You searched for:"Flávia Ribeiro Machado"
We found (44) results for your search.-
Original Articles
Prevalence of cytomegalovirus disease in kidney transplant patients in an intensive care unit
Rev Bras Ter Intensiva. 2017;29(4):436-443
Abstract
Original ArticlesPrevalence of cytomegalovirus disease in kidney transplant patients in an intensive care unit
Rev Bras Ter Intensiva. 2017;29(4):436-443
DOI 10.5935/0103-507X.20170070
Views0See moreABSTRACT
Objectives:
To define the frequency of cytomegalovirus disease among kidney transplant patients in an intensive care unit in which this complication was suspected and to identify predisposing factors and their possible impact on clinical outcome.
Methods:
Retrospective observational study in which kidney transplant patients over the age of 18 years were hospitalized for any reason in an intensive care unit with at least one collection of samples to test for the presence of antigenemia or cytomegalovirus via polymerase chain reaction during hospitalization. Cytomegalovirus disease was defined as positive antigenemia or polymerase chain reaction above 500 copies/mL in the presence of symptoms and in the appropriate clinical setting, as judged by the attending physician.
Results:
A total of 99 patients were included (age: 53.4 ± 12.8 years, 71.6% male). Cytomegalovirus disease was diagnosed in 39 patients (39.4%). Respiratory symptoms (51%), non-specific clinical worsening (20%) or gastrointestinal symptoms (14%) were the main reasons for exam collection. Transplant time was lower in those with cytomegalovirus disease than in those without this diagnosis (6.5 months and 31.2 months, p = 0.001), along with pulse therapy in the last 6 months (41% and 16.9%, p = 0.008) and previous use of thymoglobulin in the last year (35.9% and 6.8%, p < 0.001). In the logistic regression model, only the transplant time and the use of thymoglobulin were associated with a higher frequency of cytomegalovirus. There was no difference in clinical evolution between patients with and without cytomegalovirus disease.
Conclusion:
In kidney transplant patients suspected of cytomegalovirus disease, the prevalence was high. Transplant time less than 6 months, and the use of thymoglobulin in the last year should increase the intensivist’s suspicion for this complication.
-
Commentaries
Getting a consensus: advantages and disadvantages of Sepsis 3 in the context of middle-income settings
Rev Bras Ter Intensiva. 2016;28(4):361-365
Abstract
CommentariesGetting a consensus: advantages and disadvantages of Sepsis 3 in the context of middle-income settings
Rev Bras Ter Intensiva. 2016;28(4):361-365
DOI 10.5935/0103-507X.20160068
Views0What is new on the Sepsis 3 definitions?Recently the Society of Critical Care Medicine (SCCM) and the European Society of Critical Care Medicine (ESICM) promoted a new consensus conference and published the new sepsis definitions, known as Sepsis 3.()Briefly, the broad definition of sepsis is now “a life-threatening organ dysfunction caused by dysregulated host response […]See more -
Original Articles
Risk factors for agitation in critically ill patients
Rev Bras Ter Intensiva. 2016;28(4):413-419
Abstract
Original ArticlesRisk factors for agitation in critically ill patients
Rev Bras Ter Intensiva. 2016;28(4):413-419
DOI 10.5935/0103-507X.20160074
Views0See moreABSTRACT
Objective:
To evaluate the incidence of agitation in the first 7 days after intensive care unit admission, its risk factors and its associations with clinical outcomes.
