Abstract
Rev Bras Ter Intensiva. 2020;32(2):295-300
DOI 10.5935/0103-507X.20200046
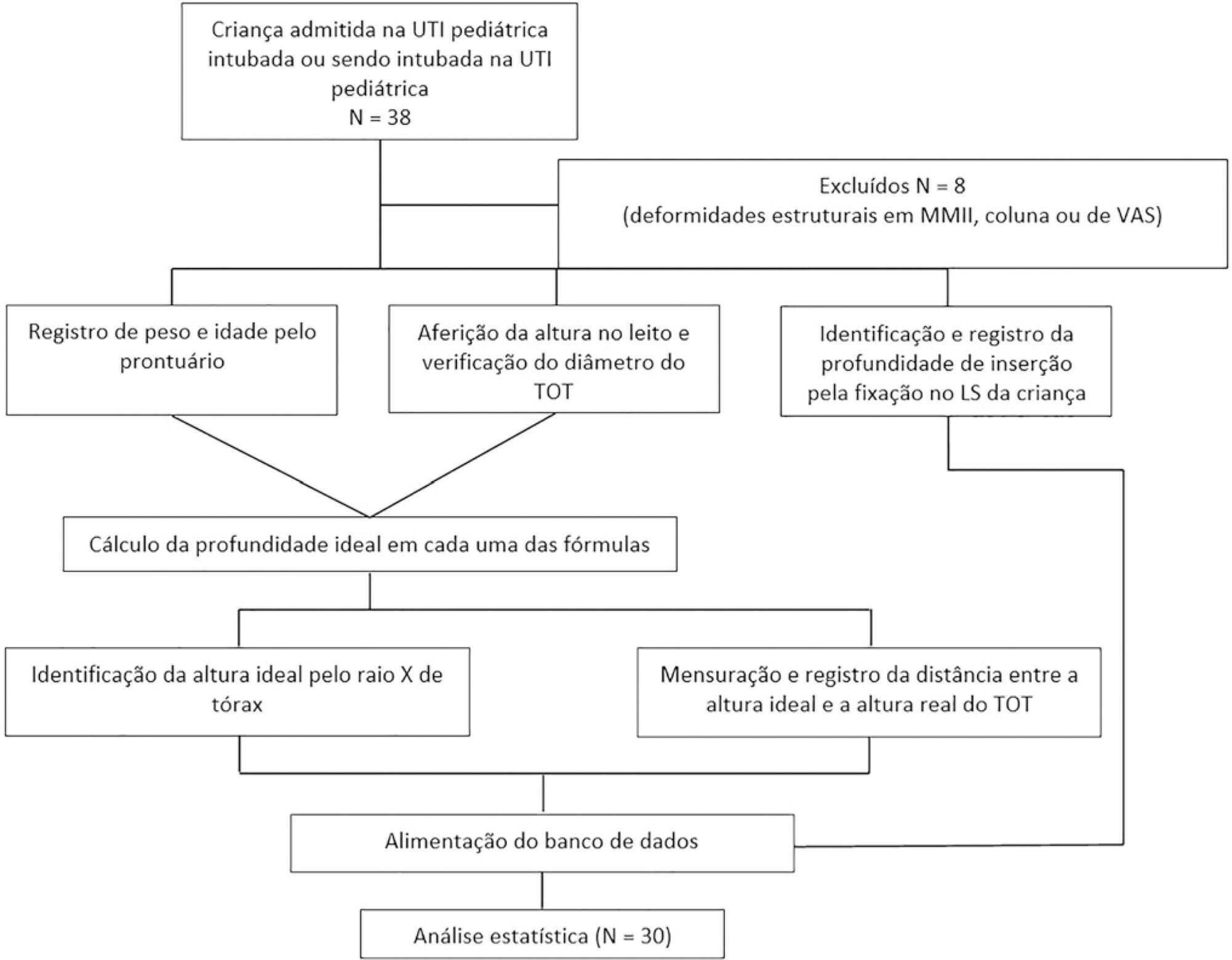
To evaluate the effectiveness of the different formulas for estimating the insertion depth of an endotracheal tube in children.
