Abstract
Rev Bras Ter Intensiva. 2006;18(3):268-275
DOI 10.1590/S0103-507X2006000300009
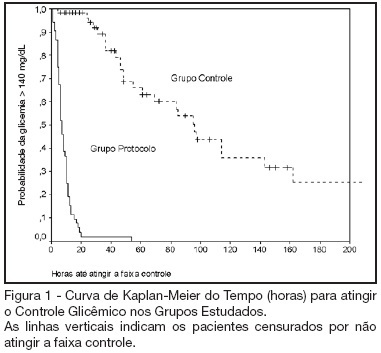
BACKGROUND AND OBJECTIVES: Actually tight glycemic control is a major concern in critical care. The objective of this study was to evaluate effectiveness and safety of Yale insulin infusion protocol in a Brazilian medical and surgical intensive care unit. METHODS: Retrospective, before-after cohort study. Selected end-points were mean blood glucose levels, time-to-reach target range of 80 - 140 mg/dL, and percent of blood glucose in target range and hypoglycemia incidence. RESULTS: Were studied 112 patients: 60 in control group (CG) and 52 in protocol group (PG). Bedside blood glucose was measured 5392 times for a mean value of 131.2 ± 14.7 mg/dL in the PG versus 2485 times for a mean value of 181.7 ± 36.1 mg/dL in the CG. Blood glucose values were in the target range 65% and 32% of the times, respectively for PG and CG groups (p < 0.001). The median time to reach glucose target range was 7 h (range 4 -10 h) for PG and 96 hr (range 46 - 278 h) for CG (p < 0.001). Incidence of severe hypoglycemia did not reach difference statistically significant: 4 patients in PG versus 2 patients in CG. CONCLUSIONS: Yale insulin infusion protocol was effective and safe to improve blood glucose control in a Brazilian medical and surgical intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):242-250
DOI 10.1590/S0103-507X2006000300005
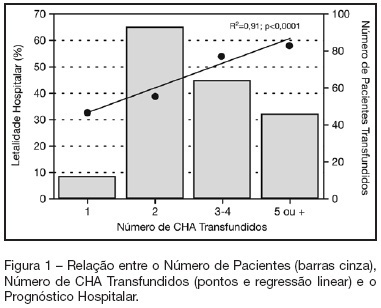
BACKGROUND AND OBJECTIVES: Packed red blood cell (PRBC) transfusion is frequent in intensive care unit (ICU). However, the consequences of anemia in ICU patients are poorly understood. Our aim was to evaluate the prevalence, indications, pre-transfusion hematocrit and hemoglobin levels, and outcomes of ICU patients transfused with PRBC. METHODS: Prospective cohort study conducted at a medical-surgical ICU of a teaching hospital during a 16-month period. Patients' demographic, clinical, laboratory and transfusion-related data were collected. Logistic regression was used after univariate analyses. RESULTS: A total of 698 patients were evaluated and 244 (35%) received PRBC, mainly within the first four days of ICU (82.4%). Transfusion was more frequent in medical and emergency surgical patients. The mean pre-transfusion hematocrit and hemoglobin were 22.8% ± 4.5% and 7.9 ± 1.4 g/dL, respectively. Transfused patients received 4.4 ± 3.7 PRBC during ICU stay and 2.2 ± 1 PRBC at each transfusion. The ICU (39.8% versus 13.2%; p < 0.0001) and hospital (48.8% versus 20.3%; p < 0.0001) mortality rates were higher in transfused patients. Mortality increased as the number of transfused PRBC increased (R² = 0.91). In logistic regression, predictive factors for PRBC transfusion were hepatic cirrhosis, mechanical ventilation (MV), type and duration of ICU admission, and hematocrit. The independent factors associated to hospital mortality were MV, transfusions of more than five PRBC and SAPS II score. CONCLUSIONS: PRBC transfusions are frequent in ICU patients, especially in those with medical and emergency surgical complications, longer ICU stay, and hepatic cirrhosis and in need of MV. Pre-transfusion hemoglobin levels were lower than those previously reported. In our study, PRBC transfusion was associated with increased mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):114-120
DOI 10.1590/S0103-507X2006000200002
BACKGROUND AND OBJECTIVES: Information on the outcomes of patients who were refused to the ICU is limited. The aims of this study were to compare the clinical characteristics of patients who were admitted with those of patients who were refused to the ICU and to identify clinical parameters associated with triage procedures. METHODS: Observational prospective cohort study. The following data were collected using a standard questionnaire: comorbidities, acute illness, vital status, laboratory data and APACHE II score. The end-points of interest were admission to the ICU and vital status at hospital discharge. RESULTS: A total of 455 patients were studied; 254 (56%) were admitted and 201 (44%) were not. The main reason for the refuse of admission was the lack of ICU beds (82%). Patients who were not admitted had a higher mortality (85% vs. 61%; p < 0.001). In multivariable analysis, the following variables were associated to non-admission [odds ratio, (95% confidence interval)]: metastatic cancer [5.6(1.7-18.7)], arterial systolic pressure < 90 mmHg [5.2(3.0-8.8)], age > 70 years [4.0(2.4-6.5)], hepatic cirrhosis [3.7(1.8-7.6)], and Glasgow coma scale < 5 [3.6(1.9-6.9)]. The variables associated with ICU admission were: mechanical ventilation [0.5(0.3-0.7)] and acute coronary syndromes [0.1(0.03-0.6)]. CONCLUSIONS: Refusal of ICU admission is frequent and generally as a consequence of ICU beds shortage. Patients who were not admitted had a higher mortality. Clinical characteristics associated with the refusal of admission were identified suggesting that they are used in clinical decision-making for ICU triage.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):82-87
