Abstract
Rev Bras Ter Intensiva. 2010;22(2):166-174
DOI 10.1590/S0103-507X2010000200011
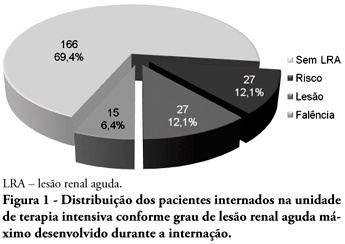
OBJECTIVES: Acute kidney injury is characterized by sudden and generally revertible renal function impairment involving inability to maintain homeostasis. In pediatrics, the main causes of acute kidney injury are sepsis, use of nephrotoxic drugs and renal ischemia in critically ill patients. The incidence of acute kidney injury in these patients ranges from 20 to 30%, resulting in increased morbid-mortality, a 40 to 90% rate. This study aimed to evaluate the incidence of acute kidney injury in intensive care unit patients, to categorize the severity of the acute kidney injury according to the Pediatric Risk, Injury, Failure, Loss, End-Stage (pRIFLE), examine the relationship between the acute kidney injury and severity using the Pediatric Index of Mortality (PIM) and to analyze outcome predictors. METHODS: A prospective study of the patients admitted to the intensive care unit of Hospital Infantil Joana de Gusmão - Florianópolis / SC - Brazil was conducted between July 2008 and January 2009. Were evaluated daily the urine output and serum creatinine, and the patients were categorized according to the pRIFLE criteria. RESULTS: During the follow-up period, 235 children were admitted. The incidence of acute kidney injury was 30.6%, and the maximal pRIFLE score during hospitalization was 12.1% for R, 12.1% for I and 6.4% for F. The mortality rate was 12.3%. The patients who developed acute kidney injury had a ten times bigger risk of death versus the not exposed patients. CONCLUSIONS: Acute kidney injury is frequent in critically ill patients. Early diagnosis and prompt and appropriate therapy for each clinical aspect may change this condition's course and severity, and reduce the patients' morbidity and mortality.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):27-32
DOI 10.1590/S0103-507X2010000100006
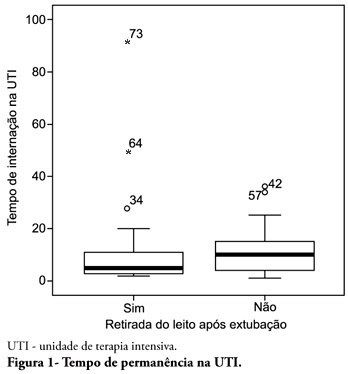
OBJECTIVE: To describe the withdrawal of the bed frequency in mechanic ventilation patients and its impact on mortality and length of stay in the intensive care unit. METHODS: This was a retrospective cohort study in mechanical ventilation patients. Clinical and epidemiological variables, withdrawal of bed related motor therapy, intensive care unit length of stay and mortality were evaluated. RESULTS: We studied 91 patients, mean age of 62.5± 18.8 years, predominantly female (52%) and mean intensive care unit length of stay of 07 days (95% CI, 8-13 days). Considering the withdrawal of the bed or not, no difference was observed between groups regarding length of stay in intensive care unit. Patients who were withdrawn of bed had a lower clinical severity. Their mortality rate was 29.7%. The not withdrawn of bed group had higher both actual and expected mortality. CONCLUSIONS: Patients withdrawn of bed following mechanical ventilation discontinuation showed lower mortality. It is suggested that early intensive care unit mobilization and withdrawal of bed should be stimulated.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):18-24
DOI 10.1590/S0103-507X2009000100003
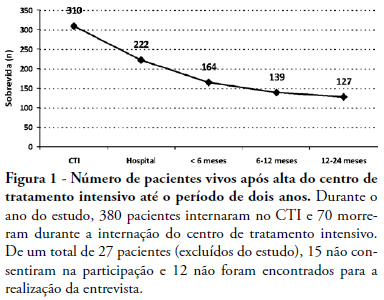
OBJECTIVES: To evaluate mortality and long term quality of life of patients who were discharged from the intensive care unit. METHODS: A prospective cohort, in which all the admitted patients in a intensive care unit (ICU) during 6 months were evaluated and interviewed by telephone after two years of discharge, aiming the completion of two quality of live scales: Karnofsky scale and activities of daily living (ADL) scale. RESULTS: From a total of 380 patients, 100 (26.5%) individuals were alive at the time of interview, 94% living in their homes and 90% without the need for family or specialized care. There was a significant reduction in quality of life of the survivors (Karnofsky pre-ICU = 90±10 vs. Karnofsky after two years = 79±11; p<0.05), although maintaining their functional capacity (ADL pre-ICU = 28±4 vs. ADL after two years = 25±8; p=0.09). This drop in the quality of life occurred mainly to patients who suffered stroke (Karnofsky pre-ICU = 88±7 vs. Karnofsky after two years = 60±15; p<0. 01). CONCLUSION: These preliminary data suggest that the performance of patients after two years of the intensive care discharge is preserved, since they retain the ability to perform self care, except in those with brain damage which shows an inferior quality of life.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):173-177
DOI 10.1590/S0103-507X2008000200010