This was an observational and cross-sectional study that included children between 29 days and 2 years of age who were hospitalized in a pediatric intensive care unit and mechanically ventilated. The formulas based on height [(height/10) + 5], the inner diameter of the tube (endotracheal tube × 3), and weight (weight + 6) were evaluated to determine which of them showed better concordance with the ideal insertion depth of the endotracheal tube as evaluated by X-ray.
The correlation between the height-based calculation and the ideal depth observed on X-ray was strong, with r = 0.88, p < 0.05, and a concordance correlation coefficient of 0.88; the correlation between the weight-based calculation and depth on X-ray was r = 0.75, p < 0.05, and concordance correlation coefficient 0.43; and the correlation between endotracheal tube diameter-based calculation and depth on X-ray was r = 0.80, p < 0.05, and concordance correlation coefficient 0.78. Lin’s concordance correlation analysis indicated that the measurements showed weak concordance (< 0.90).
The formulas that estimate the insertion depth of the endotracheal tube in children were not accurate and were discordant with the gold-standard method of X-ray evaluation. There is a need for a new method based on anthropometric variables (weight and height) and age that is effective in guiding health professionals of pediatric intensive care units at the time of intubation.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):487-495
DOI 10.5935/0103-507X.20180070
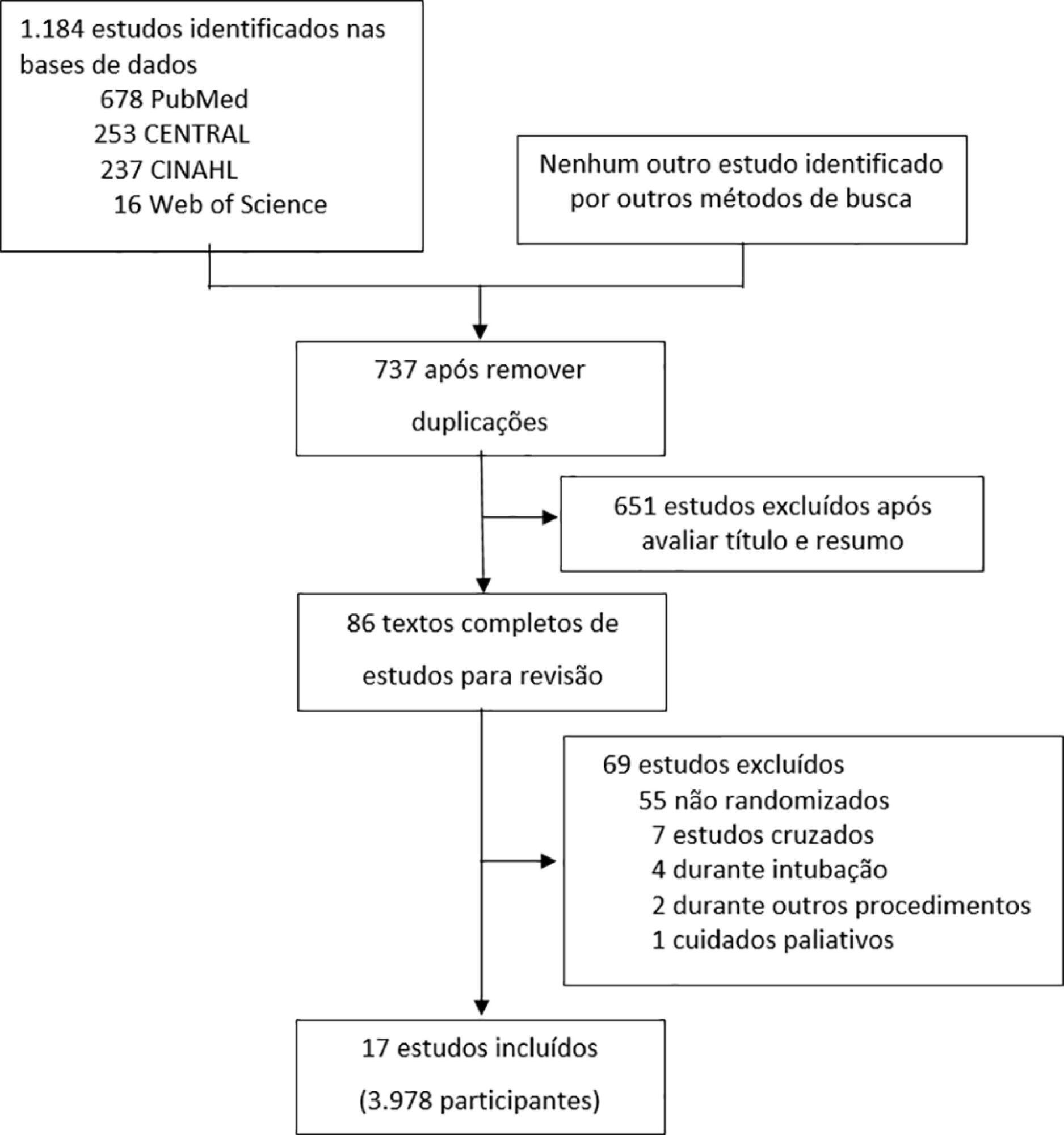
To evaluate the efficacy of high-flow nasal cannula in the prevention of intubation and re-intubation in critically ill patients compared to conventional oxygen therapy or noninvasive ventilation.
