Abstract
Rev Bras Ter Intensiva. 2014;26(4):430-434
DOI 10.5935/0103-507X.20140066
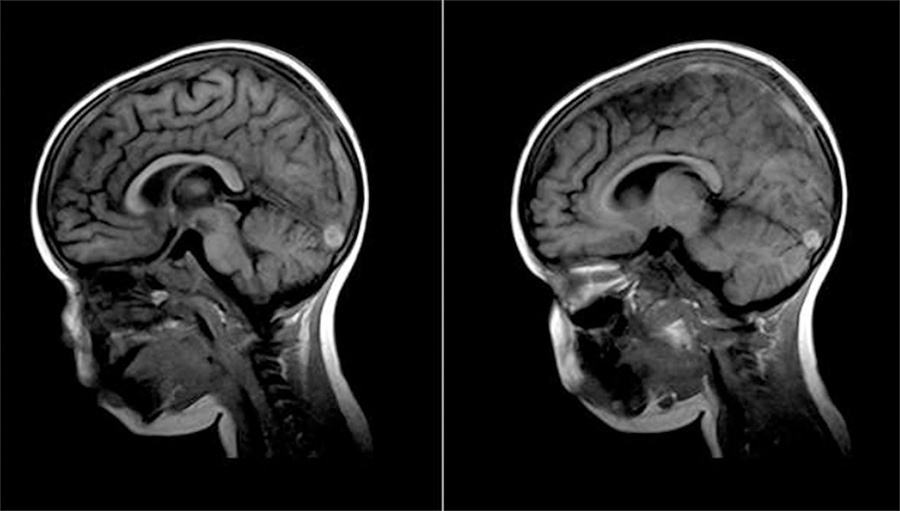
Nephrotic syndrome is associated with a hypercoagulable state and an increased risk of thromboembolic complications. Cerebral venous sinus thrombosis is a rare complication of nephrotic syndrome, with few cases described in the literature, although the disease may be under-diagnosis. The true incidence of cerebral venous sinus thrombosis may be underestimated because many events are asymptomatic or are not diagnosed in time. Here, we describe the case of a male child, 2 years and 10 months old, with nephrotic syndrome presenting with headache, epileptic seizures and sensory inhibition who was diagnosed with superior sagittal and transverse sinuses thrombosis. An international literature review was performed with a defined search strategy in the PubMed, SciELO and Lilacs databases using the terms ‘nephrotic syndrome’ and ‘cerebral sinovenous thrombosis’. The diagnosis of venous thrombosis should be considered in any patient with nephrotic syndrome who presents with neurological signs and symptoms, as early clinical diagnosis promotes favorable outcomes.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):407-414
DOI 10.1590/S0103-507X2012000400019
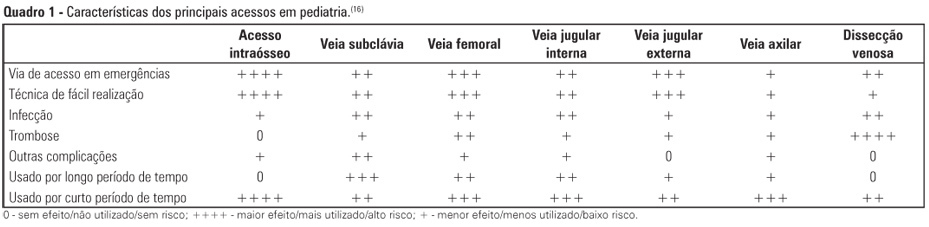
Obtaining venous access in critically ill children is an essential procedure to restore blood volume and administer drugs during pediatric emergencies. The first option for vascular access is through a peripheral vein puncture. If this route cannot be used or if a prolonged period of access is necessary, then the intraosseous route is an effective option for rapid and safe venous access. The present work is a descriptive and exploratory literature review. The study's aim was to describe the techniques, professional responsibilities, and care related to obtaining venous access via the intraosseous route in pediatric