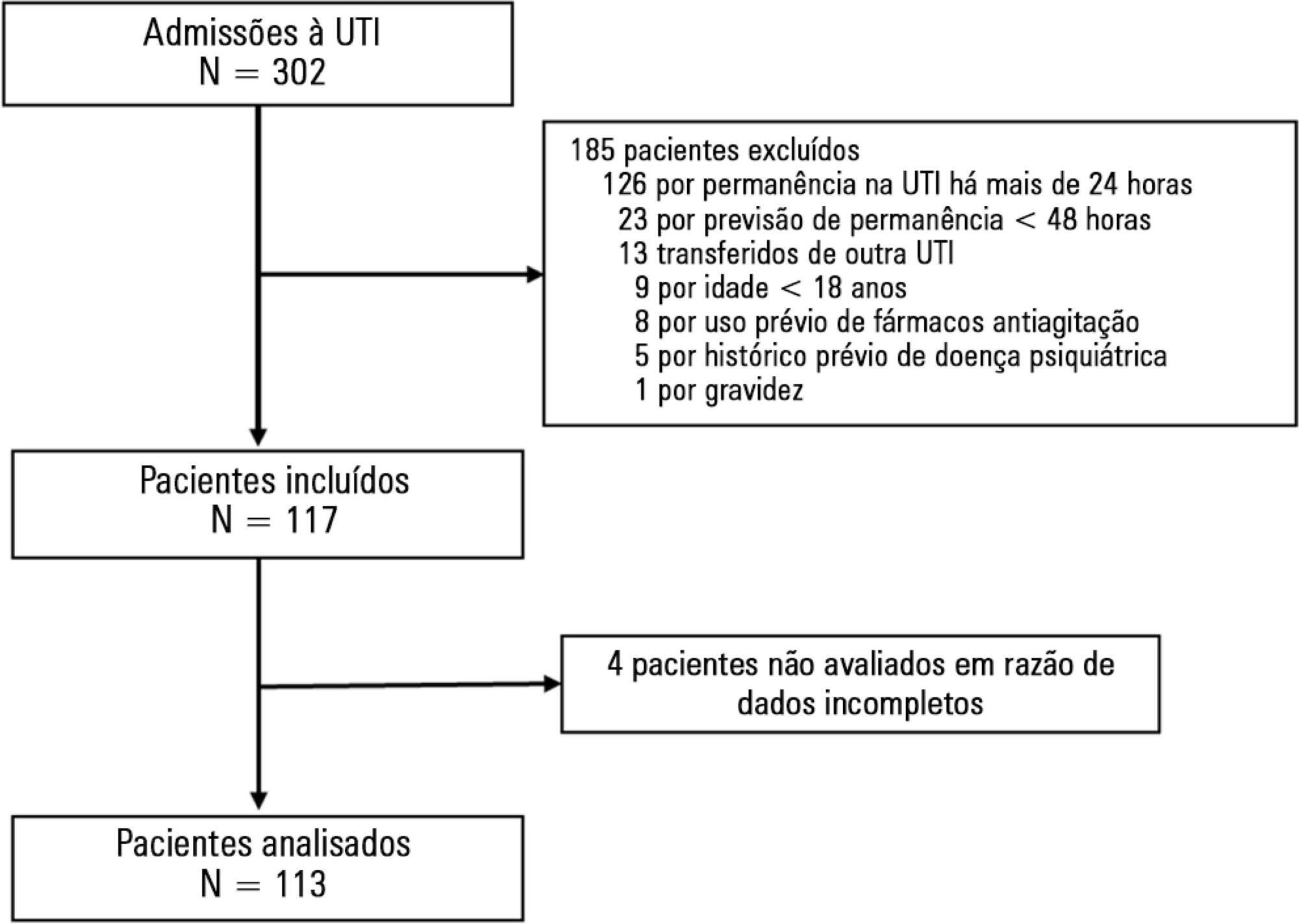
Methods:
This single-center prospective cohort study included all patients older than 18 years with a predicted stay > 48 hours within the first 24 hours of intensive care unit admission. Agitation was defined as a Richmond Agitation Sedation Scale score ≥ +2, an episode of agitation or the use of a specific medication recorded in patient charts.
Results:
Agitation occurred in 31.8% of the 113 patients. Multivariate analysis showed that delirium [OR = 24.14; CI95% 5.15 – 113.14; p < 0.001], moderate or severe pain [OR = 5.74; CI95% 1.73 - 19.10; p = 0.004], mechanical ventilation [OR = 10.14; CI95% 2.93 - 35.10; p < 0.001], and smoking habits [OR = 4.49; CI95% 1.33 - 15.17; p = 0.015] were independent factors for agitation, while hyperlactatemia was associated with a lower risk [OR = 0.169; CI95% 0.04 - 0.77; p = 0.021]. Agitated patients had fewer mechanical ventilation-free days at day 7 (p = 0.003).
