Abstract
Rev Bras Ter Intensiva. 2009;21(1):45-50
DOI 10.1590/S0103-507X2009000100007
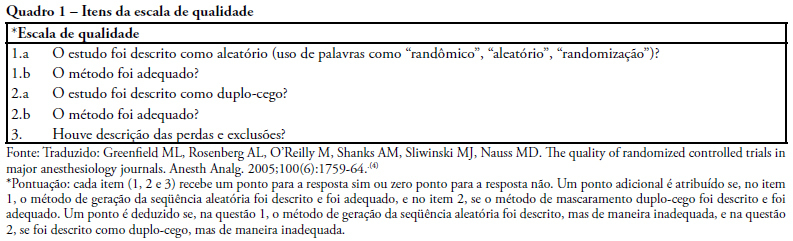
OBJECTIVE: A randomized clinical trial is a prospective study that compares the effect and value of interventions in human beings, of one or more groups vs. a control group. The objective of this study was to evaluate the quality of published randomized clinical trials in Intensive care in Brazil. METHODS: All randomized clinical trials in intensive care found by manual search in Revista Brasileira de Terapia Intensiva from January 2001 to March 2008 were assessed to evaluate their description by the quality scale. Descriptive statistics and a 95 % confidence interval were used for the primary outcome. Our primary outcome was the randomized clinical trial quality. RESULTS: Our search found 185 original articles, of which 14 were randomized clinical trials. Only one original article (7.1%) showed good quality. There was no statistical significance between the collected data and the data shown in the hypothesis of this search. CONCLUSION: It can be concluded that in the sample of assessed articles 7% of the randomized clinical trials in intensive care published in a single intensive care journal in Brazil, present good methodological quality.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):51-57
DOI 10.1590/S0103-507X2009000100008
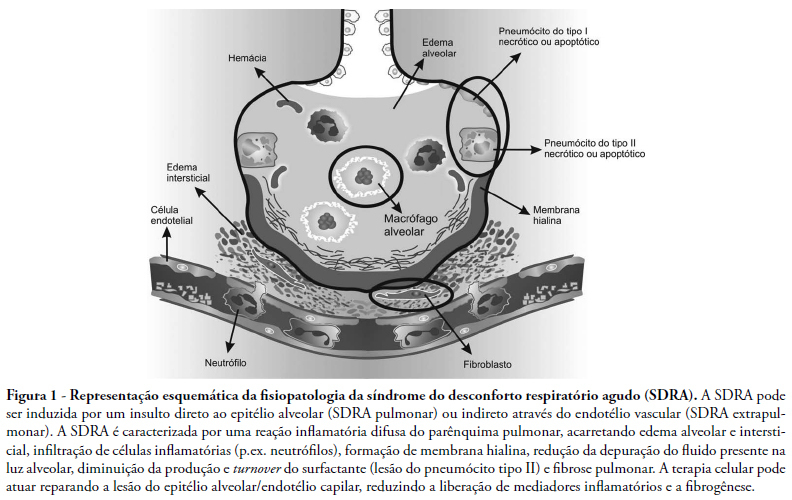
Acute respiratory distress syndrome is characterized by an acute pulmonary inflammatory process induced by the presence of a direct (pulmonary) insult that affects lung parenchyma, or an indirect (extrapulmonary) insult that results from an acute systemic inflammatory response. It is believed that an efficient therapy for the acute respiratory distress syndrome should attenuate inflammatory response and promote adequate repair of the lung injury. This article presents a brief review on the use of stem cells and their potential therapeutic effect on the acute respiratory distress syndrome. This systematic review was based upon clinical and experimental acute respiratory distress syndrome studies included in the MedLine and SciElO database during the last 10 years. Stem cell transplant lead to an improvement in lung injury and fibrotic process by inducing adequate tissue repair. This includes alveolar epithelial