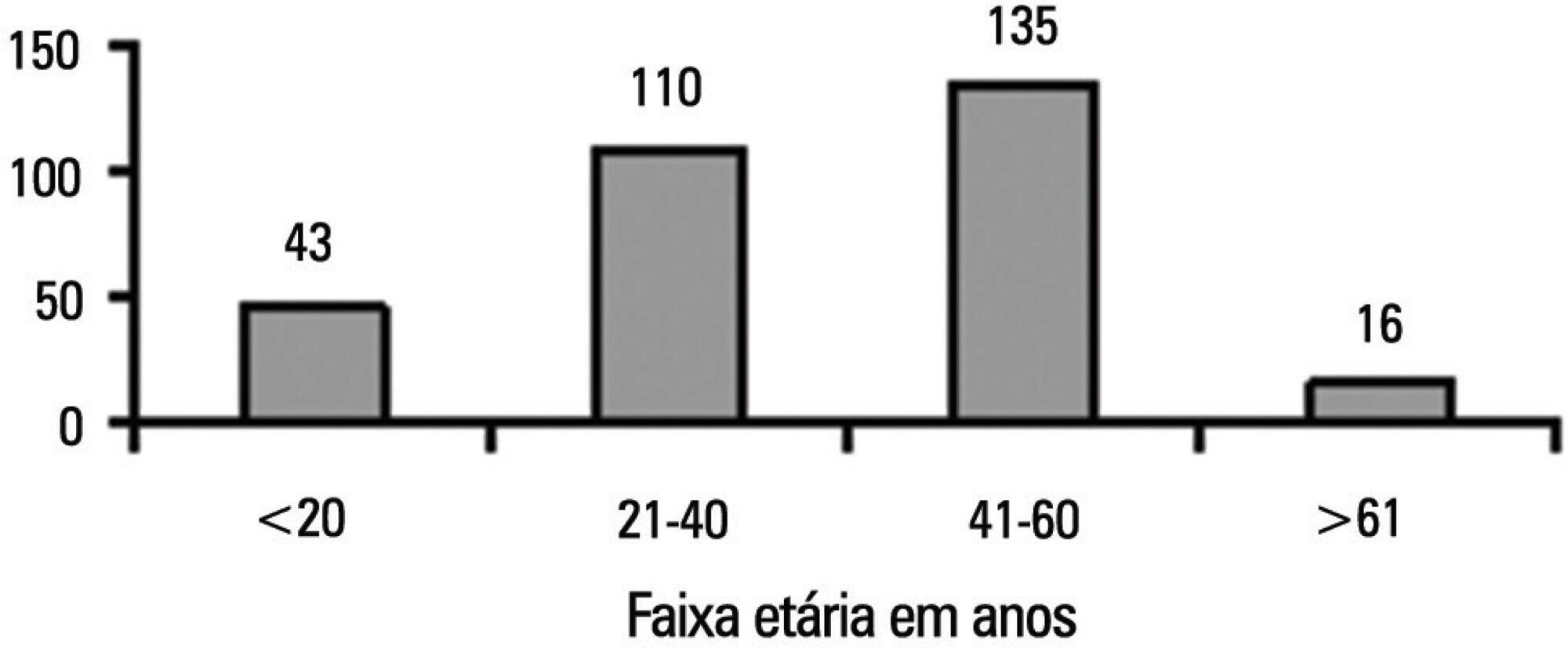
To characterize the profile of effective organ and tissue donors and to understand which organs and tissues were donated for transplantation.
This was a quantitative, descriptive, exploratory, retrospective study that analyzed clinical data from 305 donors between January 2006 to December 2010. The data were then analyzed using descriptive analyses, generating frequency tables, measures of position (mean, minimum and maximum) and measures of dispersion (standard deviation) for data that was social and clinical in nature.
There was an overall predominance of white (72%) and male (55%) individuals between the ages of 41 and 60 years (44%). The primary cause of brain death was cerebrovascular accident (55%). In the patient history, 31% of the patients were classified as overweight, 27% as hypertensive and only 4.3% as having diabetes mellitus. Vasoactive drugs were used in 92.7% of the donors, and the main drug of choice was noradrenaline (81.6%). Hyperglycemia and hypernatremia were diagnosed in 78% and 71% of the donors, respectively.