Conclusion:
The incidence of agitation in the first 7 days after admission to the intensive care unit was high. Delirium, moderate/severe pain, mechanical ventilation, and smoking habits were independent risk factors. Agitated patients had fewer ventilator-free days in the first 7 days.
-
Original Articles
Swallowing rehabilitation of dysphagic tracheostomized patients under mechanical ventilation in intensive care units: a feasibility study
Rev Bras Ter Intensiva. 2015;27(1):64-71
Abstract
Original ArticlesSwallowing rehabilitation of dysphagic tracheostomized patients under mechanical ventilation in intensive care units: a feasibility study
Rev Bras Ter Intensiva. 2015;27(1):64-71
DOI 10.5935/0103-507X.20150011
Views0Objective:
The aim of the present study was to assess the feasibility of the early implementation of a swallowing rehabilitation program in tracheostomized patients under mechanical ventilation with dysphagia.
Methods:
This prospective study was conducted in the intensive care units of a university hospital. We included hemodynamically stable patients under mechanical ventilation for at least 48 hours following 48 hours of tracheostomy and with an appropriate level of consciousness. The exclusion criteria were previous surgery in the oral cavity, pharynx, larynx and/or esophagus, the presence of degenerative diseases or a past history of oropharyngeal dysphagia. All patients were submitted to a swallowing rehabilitation program. An oropharyngeal structural score, a swallowing functional score and an otorhinolaryngological structural and functional score were determined before and after swallowing therapy.
