Abstract
Rev Bras Ter Intensiva. 2013;25(2):130-136
DOI 10.5935/0103-507X.20130024
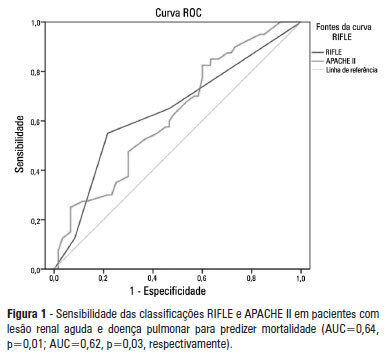
OBJECTIVE: To examine the factors associated with acute kidney injury and outcome in patients with lung disease. METHODS: A prospective study was conducted with 100 consecutive patients admitted to a respiratory intensive care unit in Fortaleza (CE), Brazil. The risk factors for acute kidney injury and mortality were investigated in a group of patients with lung diseases. RESULTS: The mean age of the study population was 57 years, and 50% were male. The incidence of acute kidney injury was higher in patients with PaO2/FiO2<200 mmHg (54% versus 23.7%; p=0.02). Death was observed in 40 cases and the rate of mortality of the acute kidney injury group was higher (62.8% versus 27.6%; p=0.01). The independent factor that was found to be associated with acute kidney injury was PaO2/FiO2<200 mmHg (p=0.01), and the independent risk factors for death were PEEP at admission (OR: 3.6; 95%CI: 1.3-9.6; p=0.009) and need for hemodialysis (OR: 7.9; 95%CI: 2.2-28.3; p=0.001). CONCLUSION: There was a higher mortality rate in the acute kidney injury group. Increased mortality was associated with mechanical ventilation, high PEEP, urea and need for dialysis. Further studies must be performed to better establish the relationship between kidney and lung injury and its impact on patient outcome.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):12-16
DOI 10.1590/S0103-507X2013000100004
OBJECTIVE: This study aimed to evaluate the outcomes for patients with lung cancer admitted to intensive care units and assess their clinical and demographic profiles. METHODS: Retrospective, analytical, observational study, wherein the outcomes for patients diagnosed with lung cancer admitted to the intensive care unit of university hospital from January 2010 until February 2011 were evaluated. RESULTS: Thirty-four patients' medical records were included. Twenty-six (76.5%) patients received some type of ventilatory support, of