Abstract
Rev Bras Ter Intensiva. 2008;20(3):249-253
DOI 10.1590/S0103-507X2008000300007
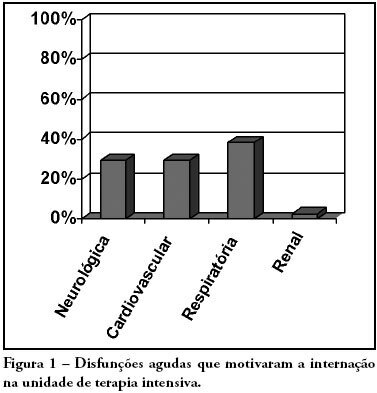
OBJECTIVES: Due to the high incidence in our service, we did object on this study describe the features and outcome of patients with systemic lupus erythematosus (SLE) admitted to the intensive care unit of Walter Cantídio University Hospital METHODS: Patients were restrospectively characterized according to demography parameters, time of diagnosis of SLE, organ dysfunction and laboratorial parameters at admission, supportive therapies during their stay, length of stay in the hospital before admission, length of stay in the unit, readmission to the unit and outcome. We also evaluated Systemic Lupus Erythematosus Disease Activity (SLEDAI) score, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, expected mortality and standardized mortality ratio. RESULTS: From November 2003 to October 2006, 1,052 patients were admitted to the intensive care unit. Fifty patients had SLE and were included in this retrospective study. Of the 50 patients with SLE admitted to the ICU, 88.2% were female. The mean age was 30.3 ± 12.8 years. The median time of diagnosis of SLE was 67 months. The most common organ dysfunctions were renal (70.6%), cardiovascular (61.8%), respiratory (55.9%) and neurological (55.9%). The main reasons for admission to the ICU were respiratory (38.2%), cardiologic (29.4%) and neurological (29.4%) dysfunctions. Among the intensive care therapies, 44.1% of the patients needed blood products, 41.2% vasopressor agents and 35.3% mechanical ventilation, 23.5% dialysis. The mean SLEDAI score was 15.0 ± 12.2. The mean APACHE II score was 19.3 ± 6.8, with a predicted mortality rate of 37.6%. The actual mortality rate in ICU was 29.4%, with 8.8% before 48 hours. The standardized mortality ratio was 0.78. Patients with APACHE II > 18, with more than 3 acute organ involvements, leukopenia (< 4000 cells/mm3) and gastrointestinal or metabolic involvement had higher mortality in the intensive care unit. CONCLUSION: Although the severity of patients at admission to the ICU, demonstrated by APACHE II and the acute dysfunctions, the outcomes of analysed patients sugest susceptibility to the therapy.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):254-260
DOI 10.1590/S0103-507X2008000300008
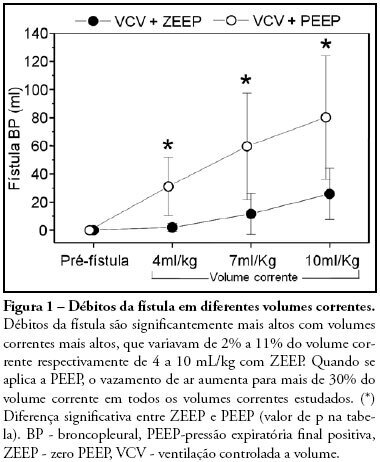
OBJECTIVES: The present study was designed to identify the effect of positive end expiratory pressure (PEEP) and the ideal pulmonary tidal volume to ventilate animals with a surgically produced bronchopleural fistula, aiming to reduce fistula output without affecting gas exchange. METHODS: Hemodynamic and respiratory assessment of gas exchange was obtained in five, healthy, young, mechanically ventilated Large White pigs under volume controlled ventilation with FiO2 of 0.4 and an inspiration:expiration ratio of 1:2, keeping respiratory rate at 22 cpm. A bronchopleural fistula was produced by resection of the lingula. Underwater seal drainage was installed and the thorax was hermetically closed. Gas exchange and fistula output were measured with the animals ventilated sequentially with tidal volumes of 4 ml/kg, 7 ml/kg and 10 ml/Kg alternating zero of positive end expiratory pressure (ZEEP) and PEEP of 10 cmH2O, always in the same order. RESULTS: These findings are attributed to reduced alveolar ventilation and ventilation/perfusion abnormalities and were attenuated with larger tidal volumes. PEEP increases air leak, even with low volume (of 2.0 ± 2.8mL to 31 ± 20.7mL; p= 0.006) and decreases alveolar ventilation in all tidal volumes. Alveolar ventilation improved with larger tidal volumes, but increased fistula output (10 mL/kg - 25.8 ± 18.3mL to 80.2 ± 43.9mL; p=0.0010). Low tidal volumes result in hypercapnia (ZEEP - Toneloto MGC, Terzi RGG, Silva WA, Moraes AC, Moreira MM 83.7± 6.9 mmHg and with PEEP 10 - 93 ± 10.1mmHg) and severely decreased arterial oxygen saturation, about of 84%. CONCLUSIONS: The tidal volume of 7 ml/Kg with ZEEP was considered the best tidal volume because, despite moderate hypercapnia, arterial oxygen saturation is sustained around 90%, alveolar ventilation improves and the fistula output is reduced when compared with a tidal volume of 10ml/Kg. A low tidal volume results in hypercapnia and severe desaturation. Finally, at any tidal volume, PEEP increases the fistula leak and decreases alveolar ventilation.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):261-266
DOI 10.1590/S0103-507X2008000300009
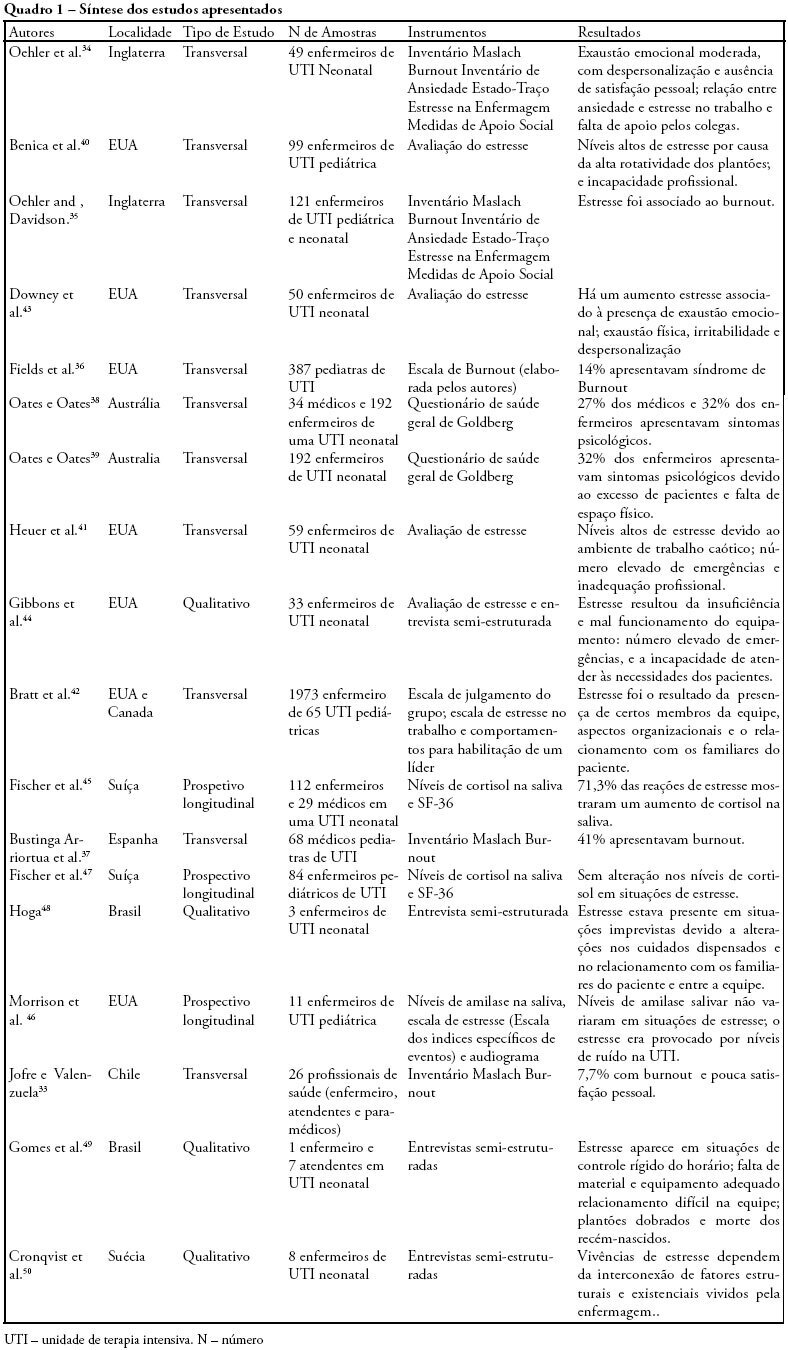
OBJECTIVES: Bibliographic review on occupational stress and burnout presence in physicians and nurses that work in pediatric and neonatal intensive care units. METHODS: The articles were selected from the MedLine, LILACS and SciElo data base using the key words: stress, burnout, physicians, nursing, intensive care unit, pediatric intensive care unit and neonatal intensive care unit. The studied period ranged from 1990 to 2007. RESULTS: Health professionals who work in pediatric and neonatal intensive care units are strong candidates for developing stress, psychological alterations and burnout syndrome. Researches on this subject identified important alterations suffered by these physicians and nurses, such as: work overload, burnout, desires of giving up their jobs, high levels of cortisol, among other alterations. CONCLUSIONS: Professionals, who work in pediatric and neonatal intensive care units, due to the specificity of their job, are liable to develop occupational stress, and consequently burnout. These results suggest the need for further research with the objective of developing preventive measures and intervention models.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):267-277
DOI 10.1590/S0103-507X2008000300010
The present review discusses the hemodynamic and immune-modulatory effects of hypertonic saline in experimental shock and in patients with sepsis. We comment on the mechanisms of action of hypertonic saline, calling upon data in hemorrhagic and septic shock. Specific actions of hypertonic saline applicable to severe sepsis and septic shock are highlighted. Data available support potential benefits of hypertonic saline infusion in various aspects of the pathophysiology of sepsis, including tissue hypoperfusion, decreased oxygen consumption, endothelial dysfunction, cardiac depression, and the presence of a broad array of pro-inflammatory cytokines and various oxidant species. A therapy that simultaneously blocks the damaging components of sepsis will have an impact on the management of sepsis. Proper designed prospective studies may prove a beneficial role for hypertonic saline solution in the future.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):144-148
DOI 10.1590/S0103-507X2008000200005
BACKGROUND AND OBJECTIVES: Failure or delay to diagnose brain death leads to needless occupation of a hospital bed, emotional and financial losses, and unavailability of organs for transplants. The intensive care physician plays an essential role in this diagnosis. This study intended to evaluate intensivists' knowledge concerning brain death. METHODS: Cross-sectional study in 15 intensive care units (ICU) in eight hospitals in the city of Porto Alegre, Brazil. RESULTS: Two hundred forty-six intensivists were interviewed in a consecutive sample between April and December 2005. The prevalence of lack of knowledge regarding the concept was of 17%. Twenty per cent of the interviewees ignored the legal need for complementary confirmatory tests for their diagnosis. Forty-seven per cent considered themselves