Significant hemodynamic changes were found, and the results indicate that the use of vasoactive drugs was the main strategy used to control these changes. Furthermore, most donors presented with hyperglycemia and hypernatremia, which were frequently reported in association with brain death. The persistent nature of these findings suggests that the organ donors were inadequately maintained.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):28-35
DOI 10.5935/0103-507X.20140005
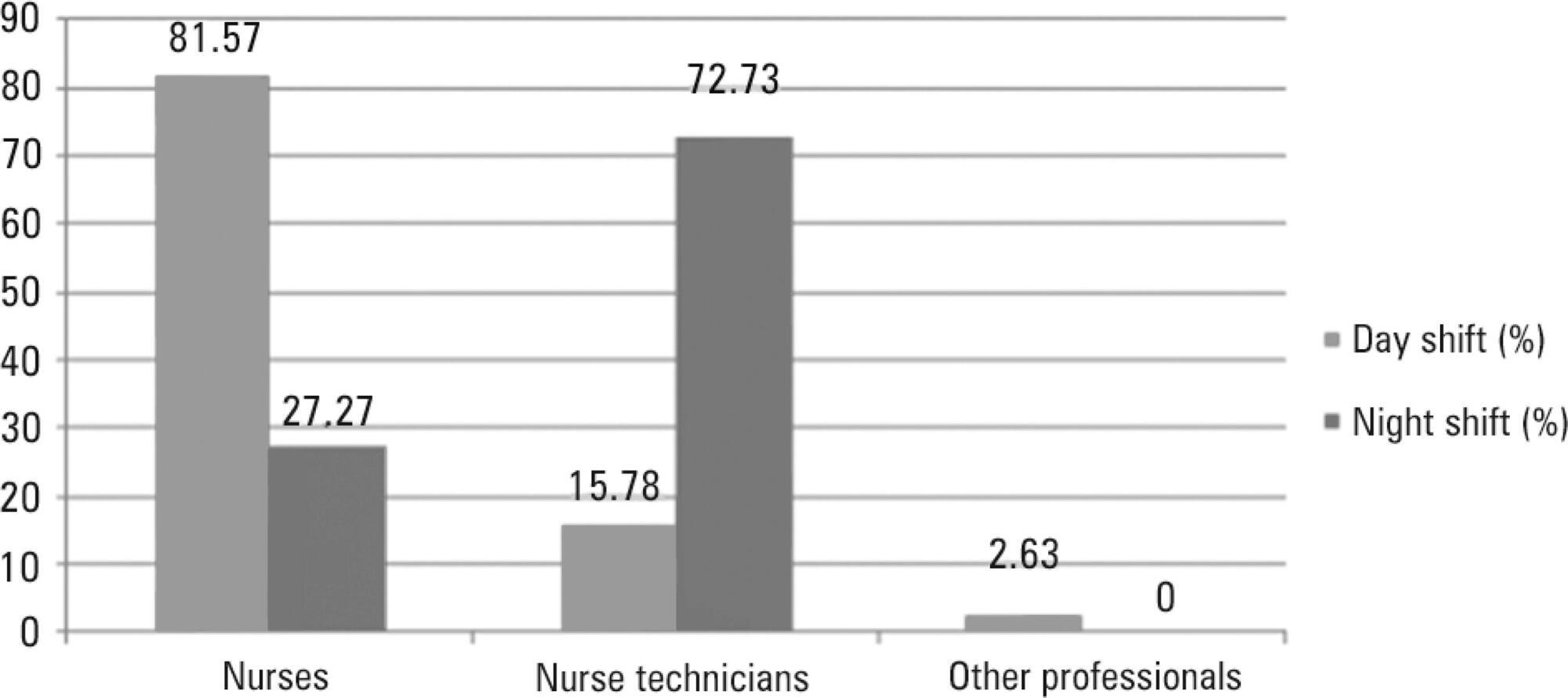
To define the characteristics and measure the reaction time of a health care team monitoring alarms in the intensive care unit.
A quantitative, observational, and descriptive study developed at the coronary care unit of a cardiology public hospital in Rio de Janeiro state (RJ). Data were obtained from the information collected on the patients, the monitoring used, and the measurement of the team's reaction time to the alarms of multi-parameter monitors during a non-participatory field observation.
