Abstract
Rev Bras Ter Intensiva. 2017;29(4):481-489
DOI 10.5935/0103-507X.20170072
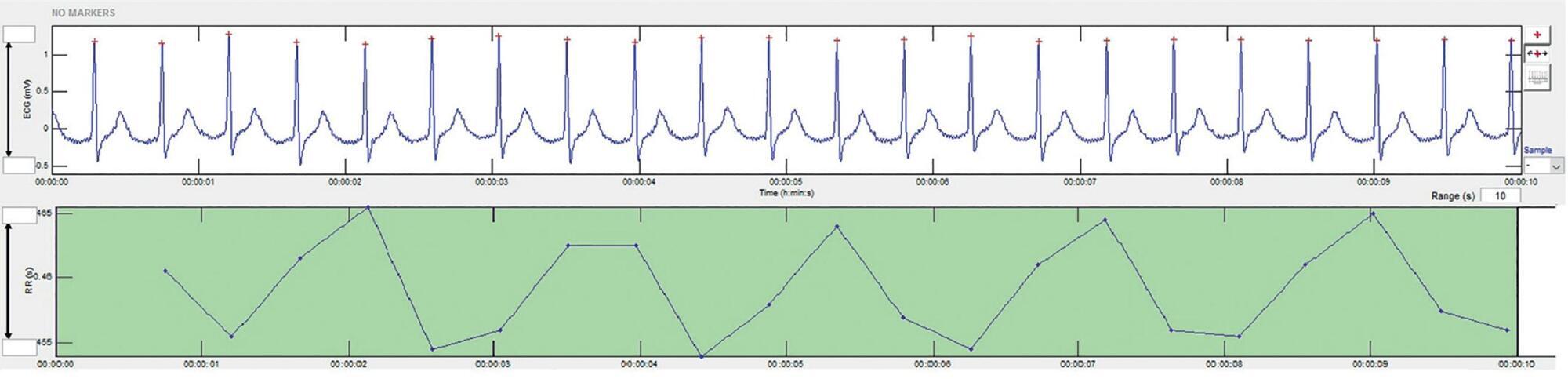
To present a systematic review of the use of autonomic nervous system monitoring as a prognostic tool in intensive care units by assessing heart rate variability.
Literature review of studies published until July 2016 listed in PubMed/Medline and conducted in intensive care units, on autonomic nervous system monitoring, via analysis of heart rate variability as a prognostic tool (mortality study). The following English terms were entered in the search field: ("autonomic nervous system" OR "heart rate variability") AND ("intensive care" OR "critical care" OR "emergency care" OR "ICU") AND ("prognosis" OR "prognoses" OR "mortality").
There was an increased likelihood of death in patients who had a decrease in heart rate variability as analyzed via heart rate variance, cardiac uncoupling, heart rate volatility, integer heart rate variability, standard deviation of NN intervals, root mean square of successive differences, total power, low frequency, very low frequency, low frequency/high frequency ratio, ratio of short-term to long-term fractal exponents, Shannon entropy, multiscale entropy and approximate entropy.
In patients admitted to intensive care units, regardless of the pathology, heart rate variability varies inversely with clinical severity and prognosis.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):179-189
DOI 10.5935/0103-507X.20160019
Lower respiratory tract infections are common and potentially lethal conditions and are a major cause of inadequate antibiotic prescriptions. Characterization of disease severity and prognostic prediction in affected patients can aid disease management and can increase accuracy in determining the need for and place of hospitalization. The inclusion of biomarkers, particularly procalcitonin, in the decision taken process is a promising strategy. This study aims to present a narrative review of the potential applications and limitations of procalcitonin as a prognostic marker in hospitalized patients with lower respiratory tract infections. The studies on this topic are heterogeneous with respect to procalcitonin measurement techniques, cutoff values, clinical settings, and disease severity. The results show that procalcitonin delivers moderate performance for prognostic prediction in patients with lower respiratory tract infections; its predictive performance was not higher than that of classical methods, and knowledge of procalcitonin levels is most useful when interpreted together with other clinical and laboratory results. Overall, repeated measurement of the procalcitonin levels during the first days of treatment provides more prognostic information than a single measurement; however, information on the cost-effectiveness of this procedure in intensive care patients is lacking. The results of studies that evaluated the prognostic value of initial procalcitonin levels in patients with community-acquired pneumonia are more consistent and have greater potential for practical application; in this case, low procalcitonin levels identify those patients with a low risk of adverse outcomes.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):240-246
DOI 10.5935/0103-507X.20150044
To determine the etiology and clinical disease progression variables of sepsis associated with the prognosis of patients admitted to a pediatric intensive care unit.