whom 21 (61.8%) used invasive mechanical ventilation and 11 (32.4%) used noninvasive ventilation at some point during their stay at the intensive care unit. Regarding mortality, 12 (35.3%) patients died during hospitalization at the intensive care unit, totaling 15 (44.1%) deaths during the entire hospitalization period; 19 (55.9%) patients were discharged from the hospital. The analysis of the variables showed that the patients who died had remained on invasive mechanical ventilation for a longer period 5.0 (0.25 to 15.0) days than the survivors (1.0 (0 to 1.0) days) (p=0.033) and underwent dialysis during their stay at the intensive care unit (p=0.014). CONCLUSIONS: The mortality of patients with lung cancer admitted to the intensive care unit is associated with the time spent on invasive mechanical ventilation and the need for dialysis.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):25-31
DOI 10.1590/S0103-507X2013000100006
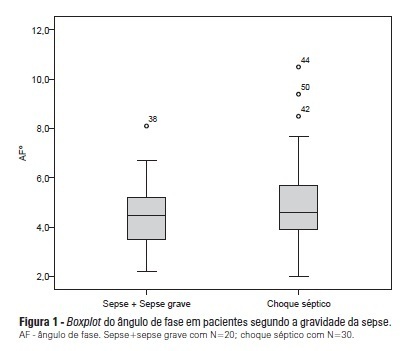
OBJECTIVE: To calculate the values of the phase angle of septic patients using bioelectrical impedance analysis, correlate the values with clinical and biochemical variables, and compare them to reference values. METHODS: Cohort study conducted with 50 septic patients aged ≥18 years old, admitted to intensive care units, and assessed according to prognostic indexes (APACHE II and SOFA), clinical progression (mortality, severity of sepsis, length of stay in intensive care unit), biochemical parameters (albumin and C-reactive protein), and the phase angle. RESULTS: The average age of the sample was 65.6±16.5 years. Most patients were male (58%) and suffering from septic shock (60%). The average APACHE II and SOFA scores were 22.98±7.1 and 7.5±3.4, respectively. The patients who survived stayed nine days on average (five to 13) in the intensive care unit, and the mortality rate was 30%. The average value of the phase angle was 5.4±2.6° in the total sample and was smaller among the females compared with the males (p=0.01). The phase angle measures