Eighty-eight patients were followed (49 during the day shift and 39 during the night shift). During the 40 hours of observation (20 hours during the day shift and 20 hours during the night shift), the total number of monitoring alarms was 227, with 106 alarms during the day shift and 121 during the night shift, an average of 5.7 alarms/hour. In total, 145 alarms unanswered by the team were observed, with 68 occurring during the day shift (64.15%) and 77 during the night shift (63.64%). This study demonstrated that the reaction time was longer than 10 minutes in more than 60% of the alarms, which were considered as unanswered alarms. The median reaction time of the answered alarms was 4 minutes and 54 seconds during the day shift and 4 minutes and 55 seconds during the night shift. The respiration monitoring was activated in only nine patients (23.07%) during the night shift. Regarding the alarm quality of these variables, the arrhythmia alarm was qualified in only 10 (20.40%) of the day-shift patients and the respiration alarm in four night-shift patients (44.44%).
The programming and configuration of the physiological variables monitored and the parameters of alarms in the intensive care unit were inadequate; there was a delay and lack of response to the alarms, suggesting that relevant alarms may have been ignored by the health care team, thus compromising the patient safety.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):176-182
DOI 10.5935/0103-507X.20140026
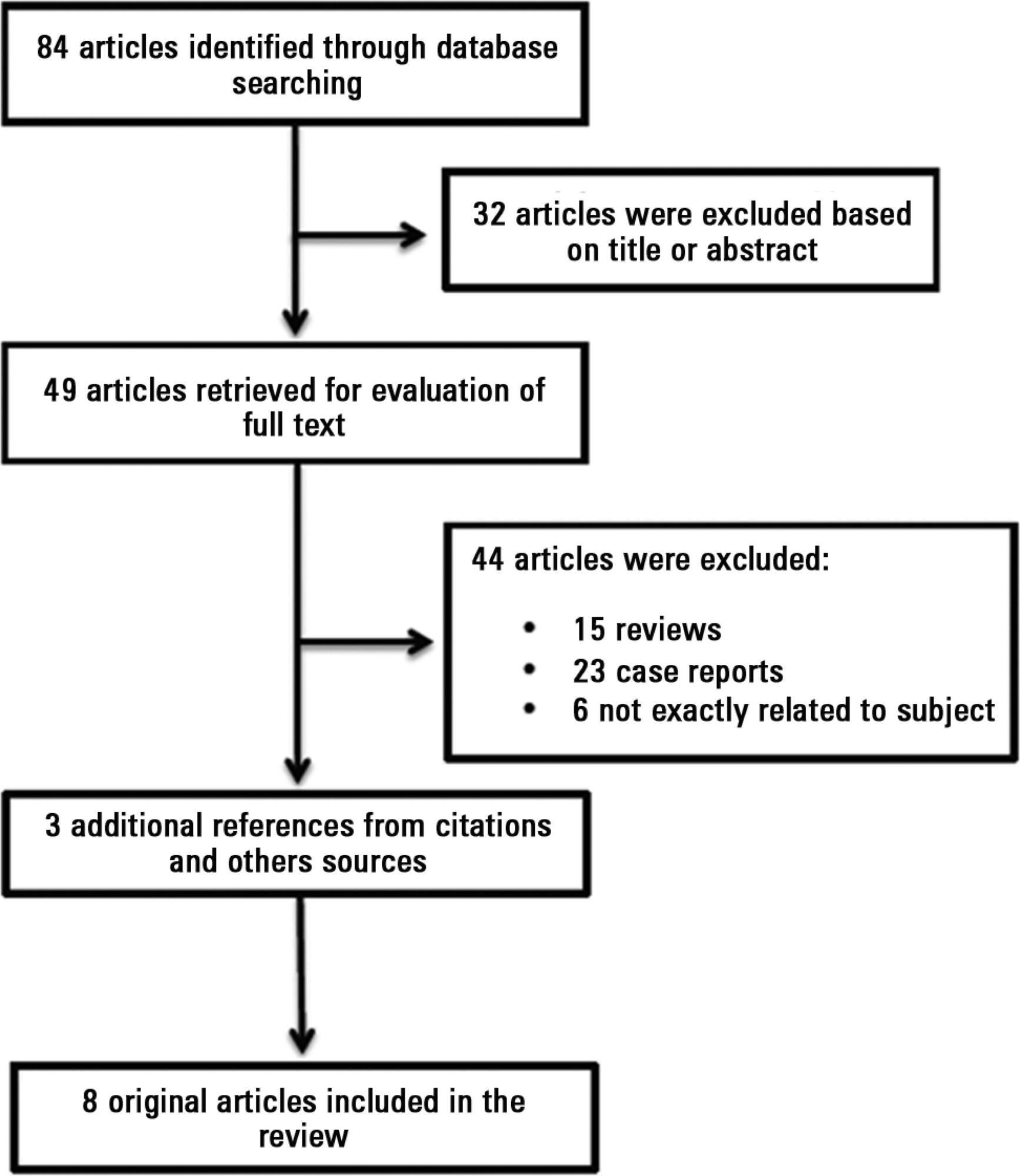
Antiphospholipid antibodies are responsible for a wide spectrum of clinical manifestations. Venous, arterial and microvascular thrombosis and severe catastrophic cases account for a large morbidly/mortality. Through the connection between the immune, inflammatory and hemostatic systems, it is possible that these antibodies may contribute to the development of organ dysfunction and are associated with poor short and long-term prognoses in critically ill patients. We performed a search of the PubMed/MedLine database for articles written during the period from January 2000 to February 2013 to evaluate the frequency of antiphospholipid antibodies in critically ill patients and their impact on the outcomes of these patients. Only eight original studies involving critically ill patients were found. However, the development of antiphospholipid antibodies in critically ill patients seems to be frequent, but more studies are necessary to clarify their pathogenic role and implications for clinical practice.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):36-43
DOI 10.5935/0103-507X.20140006
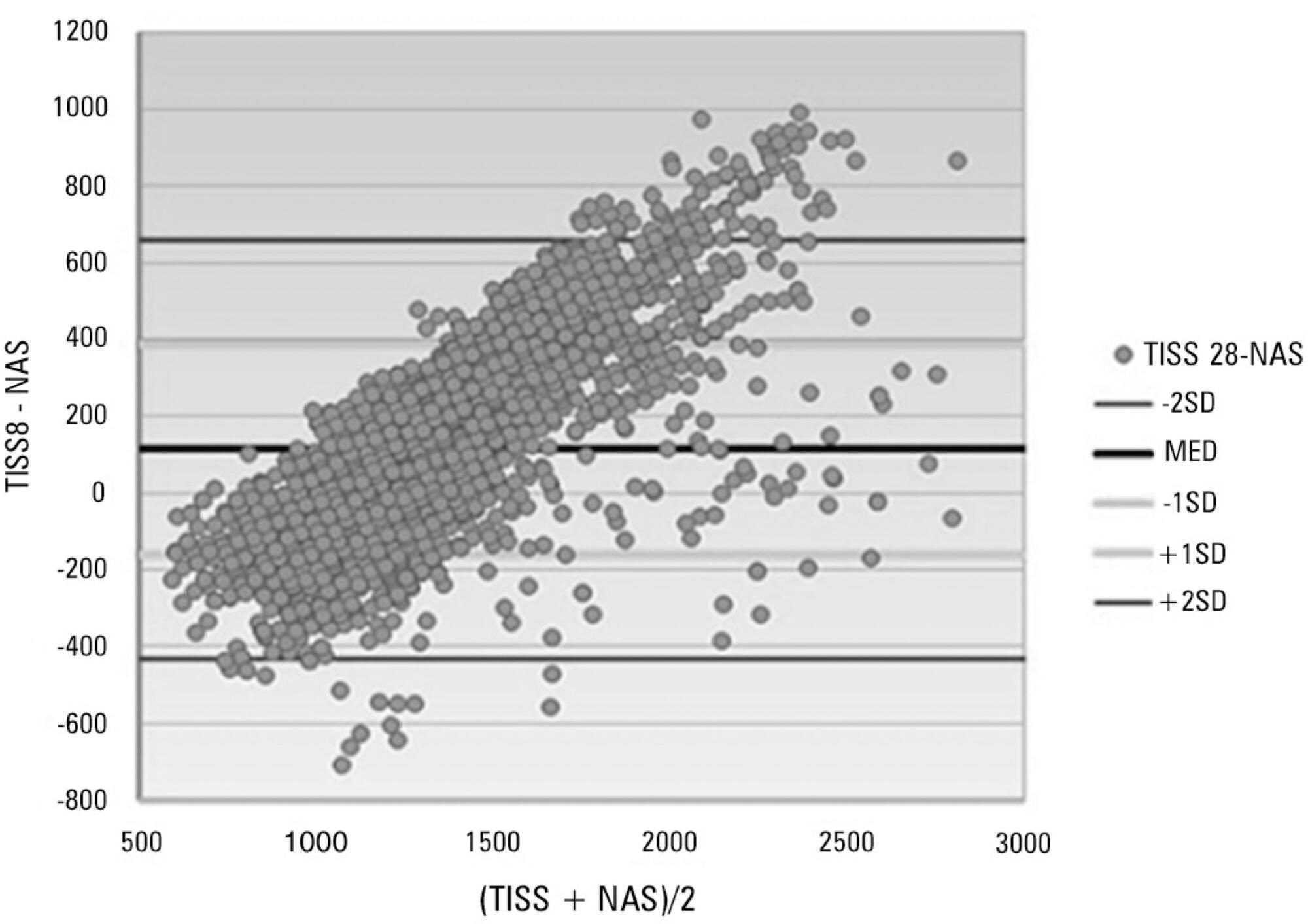