Prospective and retrospective case series. Data were collected from the medical records of patients diagnosed with sepsis who were admitted to the pediatric intensive care unit of a general hospital from January 2011 to December 2013. Bacteria were identified in blood and fluid cultures. Age, sex, vaccination schedule, comorbidities, prior antibiotic use, clinical data on admission, and complications during disease progression were compared in the survival and death groups at a 5% significance level.
A total of 115 patients, with a mean age of 30.5 months, were included in the study. Bacterial etiology was identified in 40 patients. Altered peripheral perfusion on admission and diagnosis of severe sepsis were associated with complications. A greater number of complications occurred in the group of patients older than 36 months (p = 0.003; odds ratio = 4.94). The presence of complications during hospitalization was associated with death (odds ratio = 27.7). The main etiological agents were Gram-negative bacteria (15/40), Staphylococcus aureus (11/40) and Neisseria meningitidis (5/40).
Gram-negative bacteria and Staphylococcus aureus predominated in the etiology of sepsis among children and adolescents admitted to an intensive care unit. The severity of sepsis and the presence of altered peripheral perfusion on admission were associated with complications. Moreover, the presence of complications was a factor associated with death.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):26-35
DOI 10.5935/0103-507X.20150006
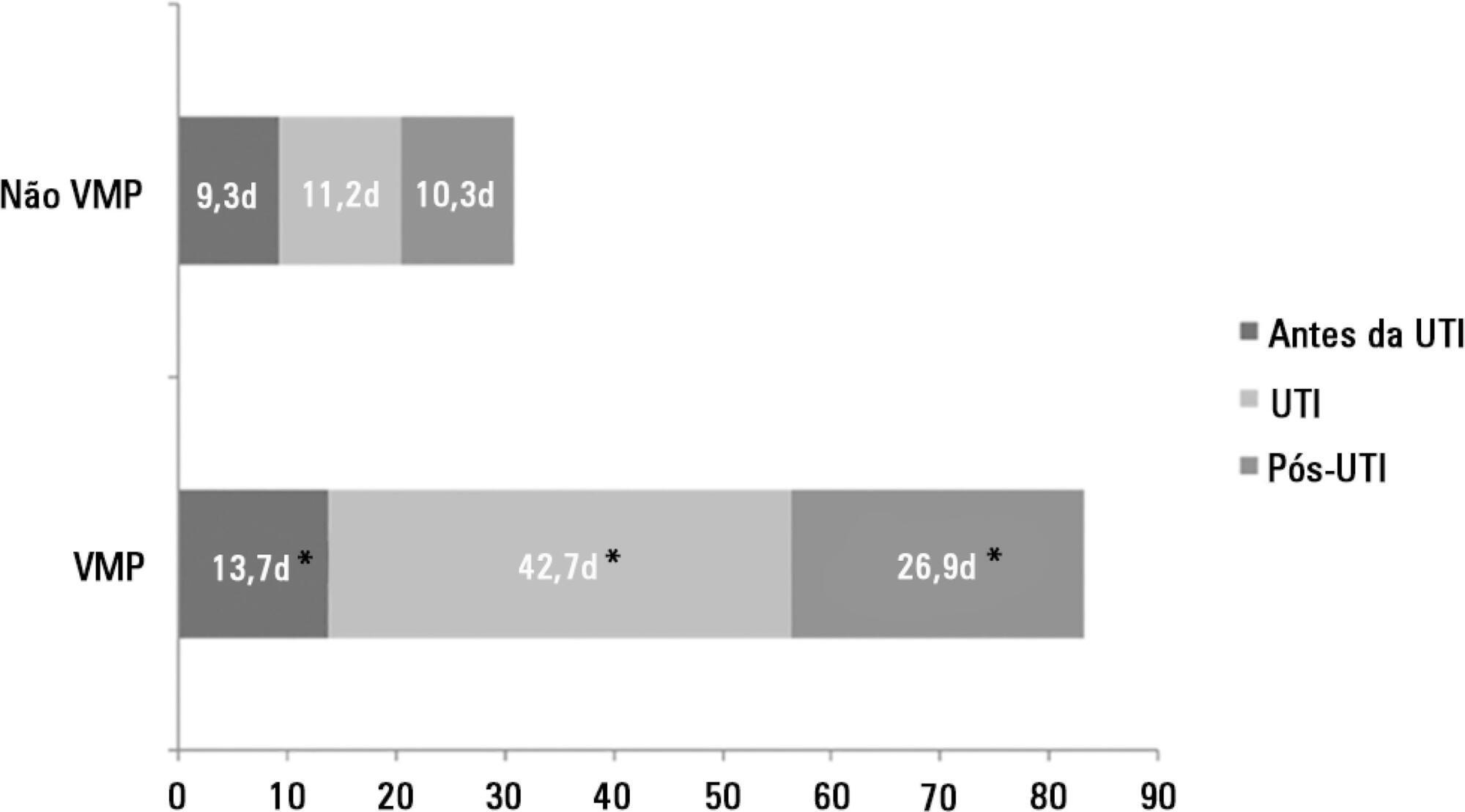