cell differentiation,and also reduces pulmonary and systemic inflammatory mediators and secretion of growth factors. Stem cells could be a potential therapy for acute respiratory distress syndrome promoting lung repair and attenuating the inflammatory response. However, mechanisms involving their anti-inflammatory and antifibrinogenic effects require better elucidation, limiting their immediate clinical use in acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):58-64
DOI 10.1590/S0103-507X2009000100009
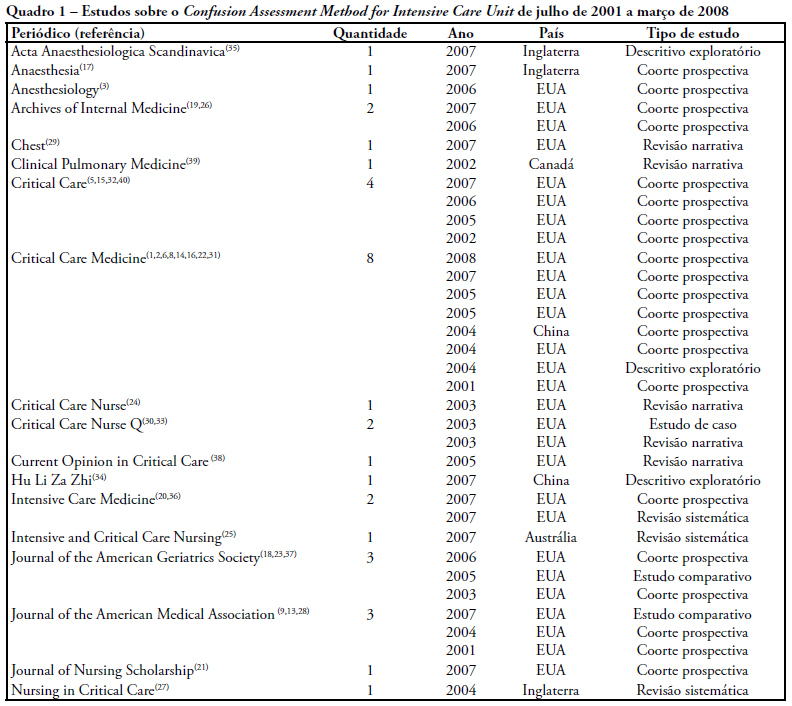
Delirium is frequently observed in intensive care unit patients and its occurrence is related to increased morbidity and mortality, length of stay, functional decline and high costs. The Confusion Assessment Method for Intensive Care Unit is a tool that facilitates early identification and occurrence of delirium among intubated patients. Objective: To verify the aspects of delirium studied by means of the Confusion Assessment Method for Intensive Care Unit. A literature review was conducted in the LILACS, MedLine, PubMed and CINAHL databases, from 2001, when the Confusion Assessment Method for Intensive Care Unit was validated, to 2008. Descriptors used for LILACS, MedLine and PubMed were delirium and intensive care unit, while for the CINAHL database, delirium and intensive care were used. From 293 articles, 35 were selected. The aspects analyzed disclosed, different types of delirium in different intensive care units. Variation in sensitivity was of 93% to 100% and variation in specificity, 89% to 100% of the Confusion Assessment Method for Intensive Care Unit, an important tool for detection, characterization and control of delirium and its impact. The aspects of delirium studied by means of the Confusion Assessment Method for Intensive Care Unit were: the performance index, identification, management, cost of treatment, morbidity and mortality due to delirium.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):65-71
DOI 10.1590/S0103-507X2009000100010
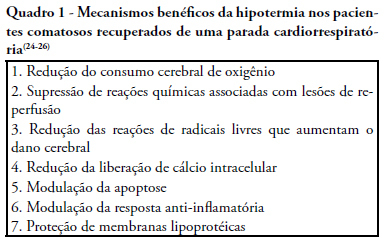