BACKGROUND AND OBJECTIVES: The debate on efficacy and patient safety related to the use of drotrecogin alfa (DrotAA) is timely, principally due to the negative results observed in clinical studies performed after the PROWESS study, and the economic cost-related impact of the drug on the healthcare system. The aim of this study was to review the main studies on the use of DrotAA in patients with severe sepsis. The focus was on drug efficacy-and patient safety-related issues. CONTENTS: Articles were selected by a MedLine search for studies on the use of DrotAA in patients with sepsis using the following key words: activated protein C; drotrecogin alfa; sepsis; septic shock; Xigris®. Additional references were retrieved from the studies initially selected. CONCLUSIONS: Mortality and bleeding complications associated with the use of DrotAA were more frequent in large observational studies than those reported in randomized trials. In the light of the current knowledge, routine use of DrotAA should be reevaluated until well-designed confirmatory clinical trials can clarify the true efficacy and safety of the drug and help identify the subgroup of patients that can benefit from use of DrotAA. Physicians should be cautious with the rapid transfer of evidences not well-documented, to the guidelines and recommendations practiced in the care and treatment of patients with severe sepsis.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):115-123
DOI 10.1590/S0103-507X2008000200001
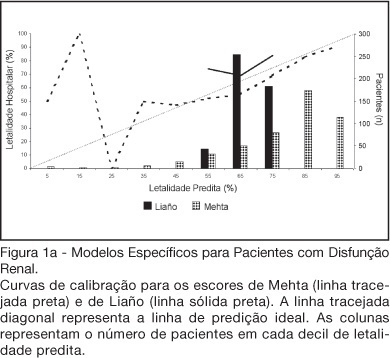
BACKGROUND AND OBJECTIVES: There is no consensus about prognostic scores for use in patients with acute kidney injury (AKI). The aim of this study was to evaluate the performance of six prognostic scores in predicting hospital mortality in patients with AKI and need for renal replacement therapy (RRT). METHODS: Prospective cohort of patients admitted to the intensive care units (ICU) of three tertiary care hospitals that required RRT for AKI over a 32-month period. Patients with end-stage renal disease and those with ICU stay < 24h were excluded. Data from the first 24h of ICU admission were used to calculate SAPS II and APACHE II scores, and data from the first 24h of RRT were used in the calculation of LOD, ODIN, Liaño and Mehta scores. Discrimination was evaluated using the area under ROC curve (AUROC) and calibration using the Hosmer-Lemeshow goodness-of-fit test. The hospital mortality was the end-point of interest. RESULTS: 467 patients were evaluated. Hospital mortality rate was 75%. Mean SAPS II and APACHE II scores were 48.5 ±11.2 and 27.4 ± 6.3 points, and median LOD score was 7 (5-8) points. Except for Mehta score (p = 0.001), calibration was appropriate in all models. However, discrimination was uniformly unsatisfactory; AUROC ranged from 0.60 for ODIN to 0.72 for SAPS II and Mehta scores. In addition, except for Mehta, all models tended to underestimate hospital mortality. CONCLUSIONS: Organ dysfunction, general and renal-specific severity-of-illness scores were inaccurate in predicting outcome in ICU patients in need for RRT.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):52-58
DOI 10.1590/S0103-507X2006000100010
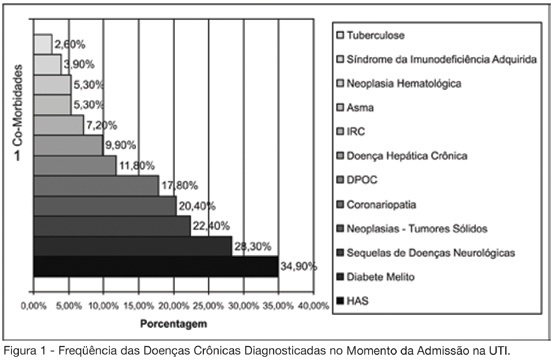
BACKGROUND AND OBJECTIVES: Establish the clinical, epidemiological and laboratorial characteristics of septic patients in an intensive care unit (ICU) of a tertiary care private hospital from Pernambuco, in the northeast of Brazil. METHODS: Cohort study without intervention that included adult patients admitted in the ICU with sepsis or that developed it during ICU stay, during a 6-month period. The patients were followed during all ICU stay period. Laboratory and clinical data were collected after sepsis diagnosis. ICU admission APACHE II score and the SOFA score during the three first days after inclusion in the study were collected. RESULTS: The study included 199 patients, of whom 67.8% were older than 65 years of age. More than a half (56.3%) survived the septic episode, mean APACHE II was 18.2 ± 6.3 and mean SOFA score was 6.3 ± 3.7. The disease related to the admission in ICU was medical in 85.4%, and the majority of patients had a chronic associated disease. In 79.3% the lungs were the source of sepsis and in 40% of patients the etiologic agent of sepsis was isolated. Amongst laboratory tests, thrombocytopenia (platelets < 100.000/mm³) was observed on 20.6%, fibrinogen was elevated (> 300 mg/dL) on 81.7%, and the activity of antithrombin was low (< 70%) on 32.5% of patients. CONCLUSIONS: The epidemiology of sepsis in this study, in a private hospital of Recife, was no different from what was recently described in Southeast and South of Brazil, United States and Europe.