as having the highest level of assurance to explain the concept to a patient's family members. Twenty-nine per cent erroneously determined the legal time of death for brain dead patients. Pediatric intensivists had less knowledge about the concept, when compared to intensivists for adults (p < 0.001). CONCLUSIONS: Current knowledge of brain death is insufficient in Brazil, among the health care professionals who most often find patients in this situation. Education on the subject is needed to avoid unnecessary expenses, reduce family suffering and increase the offer of organs for transplant.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):149-153
DOI 10.1590/S0103-507X2008000200006
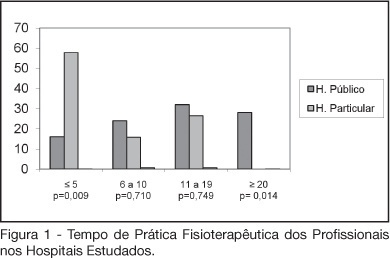
BACKGROUND AND OBJECTIVES: The number of patients requiring prolonged time on mechanical ventilation is increasing considerably in the intensive care unit (ICU). The objective of this study was to characterize the variability of methods and criteria used by physiotherapists to obtain weaning parameters in hospitals of Fortaleza. METHODS: After approval by the UNIFOR Ethics Committee, survey questionnaires were distributed among physiotherapists working in the ICU of three public and three private hospitals. Forty-four physiotherapists answered thirty-two multiple choice questions anonymously. RESULTS: The main results concerned parameters commonly evaluated by physiotherapists. A significant difference between hospitals was found regarding the rapid shallow breathing index and maximum inspiratory pressure, which are more often used in private hospitals, with a percentage of 100% and 89.5%, respectively. Concerning the ventilatory mode for obtaining the weaning parameters for mechanical ventilation; the T-tube was the most used, not only in the public (56%) but also in the private hospitals (57.9%). CONCLUSIONS: Variability in the methods and criteria used to obtain weaning parameters by the physiotherapists was found in public and private hospitals in Fortaleza. Results from this survey stress the need to develop new scientific studies to standardize the techniques used for weaning.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):154-159
DOI 10.1590/S0103-507X2008000200007
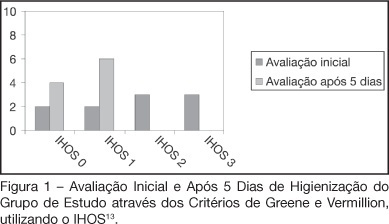
BACKGROUND AND OBJECTIVES: Patients admitted to an intensive care unit (ICU), in most cases do not have a proper oral hygiene. This deficient condition of oral hygiene in critical patients often triggers periodontitis, gingivitis and other systemic and oral complications. This research aimed to evaluate the efficiency of the antimicrobial action of a solution with bioactive enzymatic system for oral hygiene, in totally care-dependent patients admitted to ICU. METHODS: A prospective, double blind pilot study was conducted with 20 patients admitted to an ICU, divided into 2 groups with the same technique of oral hygiene, protocols but using different solutions: the study group (n = 10) using an oral solution with enzymatic system and the control group (n = 10) using an oral solution based on cetylpyridinium. RESULTS: Results of microbiological cultures collected in the study group and control group, before and after the use of enzymatic solution, showed no significant difference between groups (p = 0.41). In clinical evaluation of the Simplified Oral Hygiene Index (SOHI) statistical significance was found by the Fisher Exact test (p = 0.01) when comparing the study group and control group. The value of statistical significance was set at 5%, or p < 0.05. CONCLUSIONS: The use of oral rinse with the lactoperoxidase enzyme was effective in the clinical evaluation of the oral hygiene of patients totally care-dependent in the hospital. This study stresses the importance of developing more research on the oral care of these patients.