This systematic review was performed through an electronic database search of articles published from 1966 to April 2018. The primary outcome was the need for intubation or re-intubation. The secondary outcomes were therapy escalation, mortality at the longest follow-up, hospital mortality and the need for noninvasive ventilation.
Seventeen studies involving 3,978 patients were included. There was no reduction in the need for intubation or re-intubation with high-flow nasal cannula (OR 0.72; 95%CI 0.52 - 1.01; p = 0.056). There was no difference in the need for therapy escalation (OR 0.80, 95% CI 0.59 - 1.08, p = 0.144), mortality at the longest follow-up (OR 0.94; 95%CI 0.70 - 1.25; p = 0.667), hospital mortality (OR 0.84; 95%CI 0.56 - 1.26; p = 0.391) or noninvasive ventilation (OR 0.64, 95%CI 0.39 - 1.05, p = 0.075). In the trial sequential analysis, the number of events included was lower than the optimal information size with a global type I error > 0.05.
In the present study and setting, high-flow nasal cannula was not associated with a reduction of the need for intubation or re-intubation in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):367-372
DOI 10.5935/0103-507X.20140056
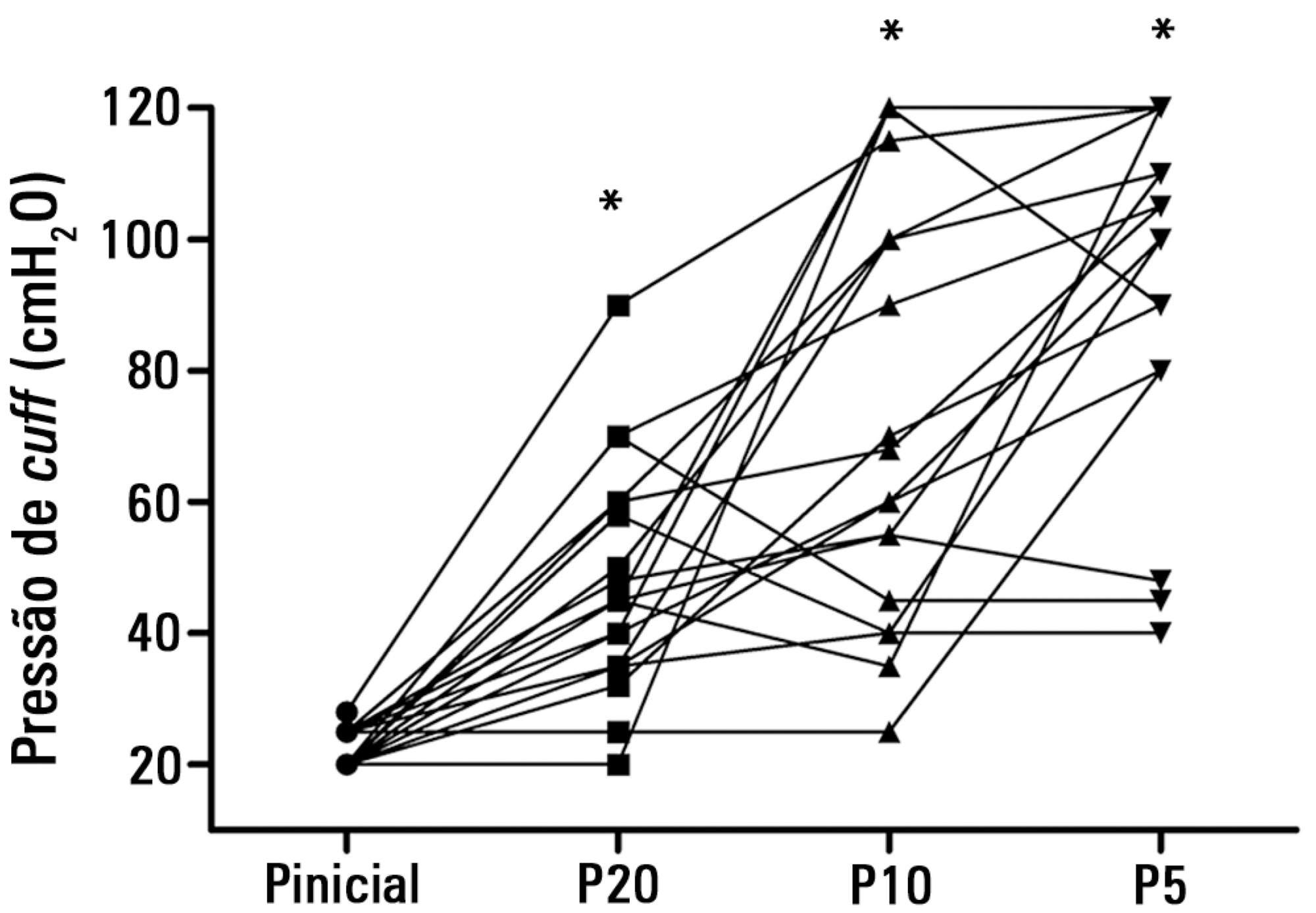