did not exhibit an association with the severity of the sepsis, mortality, gender, and age or correlate with the length of hospitalization or the biochemical parameters. The participants' phase angle values adjusted per gender and age were 1.1 to 1.9 times lower compared with the values for a normal population. CONCLUSION: The average value of the phase angle of septic patients was lower compared with the reference values for a healthy population. The phase angle measures did not exhibit association with the clinical and biochemical variables, which might be explained by the sample homogeneity.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):352-356
DOI 10.1590/S0103-507X2012000400010
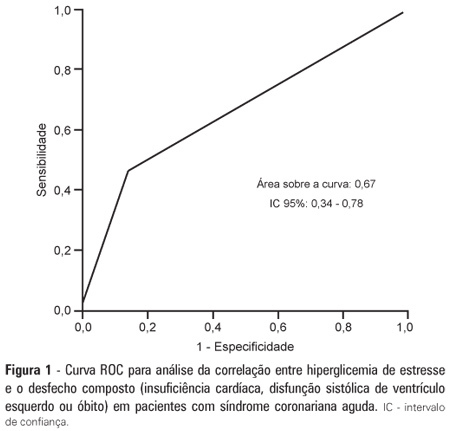
OBJECTIVE: To demonstrate the prevalence of stress hyperglycemia in a cohort of patients with acute coronary syndrome and to determine the correlation of stress hyperglycemia with death, heart failure and/or left ventricular systolic dysfunction during the intrahospital phase. METHODS: A prospective initial cohort study of hospitalized patients with acute coronary syndrome with or without ST segment elevation. The groups were compared to demonstrate the correlation between stress hyperglycemia and cardiovascular events. The chi-square test or Fisher's exact test and student's t-test were used to compare the groups with and without stress hyperglycemia. The variables with p<0.20 in the univariate analysis were submitted to logistic regression. RESULTS: In total, 363 patients with an average age of 12.45 ± 62.06 were studied. There was a predominance of males (64.2%). In total, 96 patients (26.4%) presented with stress hyperglycemia. There were no differences between the groups with or without stress hyperglycemia. The area under the ROC curve was 0.67 for the relationship between stress hyperglycemia and the composite outcome heart failure, left ventricular systolic dysfunction or death at the end of the hospital admission. The ROC curve proved that stress hyperglycemia was the predictor of