The number of patients who require prolonged mechanical ventilation increased during the last decade, which generated a large population of chronically ill patients. This study established the incidence of prolonged mechanical ventilation in four intensive care units and reported different characteristics, hospital outcomes, and the impact of costs and services of prolonged mechanical ventilation patients (mechanical ventilation dependency ≥ 21 days) compared with non-prolonged mechanical ventilation patients (mechanical ventilation dependency < 21 days).
This study was a multicenter cohort study of all patients who were admitted to four intensive care units. The main outcome measures were length of stay in the intensive care unit, hospital, complications during intensive care unit stay, and intensive care unit and hospital mortality.
There were 5,287 admissions to the intensive care units during study period. Some of these patients (41.5%) needed ventilatory support (n = 2,197), and 218 of the patients met criteria for prolonged mechanical ventilation (9.9%). Some complications developed during intensive care unit stay, such as muscle weakness, pressure ulcers, bacterial nosocomial sepsis, candidemia, pulmonary embolism, and hyperactive delirium, were associated with a significantly higher risk of prolonged mechanical ventilation. Prolonged mechanical ventilation patients had a significant increase in intensive care unit mortality (absolute difference = 14.2%, p < 0.001) and hospital mortality (absolute difference = 19.1%, p < 0.001). The prolonged mechanical ventilation group spent more days in the hospital after intensive care unit discharge (26.9 ± 29.3 versus 10.3 ± 20.4 days, p < 0.001) with higher costs.