To test the effectiveness of using a cuff pressure relief valve technique to maintain cuff pressure levels within the normal in vitro range (Phase 1) in patients admitted to the intensive care unit (Phase 2) and to test the reproducibility of the technique using different syringes.
In Phase 1, a tracheal tube was inserted into a trachea model. Ten- and 20mL syringes were used to inflate the cuff through the tracheal tube. The cuff was slowly and steadily inflated until the syringe plunger would move in the opposite direction of the application. After the plunger stopped, the cuff pressures were recorded. In Phase 2, the same maneuvers for inflating the cuff were performed on 20 patients using 5, 10, and 20mL syringes and were compared with manometer measurements. The intraclass correlation coefficient and Bland-Altman analysis were employed to determine the reproducibility and agreement between syringes. Data were expressed as medians (interquartile range).
There was no reproducibility between syringes with an intraclass correlation coefficient ranging between -0.33 and 0.8 (p>0.05). The pressures generated with the syringes were higher than the pressures generated using a standard manometer: the 5mL syringe pressure was 105cmH2O (82.5-120cmH2O), the 10mL syringe pressure was 69cmH2O (47.5-111.3cmH2O), and the 20mL syringe pressure was 45cmH2O (35-59.5cmH2O). The Bland-Altman analysis confirmed the large bias and variability between the syringes used, compared with the manometer.