Results:
We included 14 patients. The mean duration of the rehabilitation program was 12.4 ± 9.4 days, with 5.0 ± 5.2 days under mechanical ventilation. Eleven patients could receive oral feeding while still in the intensive care unit after 4 (2 – 13) days of therapy. All scores significantly improved after therapy.
Conclusion:
In this small group of patients, we demonstrated that the early implementation of a swallowing rehabilitation program is feasible even in patients under mechanical ventilation.
Keywords:Deglutition disorders/rehabilitationDysphagiaIntensive care unitsRespiration, artificialtracheostomySee more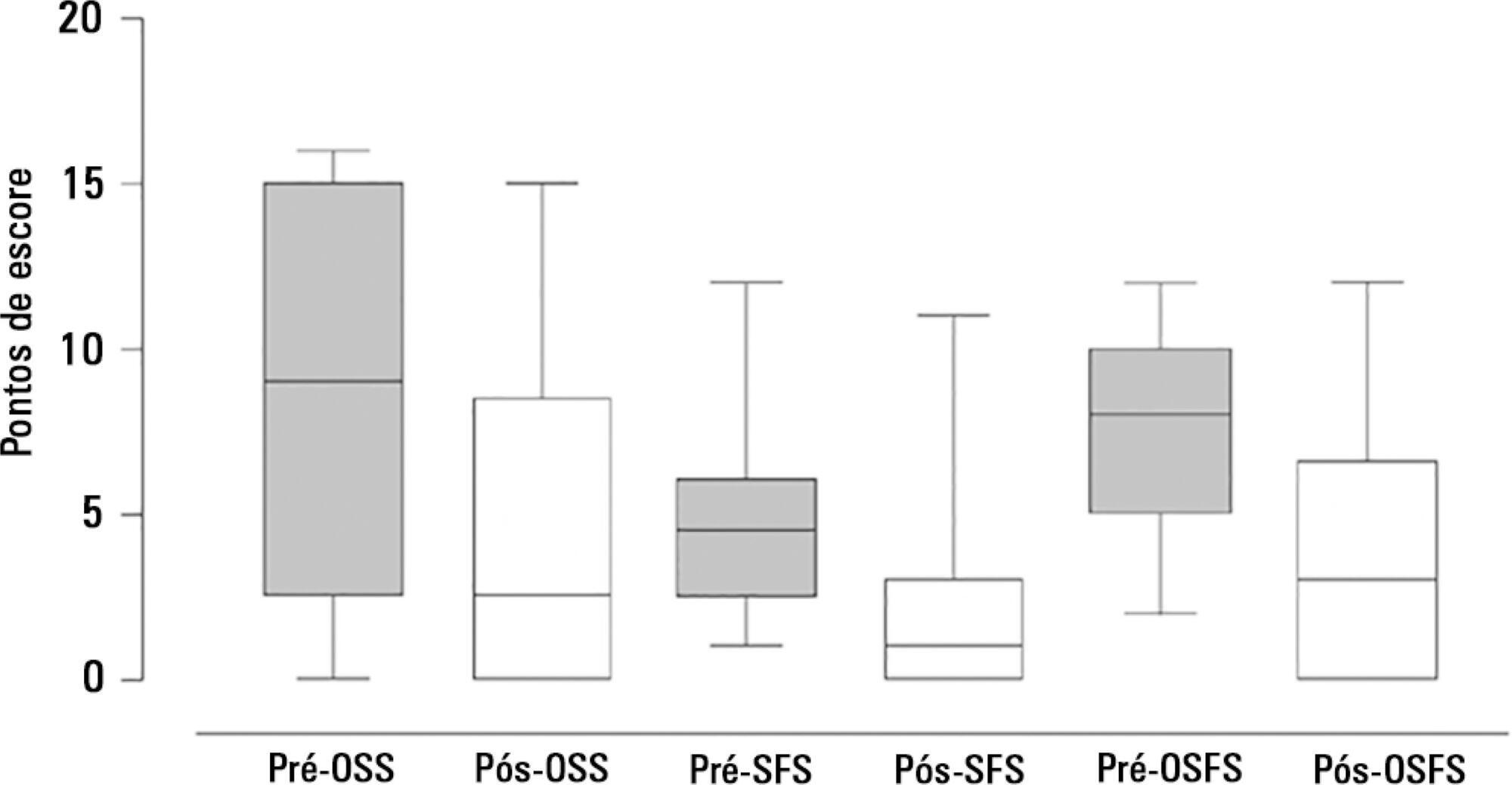
-
Original Articles
Blood transfusions in septic shock: is 7.0g/dL really the appropriate threshold?
Rev Bras Ter Intensiva. 2015;27(1):36-43
Abstract
Original ArticlesBlood transfusions in septic shock: is 7.0g/dL really the appropriate threshold?
Rev Bras Ter Intensiva. 2015;27(1):36-43
DOI 10.5935/0103-507X.20150007
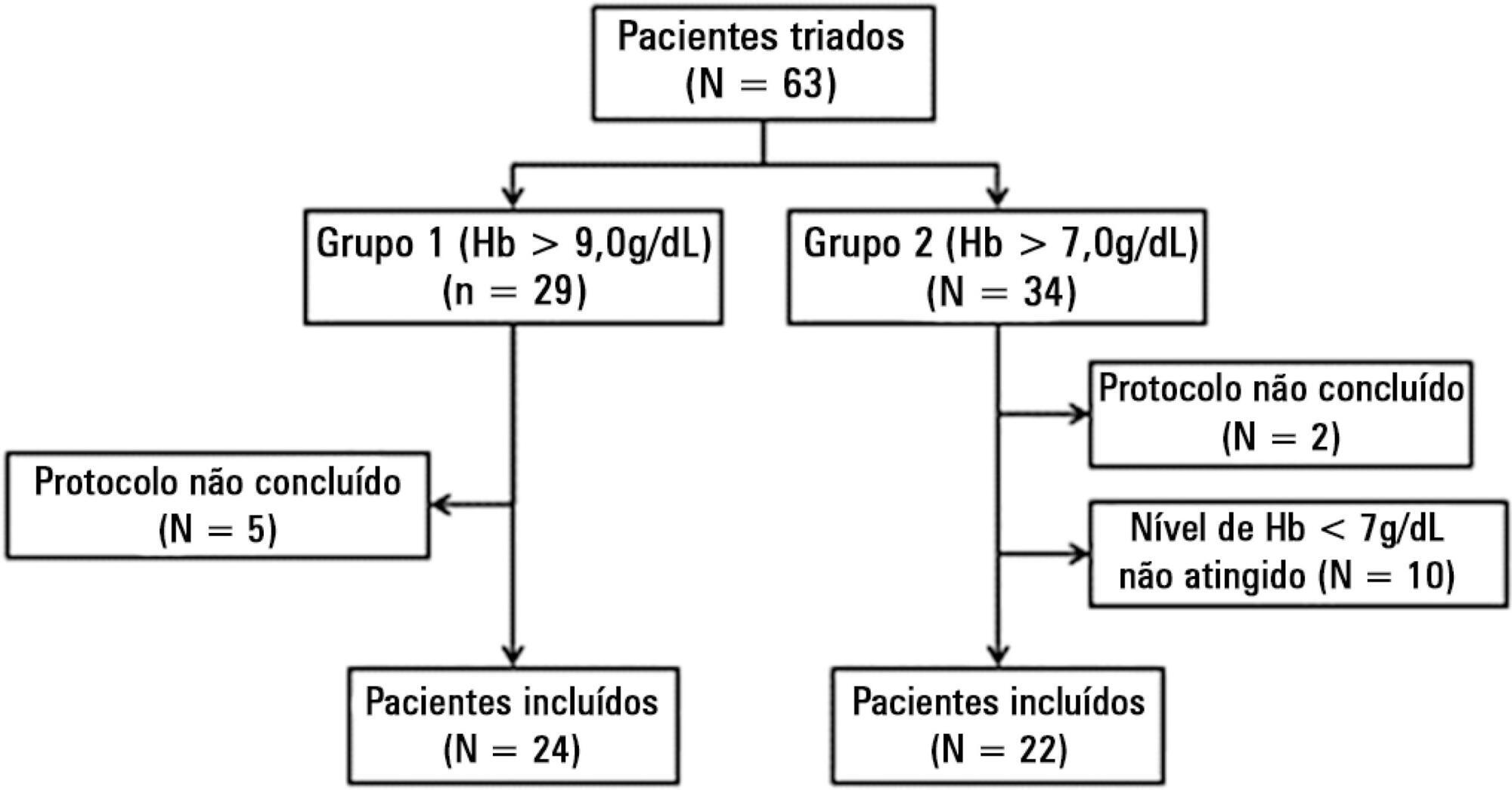
Views0See moreObjective:
To evaluate the immediate effects of red blood cell transfusion on central venous oxygen saturation and lactate levels in septic shock patients with different transfusion triggers.
Methods:
We included patients with a diagnosis of septic shock within the last 48 hours and hemoglobin levels below 9.0g/dL Patients were randomized for immediate transfusion with hemoglobin concentrations maintained above 9.0g/dL (Group Hb9) or to withhold transfusion unless hemoglobin felt bellow 7.0g/dL (Group Hb7). Hemoglobin, lactate, central venous oxygen saturation levels were determined before and one hour after each transfusion.
Results:
We included 46 patients and 74 transfusions. Patients in Group Hb7 had a significant reduction in median lactate from 2.44 (2.00 – 3.22) mMol/L to 2.21 (1.80 – 2.79) mMol/L, p = 0.005, which was not observed in Group Hb9 [1.90 (1.80 – 2.65) mMol/L to 2.00 (1.70 – 2.41) mMol/L, p = 0.23]. Central venous oxygen saturation levels increased in Group Hb7 [68.0 (64.0 – 72.0)% to 72.0 (69.0 – 75.0)%, p < 0.0001] but not in Group Hb9 [72.0 (69.0 - 74.0)% to 72.0 (71.0 - 73.0)%, p = 0.98]. Patients with elevated lactate or central venous oxygen saturation < 70% at baseline had a significant increase in these variables, regardless of baseline hemoglobin levels. Patients with normal values did not show a decrease in either group.
Conclusion:
Red blood cell transfusion increased central venous oxygen saturation and decreased lactate levels in patients with hypoperfusion regardless of their baseline hemoglobin levels. Transfusion did not appear to impair these variables in patients without hypoperfusion.