Cardiac arrest survivors frequently suffer from ischemic brain injury associated with poor neurological outcome and death. Therapeutic hypothermia improves outcomes in comatose survivors after resuscitation from out-of-hospital cardiac arrest. Considering its formal recommendation as a therapy, post-return of spontaneous circulation after cardiac arrest, the objective of this study was to review the clinical aspects of therapeutic hypothermia. Non-systematic review of articles using the keywords "cardiac arrest, cardiopulmonary resuscitation, cooling, hypothermia, post resuscitation syndrome" in the Med-Line database was performed. References of these articles were also reviewed. Unconscious adult patients with spontaneous circulation after out-of-hospital ventricular fibrillation or pulseless ventricular tachycardia should be cooled. Moreover, for any other rhythm or in the intra-hospital scenario, such cooling may also be beneficial. There are different ways of promoting hypothermia. The cooling system should be adjusted as soon as possible to the target temperature. Mild therapeutic hypothermia should be administered under close control, using neuromuscular blocking drugs to avoid shivering. The rewarming process should be slow, and reach 36º C, usually in no less then 8 hours. When temperature increases to more than 35º C, sedation, analgesia, and paralysis could be discontinued. The expected complications of hypothermia may be pneumonia, sepsis, cardiac arrhythmias, and coagulopathy. In spite of potential complications which require rigorous control, only six patients need to be treated to save one life.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):72-79
DOI 10.1590/S0103-507X2009000100011
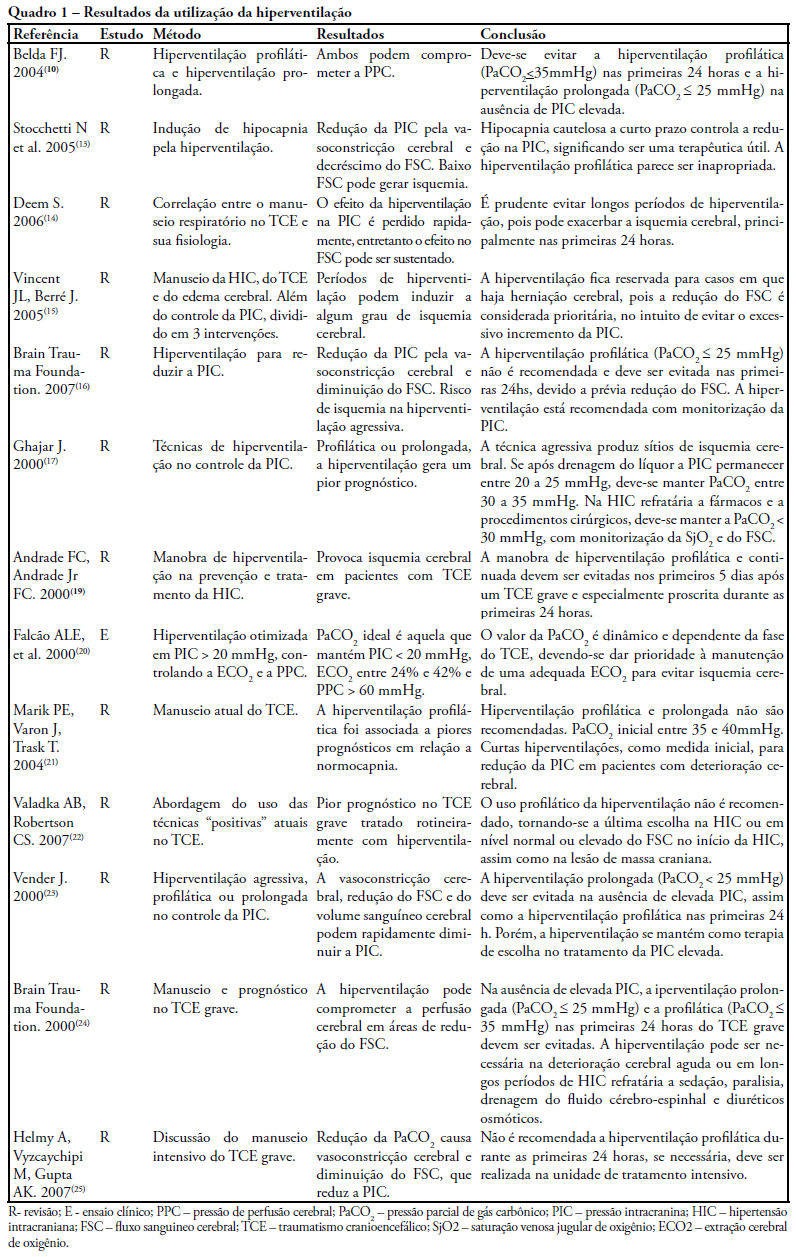
The study intended to make a critical review on use of pulmonary hyperventilation maneuvers and the different positive end-expiratory pressures applied to traumatic brain injury patients. As a reference were used publications in English, Spanish and Portuguese, contained in the following databases: MedLine, SciELO and LILACS, from 2000 to 2007, we included all studies about the use of pulmonary hyperventilation maneuvers and the different positive end-expiratory levels used for adult patients with brain injury at acute or chronic stage. Thirty one trials were selected, 13 about pulmonary hyperventilation, as prophylaxis, prolonged or optimized and 9 shows the levels of positive end-expiratory pressures used, ranging from 0 to 15 cmH2O. The prophylactic hyperventilation maneuver in the first 24 hours can lead to an increase of cerebral