To assess the performance of the Nursing Activities Score in a pediatric intensive care unit, compare its scores expressed as time spent on nursing activities to the corresponding ones calculated using the Simplified Therapeutic Intervention Scoring System, and correlate the results obtained by both instruments with severity, morbidity and mortality.
Prospective, observational, and analytical cohort study conducted at a type III general pediatric intensive care unit. The study participants were all the children aged 29 days to 12 years admitted to the investigated pediatric intensive care unit from August 2008 to February 2009.
A total of 545 patients were studied, which corresponded to 2,951 assessments. The average score of the Simplified Therapeutic Intervention Scoring System was 28.79±10.37 (915±330 minutes), and that of the Nursing Activities Score was 55.6±11.82 (802±161 minutes). The number of minutes that resulted from the conversion of the Simplified Therapeutic Intervention Scoring System score was higher compared to that resulting from the Nursing Activities Score for all the assessments (p<0.001). The correlation between the instruments was significant, direct, positive, and moderate (R=0.564).
The agreement between the investigated instruments was satisfactory, and both instruments also exhibited satisfactory discrimination of mortality; for that purpose, the best cutoff point was 16 nursing hours/patient day.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):57-64
DOI 10.5935/0103-507X.20140009
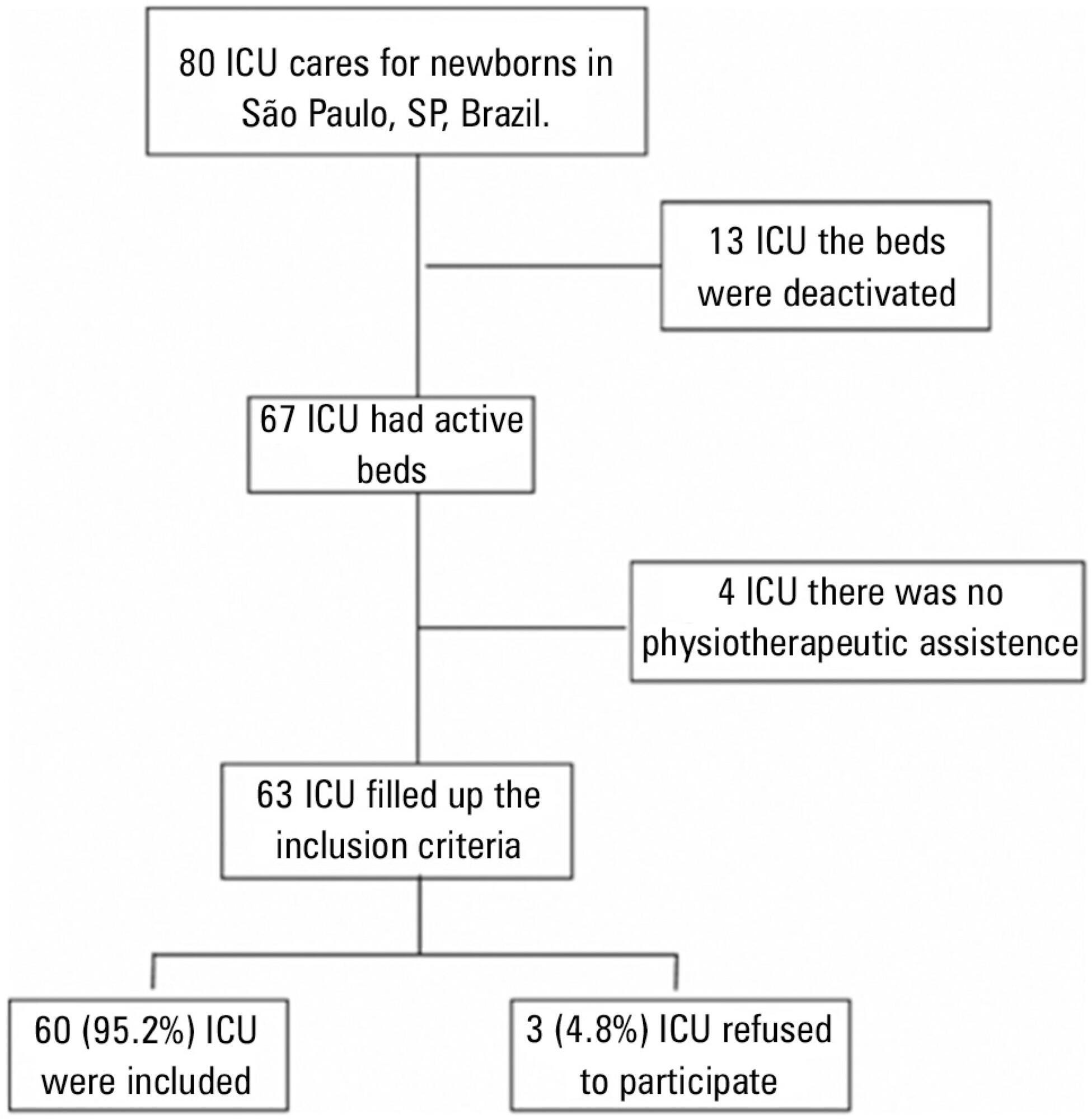
To describe the characteristics of physical therapy assistance to newborns and to provide a profile of physical therapists working in intensive care units in the city of São Paulo, Brazil.
This cross-sectional study was conducted in every hospital in São Paulo city that had at least one intensive care unit bed for newborns registered at the National Registry of Health Establishments in 2010. In each unit, three types of physical therapists were included: an executive who was responsible for the physical therapy service in that hospital (chief-physical therapists), a physical therapist who was responsible for the physical therapy assistance in the neonatal unit (reference-physical therapists), and a randomly selected physical therapist who was directly involved in the neonatal care (care-physical therapists).
Among the 67 hospitals eligible for the study, 63 (94.0%) had a physical therapy service. Of those hospitals, three (4.8%) refused to participate. Thus, 60 chief-PTs, 52 reference-physical therapists, and 44 care-physical therapists were interviewed. During day shifts, night shifts, and weekends/holidays, there were no physical therapists in 1.7%, 45.0%, and 13.3% of the intensive care units, respectively. Physical therapy assistance was available for 17.8±7.2 hours/day, and each physical therapist cared for 9.4±2.6 newborns during six working hours. Most professionals had completed at least one specialization course.