emergencies. We selected 22 articles (published between 2000 and 2011) that were available in the Latin American and Caribbean Health Sciences (LILACS) and MEDLINE databases and the SciELO electronic library, in addition to the current protocol of cardiopulmonary resuscitation from the American Heart Association (2010). After the literature search, data were pooled and grouped into the following categories of analysis: historical aspects and physiological principles; indications, benefits, and contraindications; professional assignments; technical principles; care during the access; and possible complications. The results of the present study revealed that the intraosseous route is considered the main secondary option for vascular access during the emergency response because the technique is quick and easily executed, presents several non-collapsible puncture sites, and enables the rapid and effective administration of drugs and fluid replacement.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):306-311
DOI 10.5935/0103-507X.20130052
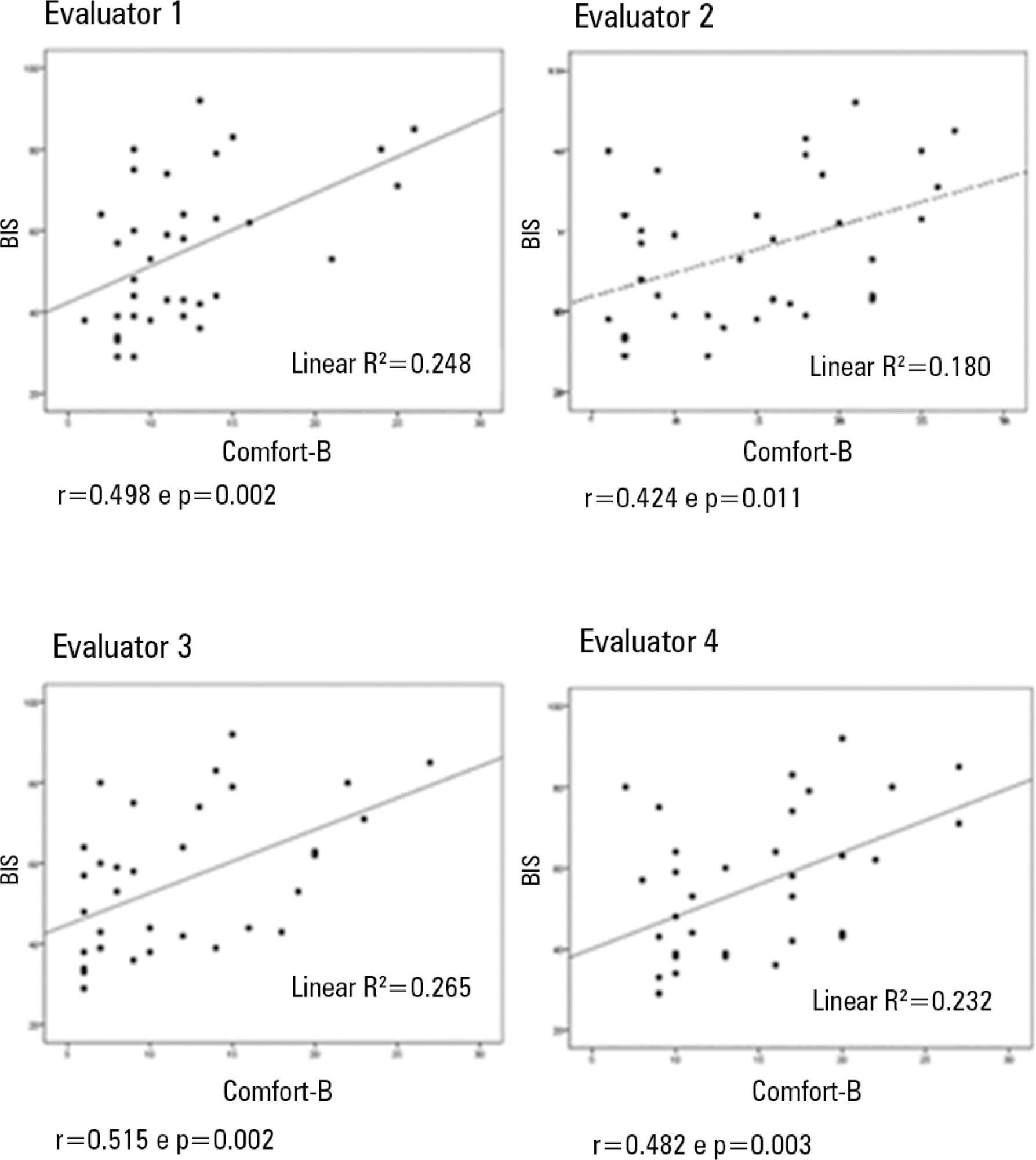
Compare the scores resulting from the Comfort-B scale with the bispectral index in children in an intensive care unit.
Eleven children between the ages of 1 month and 16 years requiring mechanical ventilation and sedation were simultaneously classified based on the bispectral index and the Comfort-B scale. Their behavior was recorded using digital photography, and the record was later evaluated by three independent evaluators. Agreement tests (Bland-Altman and Kappa) were then performed. The correlation between the two methods (Pearson correlation) was tested.
In total, 35 observations were performed on 11 patients. Based on the Kappa coefficient, the agreement among evaluators ranged from 0.56 to 0.75 (p<0.001). There was a positive and consistent association between the bispectral index and the Comfort-B scale [r=0.424 (p=0.011) to r=0.498 (p=0.002)].