the composite outcome (death, heart failure and/or ventricular dysfunction). The multivariate analysis did not indicate age, stress hyperglycemia or admission heart rate as risk factors. CONCLUSION: Stress hyperglycemia was common in the studied sample. In the univariate analysis, the presence of stress hyperglycemia was associated with such events as death, heart failure and/or intrahospital ventricular dysfunction in patients with acute coronary syndrome.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
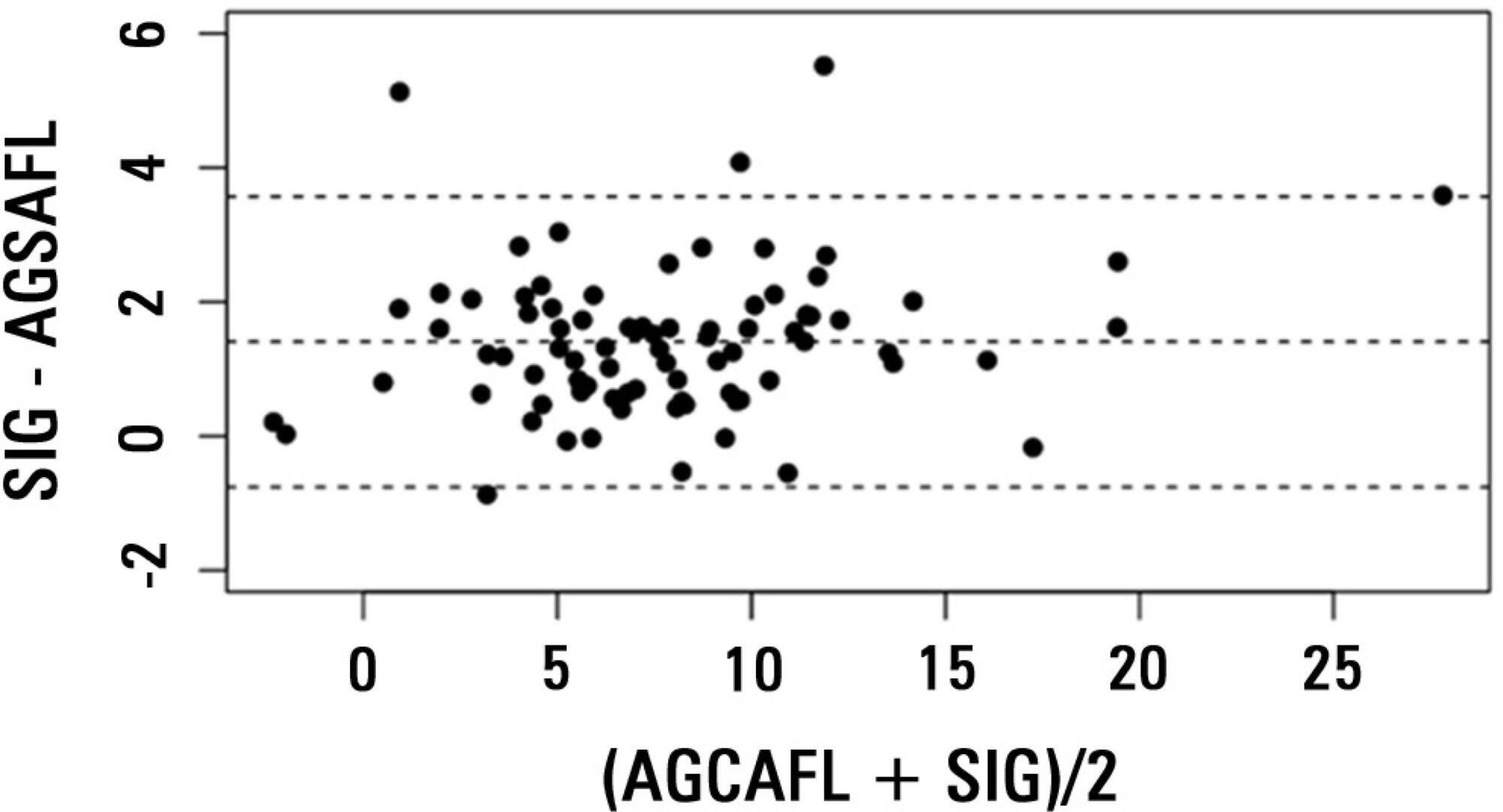
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group - hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):290-296
DOI 10.5935/0103-507X.20130050
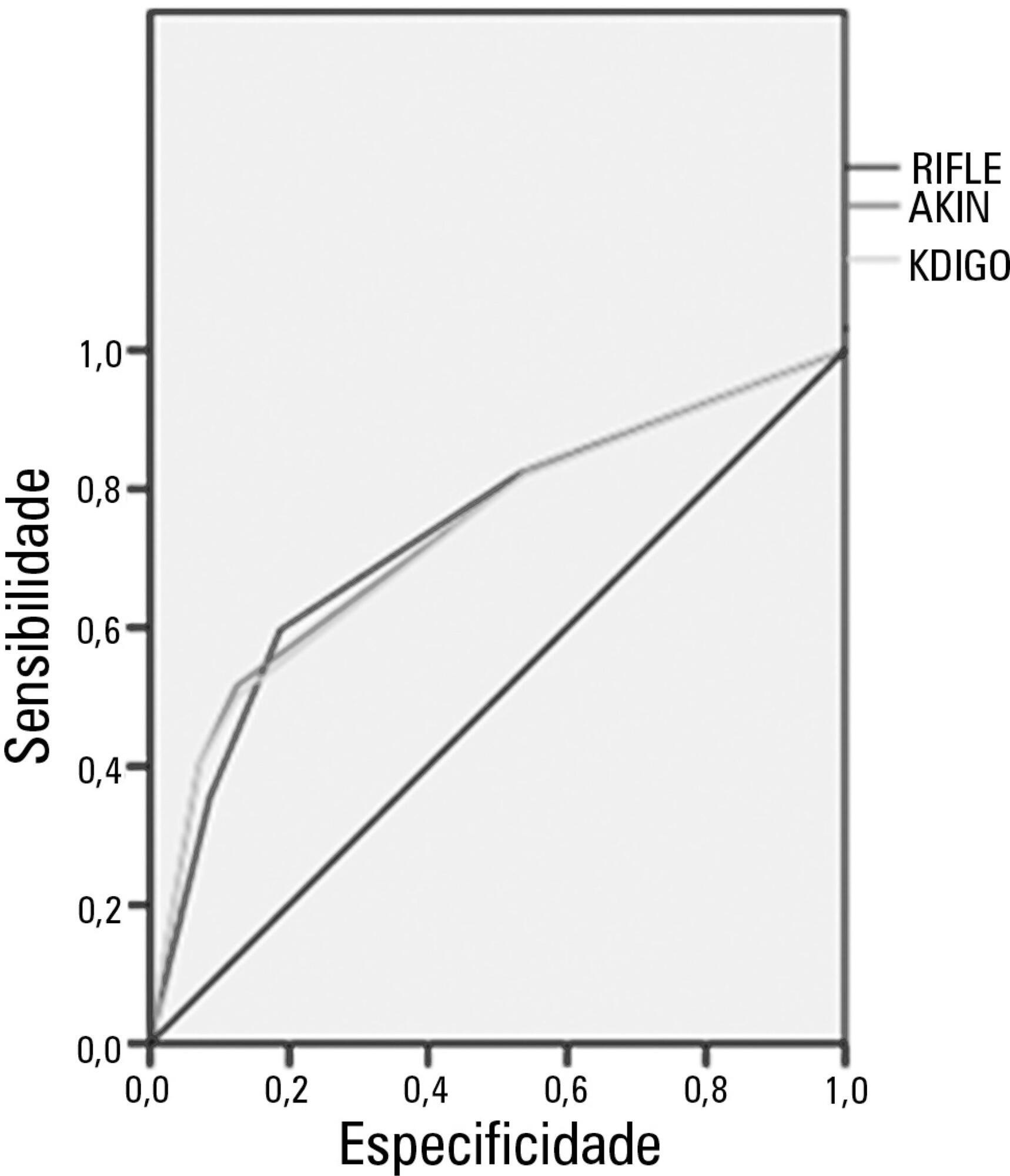
Acute kidney injury is a common complication in critically ill patients, and the RIFLE, AKIN and KDIGO criteria are used to classify these patients. The present study's aim was to compare these criteria as predictors of mortality in critically ill patients.
Prospective cohort study using medical records as the source of data. All patients admitted to the intensive care unit were included. The exclusion criteria were hospitalization for less than 24 hours and death. Patients were followed until discharge or death. Student's t test, chi-squared analysis, a multivariate logistic regression and ROC curves were used for the data analysis.
The mean patient age was 64 years old, and the majority of patients were women of African descent. According to RIFLE, the mortality rates were 17.74%, 22.58%, 24.19% and 35.48% for patients without acute kidney injury (AKI) in stages of Risk, Injury and Failure, respectively. For AKIN, the mortality rates were 17.74%, 29.03%, 12.90% and 40.32% for patients without AKI and at stage I, stage II and stage III, respectively. For KDIGO 2012, the mortality rates were 17.74%, 29.03%, 11.29% and 41.94% for patients without AKI and at stage I, stage II and stage III, respectively. All three classification systems showed similar ROC curves for mortality.