-
Original Article
Is venous blood drawn from femoral access adequate to estimate the central venous oxygen saturation and arterial lactate levels in critically ill patients?
Rev Bras Ter Intensiva. 2015;27(4):340-346
Abstract
Original ArticleIs venous blood drawn from femoral access adequate to estimate the central venous oxygen saturation and arterial lactate levels in critically ill patients?
Rev Bras Ter Intensiva. 2015;27(4):340-346
DOI 10.5935/0103-507X.20150058
Views0ABSTRACT
Objectives:
The purpose of this study was to test if venous blood drawn from femoral access can be used to estimate the central venous oxygen saturation and arterial lactate levels in critically ill patients.
Methods:
Bland-Altman analysis and Spearman correlations were used to compare the femoral venous oxygen saturation and central venous oxygen saturation as well as arterial lactate levels and femoral lactate. A pre-specified subgroup analysis was conducted in patients with signs of hypoperfusion. In addition, the clinical agreement was also investigated.
Results:
Blood samples were obtained in 26 patients. In 107 paired samples, there was a moderate correlation (r = 0.686, p < 0.0001) between the central venous oxygen saturation and femoral venous oxygen saturation with a bias of 8.24 ± 10.44 (95% limits of agreement: -12.23 to 28.70). In 102 paired samples, there was a strong correlation between the arterial lactate levels and femoral lactate levels (r = 0.972, p < 0.001) with a bias of -2.71 ± 9.86 (95% limits of agreement: -22.03 to 16.61). The presence of hypoperfusion did not significantly change these results. The clinical agreement for venous saturation was inadequate, with different therapeutic decisions in 22.4% of the situation; for lactate, this was the case only in 5.2% of the situations.
Conclusion:
Femoral venous oxygen saturation should not be used as a surrogate of central venous oxygen saturation. However, femoral lactate levels can be used in clinical practice, albeit with caution.
Keywords:Central venous pressure/physiologyFemoral vein/physiologyLactatesOxygen consumption/physiologySee more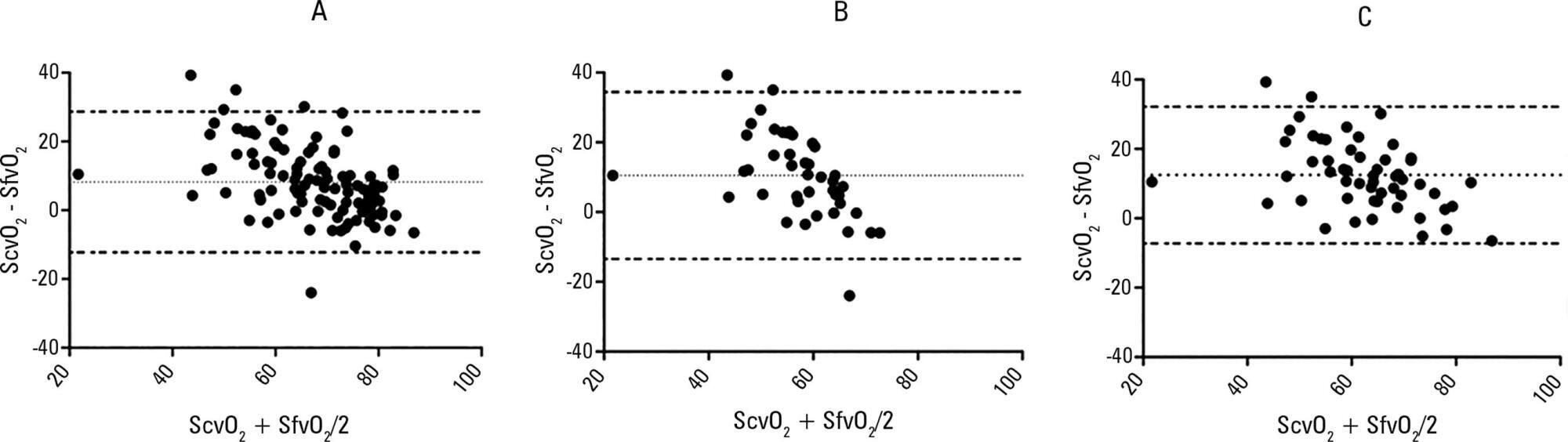
-
Original Article
Serum concentrations of vitamin D and organ dysfunction in patients with severe sepsis and septic shock
Rev Bras Ter Intensiva. 2015;27(4):376-382
Abstract
Original ArticleSerum concentrations of vitamin D and organ dysfunction in patients with severe sepsis and septic shock
Rev Bras Ter Intensiva. 2015;27(4):376-382
DOI 10.5935/0103-507X.20150063
Views0See moreABSTRACT
Objectives:
To evaluate the serum concentrations of vitamin D and their variations in patients with severe sepsis or septic shock and in control subjects upon admission and after 7 days of hospitalization in the intensive care unit and to correlate these concentrations with the severity of organ dysfunction.