Due to the strong correlation between the independent evaluators and the consistent correlation between the two methods, the results suggest that the Comfort-B scale is reproducible and useful in classifying the level of sedation in children requiring mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):119-129
DOI 10.1590/S0103-507X2012000200005
Developing guidelines for the role of the physiotherapist in neonatal and pediatric intensive care units is essential because these professionals are responsible for the rehabilitation of critically ill patients. Rehabilitation includes the evaluation and prevention of functional kinetic alterations, application of treatment interventions (respiratory and/or motor physiotherapy), control and application of medical gases, care of mechanical ventilation, weaning and extubation, tracheal gas insufflation, inflation/deflation of the endotracheal cuff protocol, and surfactant application, aiming to allow patients to have a full recovery and return to their functional activities. In this article, we present guidelines that are intended to guide the physiotherapist in some of the prevention/treatment interventions in respiratory therapy (airway clearance, lung expansion, position in bed, airway suction, drug inhalation, and cough assist), which help in the rehabilitation process of newborns and children in intensive care units during mechanical ventilation and up to 12 hours following extubation.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):130-136
DOI 10.1590/S0103-507X2012000200006
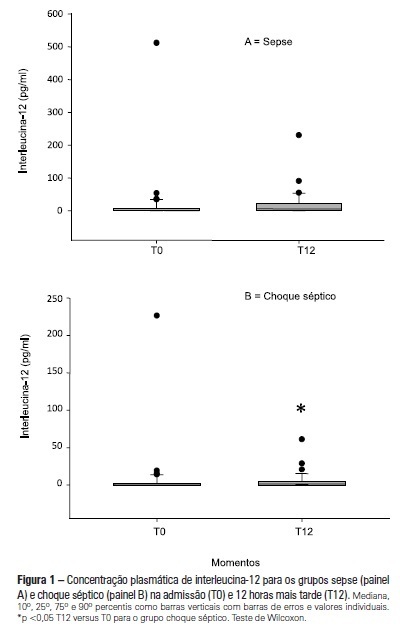
OBJECTIVE: To examine the behavior of interleukin-12 and verify whether it can be used to differentiate septic conditions in children. METHODS: Septic children aged between 28 days and 14 years, prospectively enrolled from 01/2004 to 12/2005, were divided into sepsis (SG; n=47) and septic shock (SSG; n=43) groups. Interleukin-12 levels were measured at admission (T0) and 12 hours later (T12). Disease severity was assessed by the PRISM score. RESULTS: Interleukin-12 levels did not differentiate children with sepsis from those with septic shock at admission [SSG: 0.24 (0-226.4)=SG: 1.23 (0-511.6); p=0.135)] and T12 [SG: 6.11 (0-230.5)=SSG: 1.32 (0-61.0); p=0.1239)]. Comparing time points, no significant difference was observed in the SG [SG, T0: 1.23 (0-511.6)=T12: 6.11 (0-230.5); p=0.075]. In SSG however, interleukin-12 increased from T0 to T12 (SSG, T0: 0.24 (0-226.4)
Abstract
Rev Bras Ter Intensiva. 2011;23(1):78-86
DOI 10.1590/S0103-507X2011000100013
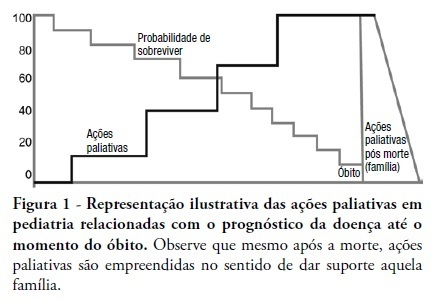
This review discusses the main dilemmas and difficulties related to end-of-life decision's in children with terminal and irreversible diseases and propose a rational sequence for delivering palliative care to this patients' group. The Medline and Lilacs databases were searched using the terms 'end of life', 'palliative care', 'death' and 'terminal disease' for articles published in recent years. The most relevant articles and those enrolling pediatric patients were selected and compared to previous authors' studies in this field. The current Brazilian Medical Ethics Code (2010) was analyzed regarding end-oflife practices and palliative care for terminal patients. Lack of knowledge, insufficient specific training, and legal concerns are the main reasons why end-of-life decisions in terminal children are based on medical opinion with scarce family participation. The current Brazilian Medical Ethics Code (2010) fully supports end-of-life decisions made consensually with active family participation. Honest dialogue with the family regarding diagnostic, prognostic, therapeutic and palliative care measures should be established gradually to identify the best strategy to meet the child's end-of-life needs. Treatment focused on the child's welfare combined with the family's participation is the basis for successful palliative care of children with terminal diseases.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):300-304
DOI 10.1590/S0103-507X2010000300013
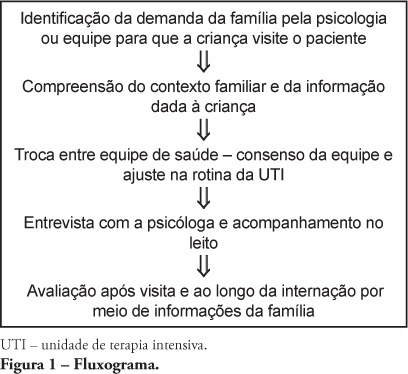
Most hospitals only allow children above 12 years-old to visit adult intensive care unit patients. However, younger children participating in the hospitalization process manifest, through their family members, their willingness to visit their hospitalized relatives. This raises different health care team members' opinions on how to manage their visits to the intensive care unit and prevent psychological harm. Aiming to expand and support this practice, a literature review was conducted, and the children's cognitive and emotional development phases related to understanding of death studied. From this, a routine for children's visits to adult intensive care unit is proposed.