ischemia; the prolonged hyperventilation must be avoided if intracranial pressure did not increase; however optimized hyperventilation seems to be the most promising technique for control of the intracranial pressure and cerebral perfusion pressure; the rise of the positive end-expiratory pressure, up to 15cmH2O, can be applied in a conscientious form aiming to increase arterial oxygen saturation in lung injury.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):80-88
DOI 10.1590/S0103-507X2009000100012
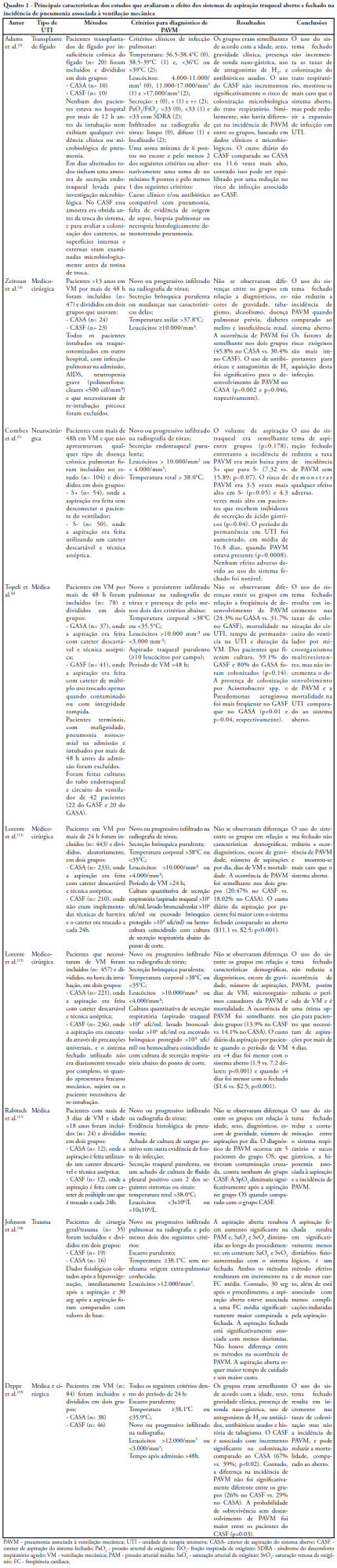
Pneumonia is the most common nosocominal infection in intensive care units and mechanical ventilation is a significant factor associated to its development. The objective of this study was to describe the impact of the open and closed tracheal suction systems on the incidence of ventilation-associated pneumonia. A search in the Pubmed database was performed to identify randomized controlled trials, published from 1990 to November 2008. Nine studies were included. Of the studies reviewed, seven did not disclose any significant advantages of using the closed system when compared to th e open, whereas two reported that use of the closed system increased colonization rates but not incidence of ventilation-associated pneumonia and one observed that use of the closed system did not increase colonization of the respiratory tract but reduced the spread of infection resulting in decreased sepsis rates. Only two studies found a reduction in the incidence of ventilation-associated pneumonia with use of the closed system, and one revealed a 3.5 times greater risk of developing this infection with the open system. Results suggest that the impact of the open and closed tracheal suction system is similar on development of ventilation-associated pneumonia, choice of the suction system should therefore be based on other parameters. While the closed system increases risk of colonization of the respiratory tract, but has the advantages of continuing mechanical ventilation and lessening hemodynamic impairment.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):89-95
DOI 10.1590/S0103-507X2009000100013
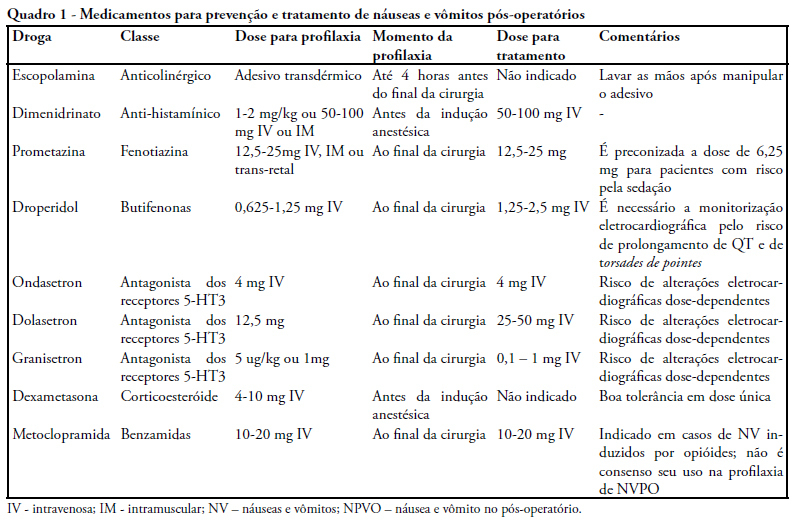