Methods:
This case-control, prospective, observational study involved patients aged > 18 years with severe sepsis or septic shock paired with a control group. Serum vitamin D concentrations were measured at inclusion (D0) and on the seventh day after inclusion (D7). Severe deficiency was defined as vitamin D levels < 10ng/ml, deficiency as levels between 10 and 20ng/ml, insufficiency as levels between 20 and 30ng/ml, and sufficiency as levels ≥ 30ng/mL. We considered a change to a higher ranking, together with a 50% increase in the absolute concentration, to represent an improvement.
Results:
We included 51 patients (26 with septic shock and 25 controls). The prevalence of vitamin D concentration ≤ 30ng/ml was 98%. There was no correlation between the serum concentration of vitamin D at D0 and the SOFA score at D0 or D7 either in the general population or in the group with septic shock. Patients with improvement in vitamin D deficiency had an improved SOFA score at D7 (p = 0.013).
Conclusion:
In the population studied, patients with septic shock showed improvement in the serum concentrations of vitamin D on the seventh day compared with the controls. We also found a correlation between higher vitamin D concentrations and a greater decrease in the severity of organ dysfunction.
-
Original Articles
Impact of a continuous education program on the quality of assistance offered by intensive care physiotherapy
Rev Bras Ter Intensiva. 2014;26(1):7-13
Abstract
Original ArticlesImpact of a continuous education program on the quality of assistance offered by intensive care physiotherapy
Rev Bras Ter Intensiva. 2014;26(1):7-13
DOI 10.5935/0103-507X.20140002
Views0Objective:
To evaluate the role of quality indicators and adverse events registering in the quality assessment of intensive care physiotherapy and to evaluate the impact of implementing protocolized care and professional training in the quality improvement process.
Methods:
A prospective before-after study was designed to assess 15 indicators of the quality of care. Baseline compliance and adverse events were collected before and after the implementation of treatment protocols and staff training.
Results:
Eighty-nine patients admitted, being 48 in the pre-intervention period and 41 in the post-intervention period with a total of 1246 and 1191 observations respectively. Among the indicators related to the global population, there was a significant improvement in chest x-ray control, multidisciplinary rounds and shift changes as well as in compliance with these decisions. Indicators related to the population under mechanical ventilation, obtained by direct observation at bedside, showed a significant improvement in the compliance with the tidal volume of 6-8mL/Kg, plateau pressure <30cmH2O, adequate mechanical ventilation alarm setting, mechanical ventilation humidification control, adequate humidification line exchange and orotracheal tube position. Among the mechanical ventilation indicators collected through the physiotherapy records, there was significantly improved compliance with the predicted tidal volume registry and cuff pressure registry. There was a significant reduction in the number of adverse events. There was no impact on intensive care unit mortality, length of stay, duration of mechanical ventilation and ventilator-free days.
Conclusion:
It is possible to measure the quality of physiotherapy care using indicators of quality control. The implementation of care protocols and training of the professionals can improve team performance.
Keywords:Education, continuingIndicators of health serviceIntensive carePhysical therapy modalitiesQuality improvementQuality managementRespiratory therapySee more
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