The RIFLE, AKIN and KDIGO criteria were good tools for predicting mortality in critically ill patients with no significant difference between them.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):236-245
DOI 10.1590/S0103-507X2012000300006
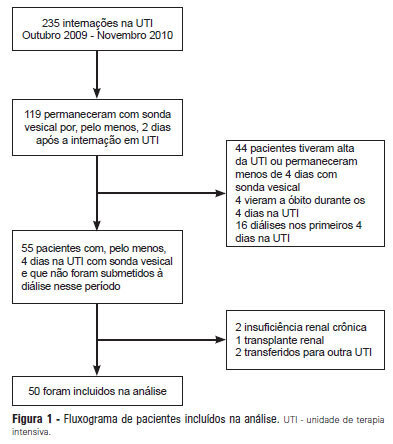
OBJECTIVE: Intensive care unit survivors and non-survivors have distinct acid-base profiles. The kidney's regulation of urinary electrolytes and the urinary strong ion difference plays a major role in acid-base homeostasis. The aim of this study was to evaluate the potential utility of daily spot urinary electrolyte measurement in acid-base and renal function monitoring. METHODS: We prospectively recorded daily plasma acid-base parameters and traditional markers of renal function in parallel with spot urinary electrolyte measurements in patients with urinary catheters admitted to our intensive care unit. Patients who remained in the intensive care unit for at least 4 days with a urinary catheter were included in the study. RESULTS: Of the 50 patients included in the study, 22% died during their intensive care unit stay. The incidence of acute kidney injury was significantly higher in non-survivors during the 4-day observation period (64% vs. 18% in survivors). Urinary chloride and sodium were lower and urinary strong ion difference was higher on day 1 in patients who developed acute kidney injury among both survivors and non-survivors. Both groups had similar urine output, although non-survivors had persistently higher urinary strong ion difference on all days. Survivors had a progressive improvement in metabolic acid-base profile due to increases in the plasma strong ion difference and decreases in weak acids. These changes were concomitant with decreases in urinary strong ion difference. In non-survivors, acid-base parameters did not significantly change during follow-up. CONCLUSIONS: Daily assessment of spot urinary electrolytes and strong ion difference are useful components of acid-base and renal function evaluations in critically ill patients, having distinct profiles between intensive care unit survivors and non-survivors.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):246-251
DOI 10.1590/S0103-507X2012000300007
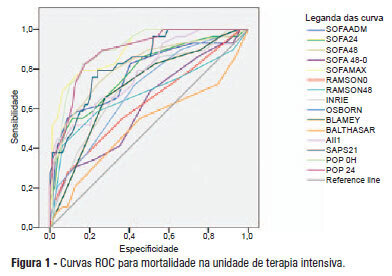
OBJECTIVE: This study compared the general and specific severity indices to assess the prognosis of severe acute pancreatitis at a polyvalent intensive care unit. METHODS: This retrospective study included 108 patients who were diagnosed with severe acute pancreatitis from July 1, 1999 to March 31, 2012. Their demographic and clinical data were collected, and the following severity indices were calculated: Ranson, Osborne, Blamey and Imrie, Balthazar, POP, APACHE II, SAPS II, and SOFA. The discriminative power of these indices with regard to mortality at the intensive care unit and hospital was assessed using the area under the ROC curve. RESULTS: The demographic data of the surviving and deceased patients did not significantly differ at baseline. The mortality rates were 27% and 39% at the intensive care unit and hospital, respectively. The severity indices that exhibited the greatest discriminative power with regard to mortality at the intensive care unit and hospital were the POP 0, POP 24, SOFA (at admission, 24 hours, 48 hours, and discharge), SAPS II, and APACHE II. CONCLUSION: The POP performed better than the other indices (aROC>0.8) at admission and 24 hours later (as originally described). The general physiological dysfunction indices also exhibited reasonable discriminative power (aROC=0.75-0.8), which was unlike the remaining pancreatitis specific indices, whose discriminative power was lower.