The classification of chronically critically ill patients according to the definition of prolonged mechanical ventilation adopted by our study (mechanical ventilation dependency ≥ 21 days) identified patients with a high risk for complications during intensive care unit stay, longer intensive care unit and hospital stays, high death rates, and higher costs.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):141-148
DOI 10.5935/0103-507X.20150025
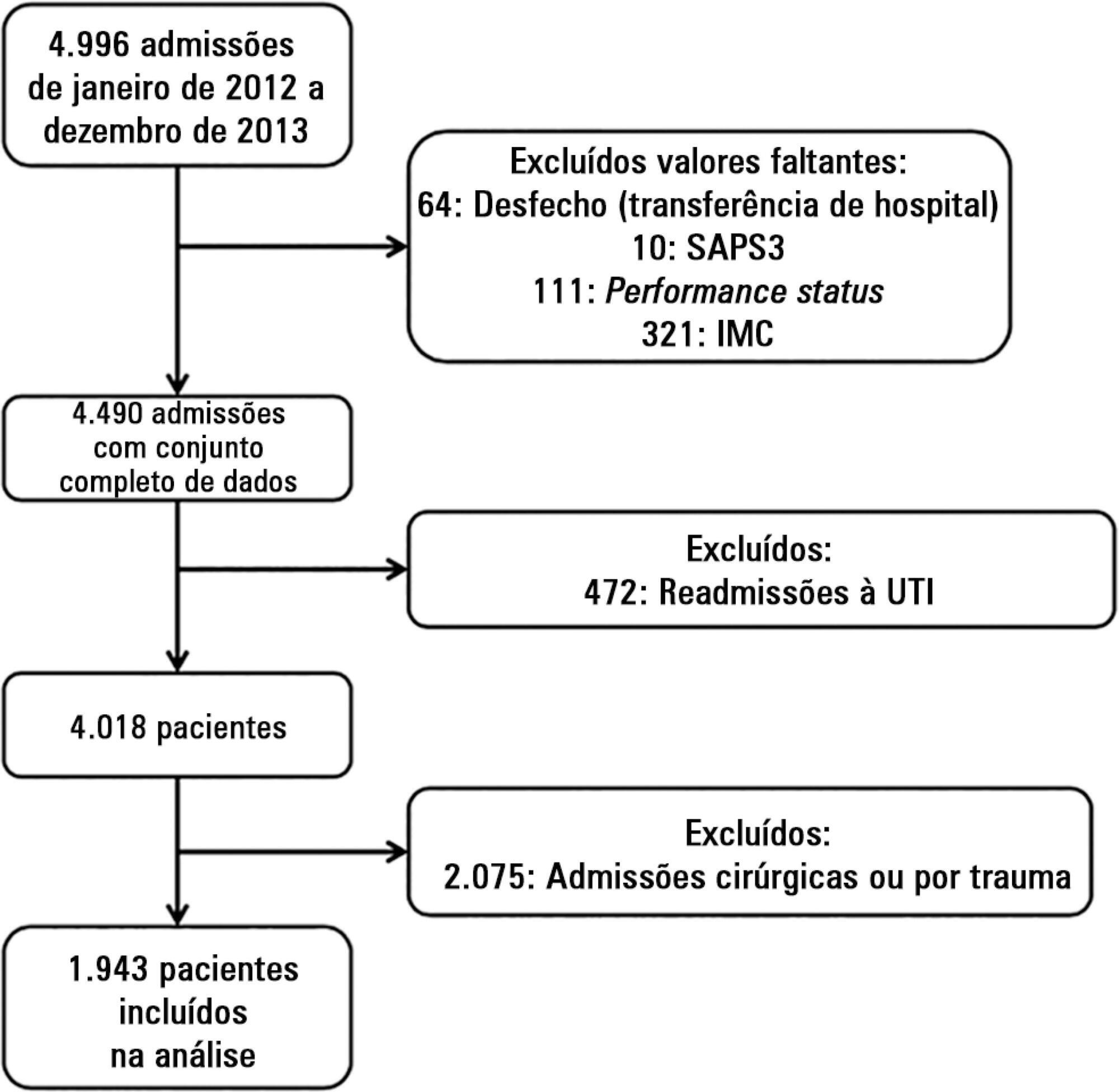
To evaluate the impact of body mass index on the short-term prognosis of non-surgical critically ill patients while controlling for performance status and comorbidities.
We performed a retrospective analysis on a two-year single-center database including 1943 patients. We evaluated the impact of body mass index on hospital mortality using a gradient-boosted model that also included comorbidities and was assessed by Charlson’s comorbidity index, performance status and illness severity, which was measured by the SAPS3 score. The SAPS3 score was adjusted to avoid including the same variable twice in the model. We also assessed the impact of body mass index on the length of stay in the hospital after intensive care unit admission using multiple linear regressions.
A low value (< 20kg/m2) was associated with a sharp increase in hospital mortality. Mortality tended to subsequently decrease as body mass index increased, but the impact of a high body mass index in defining mortality was low. Mortality increased as the burden of comorbidities increased and as the performance status decreased. Body mass index interacted with the impact of SAPS3 on patient outcome, but there was no significant interaction between body mass index, performance status and comorbidities. There was no apparent association between body mass index and the length of stay at the hospital after intensive care unit admission.