Most neonatal intensive care units in the city of São Paulo had physical therapists working on the day shift. However, other shifts had incomplete staff with less than 18 hours of available physical therapy assistance per day.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):65-70
DOI 10.5935/0103-507X.20140010
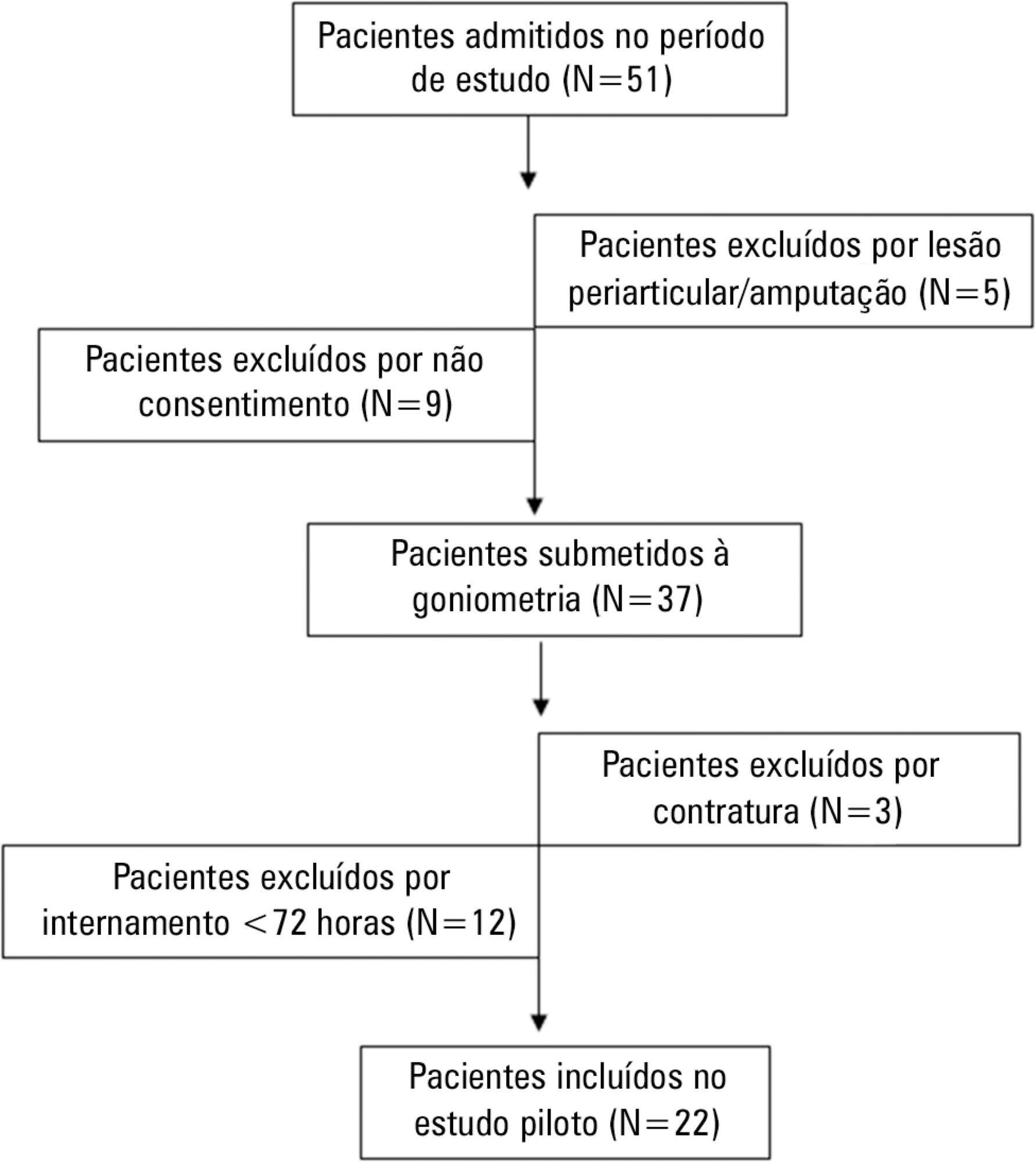
To evaluate the joint range of motion of critically ill patients during hospitalization in the intensive care unit.
This work was a prospective longitudinal study conducted in a critical care unit of a public hospital in the city of Salvador (BA) from September to November 2010. The main variable evaluated was the passive joint range of motion. A goniometer was used to measure the elbows, knees and ankles at the time of admission and at discharge. All patients admitted in the period were included other than patients with length of stay <72 hours and patients with reduced joint range of motion on admission.
The sample consisted of 22 subjects with a mean age of 53.5±17.6 years, duration of stay in the intensive care unit of 13.0±6.0 days and time on mechanical ventilation of 12.0±6.3 days. The APACHE II score was 28.5±7.3, and the majority of patients had functional independence at admission with a prior Barthel index of 88.8±19. The losses of joint range of motion were 11.1±2.1°, 11.0±2.2°, 8.4±1.7°, 9.2±1.6°, 5.8±0.9° and 5.1±1.0°, for the right and left elbows, knees and ankles, respectively (p<0.001).
There was a tendency towards decreased range of motion of large joints such as the ankle, knee and elbow during hospitalization in the intensive care unit.