The use of syringes is not an effective technique for determining the cuff pressure in patients admitted to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):169-172
DOI 10.1590/S0103-507X2009000200009
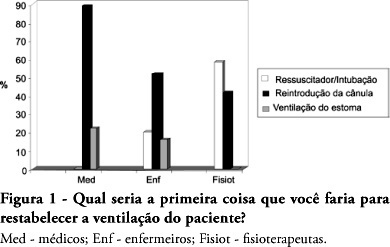
OBJECTIVES: The aim of this study was to evaluate the level of knowledge of health care professionals in an emergency situation related to tracheostomy tube displacement METHODS: a descriptive and exploratory study was carried out with the intensive care unit health professionals of a university hospital in Salvador, Brazil, from July to September 2007. For this purpose, a questionnaire was translated and adapted from a previous study. Questions were: 1- Have you dealt with this emergency? 2 - What is the first thing you do? 3- Do you know what the stay sutures are for? 4 - How are they used in an emergency setting? 5 -Do you know what to do with the introducer? RESULTS: the sample comprised 41 professionals (nine physicians, 20 nurses and 12 physiotherapists). A descriptive analysis showed that 63% of professionals had never experienced such complications. Analysis of a subgroup showed that 42% of physiotherapists, 56% of physicians and 69% of nurses would act inappropriately. Analyzing the level of knowledge about the importance of stay sutures, the study showed that 78% of the sample did not know what they were or how to use them, and 63.4% did not know how to use the introducer correctly. CONCLUSIONS: , regarding the use of a tracheostomy tube in a situation of emergency, the level of knowledge of the professionals evaluated was insufficient. The greatest shortcoming was detected in the level of knowledge about stay sutures.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):339-343
DOI 10.1590/S0103-507X2008000400004
OBJECTIVE: After brain injury intracranial hypertension is the major cause of mortality, in addition to the possibility of functional, behavioral and cognitive sequels. Scarcity of studies on the effects of respiratory physiotherapy on these patients may lead to contradictory performances. This study aimed to assess the effects of customary respiratory physiotherapy maneuvers on intracranial and cerebral perfusion pressures in patients with severe brain injury. METHODS: Clinical, prospective trial with patients with severe traumatic brain injury, mechanically ventilated and with a continued measurement of intracranial pressure. The effects of manual vibrocompression maneuvers and intratracheal aspiration with or without saline infusion on the measurements of intracranial and cerebral perfusion pressures, between the first and third day after cerebral injury were evaluated. RESULTS: Data were collected from 11 patients, 41 years of age (median) and APACHE II of 19.5 ± 5. The manual vibrocompression maneuver did not cause an increase of intracranial pressure on any of the days assessed. Intracranial pressure significantly increased after intratracheal aspiration maneuvers in relation to the basal measurement (day1, 9.5 ± 0.9 mm Hg vs 18.0 ± 3.2 mm Hg; day 2, 10.6 ± 1.7 mm Hg vs 21.4 ± 3.8 mm Hg; day 3, 14.4 ± 1.0 vs 24.9 ± 2.7 mm Hg; p<0.05 for all). However, these elevations were transient (about 27 seconds) and accompanied by compensatory increases of the cerebral perfusion pressure. CONCLUSION: The manual vibrocompression maneuver did not increase intracranial pressure or cerebral perfusion pressure in patients with severe brain injury. Intratracheal aspiration induced a significant and transient increase of the intracranial and cerebral perfusion pressures.

Abstract
Rev Bras Ter Intensiva. 2008;20(3):220-225
DOI 10.1590/S0103-507X2008000300003
OBJECTIVES: Correct cuff inflation allows appropriate ventilation, and prevents aspiration pneumonia as well as several tracheal complications. The objective of this study was to evaluate endotracheal cuff pressure and/or tracheotomy tubes at zero, 30 and 60 degrees inclination of the patient's bed head section in adult intensive care units. METHODS: A cross sectional study was carried out evaluating the cuff pressure, the expiratory tidal volume (VT) and the peak airway pressure (PP) at inclinations zero, 30 and 60 degree of the head section of the patients' bed. The 30 degree inclination was considered the standard position used as control to analyze values in the zero and 60 degree positions, which were randomly ordered. The Student's t test was used and was considered significant when p < 0.05. RESULTS: A sample of 12 women and 12 men with a mean age of 51.29 ± 19.55 years was surveyed. When inclination of the bed head section was changed from 30 to zero degrees, there was a 16.9% mean reduction of the cuff pressure and 11.8% mean increase of the PP. On the other hand, changing the position from 30 to 60 degrees caused a mean reduction of 18.8% in the cuff pressure and a mean increase of 13.3% in the PP. Findings were significant when p < 0.05. CONCLUSIONS: To prevent air leak and risk of aspiration pneumonia, adequate adjustments and monitoring of the patients cuff pressure are necessary when inclination of the bed head section is changed.