Body mass index does appear to influence the shortterm outcomes of critically ill medical patients, who are generally underweight. This association was independent of comorbidities and performance status.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):176-182
DOI 10.5935/0103-507X.20140026
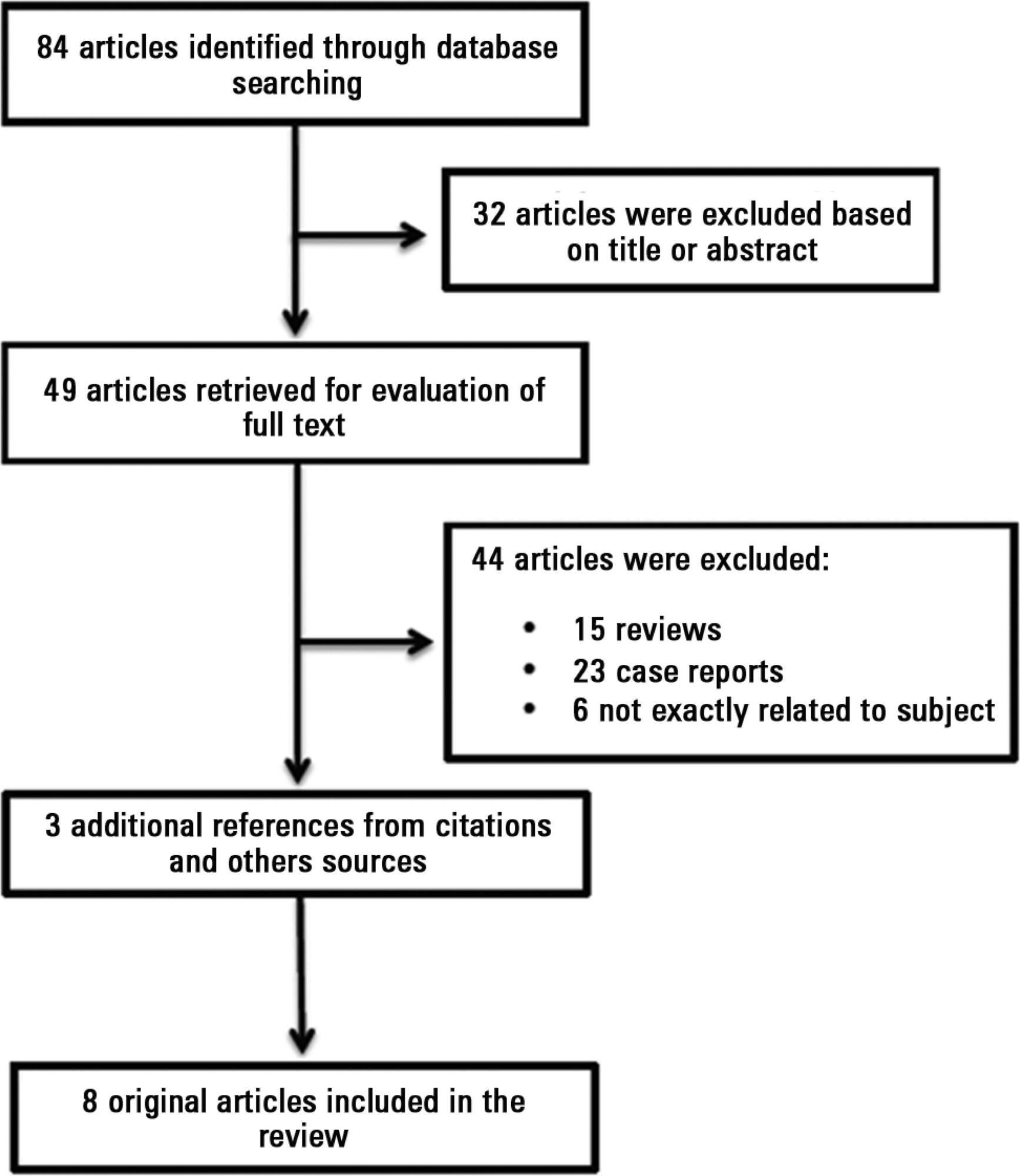
Antiphospholipid antibodies are responsible for a wide spectrum of clinical manifestations. Venous, arterial and microvascular thrombosis and severe catastrophic cases account for a large morbidly/mortality. Through the connection between the immune, inflammatory and hemostatic systems, it is possible that these antibodies may contribute to the development of organ dysfunction and are associated with poor short and long-term prognoses in critically ill patients. We performed a search of the PubMed/MedLine database for articles written during the period from January 2000 to February 2013 to evaluate the frequency of antiphospholipid antibodies in critically ill patients and their impact on the outcomes of these patients. Only eight original studies involving critically ill patients were found. However, the development of antiphospholipid antibodies in critically ill patients seems to be frequent, but more studies are necessary to clarify their pathogenic role and implications for clinical practice.
Abstract
Rev Bras Ter Intensiva. 2014;26(3):305-312
DOI 10.5935/0103-507X.20140043
The number of studies investigating circulating nucleic acids as potential biomarkers has increased in recent years. The detection of such biomarkers is a minimally invasive alternative for the diagnosis and prognosis of various clinical conditions. The value of circulating DNA levels as a predictive biomarker has been demonstrated in patients suffering from numerous acute pathologies that have a high risk of intensive care needs and in-hospital deaths. The mechanism by which circulating DNA levels increase in patients with these conditions remains unclear. In this review, we focused on the potential use of this biomarker for prognosis prediction in critically ill and trauma patients. The literature review was performed by searching MedLine using PubMed in the English language.