Abstract
Rev Bras Ter Intensiva. 2006;18(1):38-44
DOI 10.1590/S0103-507X2006000100008
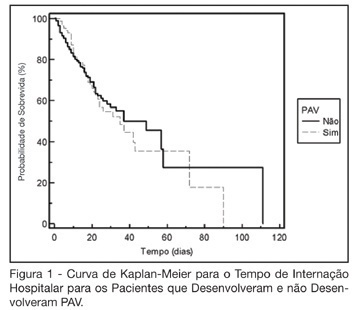
BACKGROUND AND OBJECTIVES: The ventilator-associated pneumonia (VAP) is a severe infection that presents multiple causes which can vary depending on the type of intensive care unit, type of patients, emphasizing the needs for vigilance measures with local data. The aim of this study is to describe the incidence, risk factors and mortality of VAP in patients in a surgical ICU. METHODS: Prospective cohort conducted from January 2004 to January 2005. It was included all the patients in mechanical ventilation, followed daily to collect data about demographics, diagnostic, APACHE II and TISS 28 scores, duration of mechanical ventilation, length of stay, incidence of VAP and mortality. RESULTS: 462 patients were studied; age 57.2 ± 16.6 years, 55% men. The mean APACHE II score was 18.3 and the incidence of VAP was 18.8%. The TISS score at admission OR = 1.050 (IC 95%: 1.003-1.050) and the enteral nutrition OR = 5.609 (IC 3.351-9.388) were factors associated with VAP and the prophylactic use of antibiotics was a factor of protection OR = 0.399 (IC95%: 0.177-0.902). The patients with VAP had longer length of stay in ICU (10.3 ± 10.7 vs 4.9 ± 3.3 days), higher median of duration of mechanical ventilation (4 vs 1 days), higher mean of TISS 28 (24.4 ± 4.6 vs 22.8 ± 4.5), and higher crude mortality (46 vs 28.8%) when compared with the patients without VAP. CONCLUSIONS: VAP was a frequent infection in surgical patients in mechanical ventilation. Enteral nutrition and admission TISS were risk factors and the previous use of antibiotics was protection factor to develop VAP. In our sample the results demonstrate that VAP is associated with higher duration in mechanical ventilation, longer length of stay and higher mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):251-255
DOI 10.1590/S0103-507X2006000300006
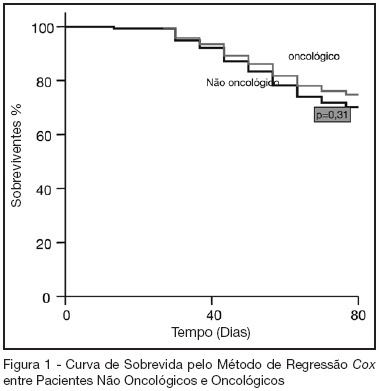
BACKGROUND AND OBJECTIVES: Oncologic diseases are conditions that have influence in the treatment offered to affected patients. The aim of this study was to compare hospitalar outcome of oncologic and non oncologic patients submitted to high risk elective surgery. METHODS: Prospective, observational cohort study realized in an ICU of a tertiary hospital during the period between 04/01/2005 and 07/31/2005. Demographic data, APACHE II and MODS scores and laboratorial and hemodynamic variables were collected and complications like re-intervention need for mechanical ventilation, red blood cell transfusions and pulmonary artery catheter use during the post-operative period were evaluated. All patients were followed until hospital discharge or death. T student and Mann Whitney tests were used to compare numerical variables. Chi-square test was used to compare categorical variables. A p < 0.05 was considered as significant. RESULTS: 119 patients were included in the study. 43 were oncologic and 76 were non-oncologic. 52.9% were female. Mean age was 65.1 ± 14.1 years. Mean APACHE II score was 16.5 ± 5.8 and MODS median was 3 (2-6). Median length of surgery was 5 (3.3-7) hours and ICU and hospital mortality were 10.9% and 25.2%, respectively. Oncologic patients had greater length of hospital stay and length of stay before surgery. These results were statistically significant. Hospital mortality of oncologic patients was not greater than non-oncologic patients (22.4% versus 30.2%, p = 0.32). CONCLUSIONS: In this series, oncologic patients submitted to high risk surgery had the same mortality rate as non-onconlogic patients with similar disease severity.