Postoperative nausea and vomiting are common and can be prevented. Complications of this condition cause higher rates of morbidity and mortality. A review of literature was carried out on MEDLINE, with focus on controlled clinical trials. Pathophysiology is complex, with many afferent and efferent pathways, and its comprehension facilitate the choice of medication. Risk factors are presented, with a stratified score of chance to develop postoperative nausea and vomiting. An algorithm for identification of higher risk patients was elaborated and classified the level of prevention/treatment recommended to avoid excessive use of drugs and their side effects. Postoperative nausea and vomiting must be prevented, because of the involved complications and discomfort for patients. A systematic approach with analysis of preoperative risk factors and prescription of medication can be effective for prevention.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):9-17
DOI 10.1590/S0103-507X2009000100002
OBJECTIVES: The objective of this study was to evaluate variables related to intra hospital mortality at 28 days, of aged persons with severe sepsis and septic shock in a clinical ICU. METHODS: One hundred and fifty-two patients aged > 65 years with severe sepsis and septic shock were followed for 28 days and the variables were collected on days 1, 3, 5, 7, 14 and 28 of stay. To compare categorical variables the Chi-square test was used and the Mann-Whitney or t test for continuous variables. All tests were double-tailed, alpha error of 0.05. RESULTS: Mean age was 82.0 ± 9.0 years and 64.5% were female. Mortality was of 47.4%. Related to death were the following: Acute Physiological and Chronic Heath Evaluation II score (p < 0.001), Sequential Organ Failure Assessment score on days 1, 3, 5, 7 (p < 0.001), length of stay in intensive care (p < 0.001), number of organ failures (p < 0.001), high serum lactate on day 3 (p = 0.05), positive troponin I (p < 0.01), echocardiographic variables (systolic diameter p = 0.005; diastolic diameter p = 0.05; shortening fraction p = 0.02), previous renal disease (p = 0.03), shock (p < 0.001), mechanical ventilation (p < 0.001) and Lawton scale (p = 0.04). CONCLUSIONS: Shock, elevated lactate, organ failure, especially respiratory were more prevalent in non-survivors. Heart dysfunction detected by echocardiographic variables and positive troponin I may play an important role in the mortality of aged patients with sepsis.