DOI 10.1590/S0103-507X2008000100013
BACKGROUND AND OBJECTIVES: Until the end of the previous century it remained controversial to admit cancer patients to the ICU for advanced-life-supporting therapy. However, over the past few years several centres over the world have shown that it is possible to achieve a meaningful survival in these patients. The aim of this review is to focus on the improvement in outcome that has been achieved over the past two decades in critically ill cancer patients. CONTENTS: We performed a MEDLINE search (period of 1980 to November 2007) to identify full-text English language publications on critically ill patients with solid tumors or hematological malignancies with particular interest for the outcome and treatment. Major MESH search terms included; cancer, solid tumor, hematologic or hematological malignancies, immunosupression, ICU, ventilation, organ failure, sepsis and infection. Additional studies were identified through a manual search of citations from retrieved articles. CONCLUSIONS: In this review, we first focus on the grim prognosis in the past, subsequently we discuss the improvements in outcome over the past few years across subgroups of cancer patients with increasing degree of severity of illness, and finally, we focus on the value of non-invasive ventilation since it is considered the initial ventilatory strategy in these patients.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):31-36
DOI 10.1590/S0103-507X2008000100005
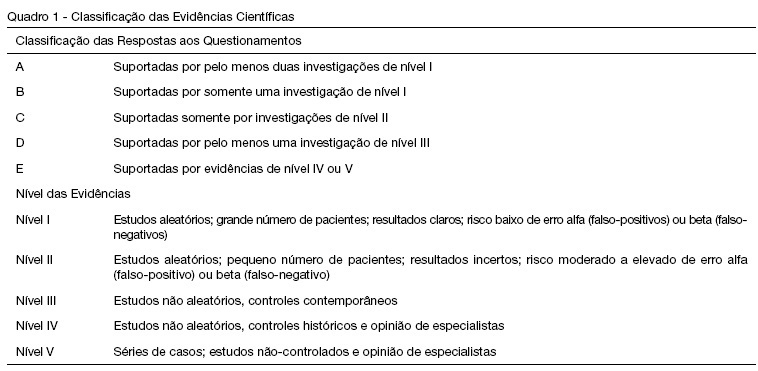
BACKGROUND AND OBJECTIVES: Peritoneal dialysis (PD) is frequently used to replace glomerular filtration and to control acid-base, electrolyte and fluid disturbances in critically ill children with acute renal failure. However, cardiorespiratory changes can happen during this procedure. The objective of this review is to describe the PD cardio-respiratory repercutions in the pediatric patient and the evidence level of the studies that approach these repercutions. METHODS: Bibliographic revision about PD cardio-respiratory repercutions in the pediatric patient. Medline, Ovid e Lilacs databases were searched for articles from 1990 to 2007 with the following key words in Portuguese, English and Spanish: diálise peritoneal, efeitos hemodinâmicos, complicações respiratórias, complicações cardíacas, Pediatria; peritoneal dialysis, hemodynamic effects, respiratory complications, cardiac complications, Pediatric; peritoneal diálisis, efecto hemodinámico, complicaciones respiratorias, complicaciones cardiacas, Pediatria. The retrieved articles were classified according to Cook et al. 1992. RESULTS: Thirteen articles were retrieved, 8 of them were about cardiorespiratory repercussions and five approached respiratory repercussions of PD. These studies evaluated 178 critically ill patients, from newborns to adolescents. Among the respiratory repercutions during PD the most frequent ones were decrease of the pulmonary compliance and arterial oxygen partial pressure and increase of airway resistance and carbon dioxide partial pressure; after the infusion of PD fluid the studies pointed out an increased arterial oxygen partial pressure/ inspired oxygen fraction relation and diminution of the alveolar-arterial difference and oxygenation index. Increase of the mean arterial pressure, pulmonary artery pressure, right and left atrial pressure and systemic vascular resistance and, reduction of the central venous pressure were the described cardio-circulatory repercutions during PD. CONCLUSIONS: Pulmonary volumes, gas exchange and cardio-circulatory alterations are the most frequent complications during and after PD in the pediatric patient. Therefore critically ill pediatric patients with acute renal failure needing PD should be monitored during and after this procedure to avoid clinical deterioration and to educate the multi-professional team.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):481-484
DOI 10.1590/S0103-507X2007000400013
BACKGROUND AND OBJECTIVES: Caring for the families is one of the major tasks of the global care of patients admitted to the intensive care unit (ICU). In the context of a terminally ill patient or a patient in whom the recovery from the acute illness is unlikely, dealing with and caring for their family members becomes even more important as the patient will not be awake in most of situations. Family members have specific needs and present with high incidence of symptoms of stress, depression, anxiety and related disorders during the ICU of their beloved one, which can even persist late after the patient's death. CONTENTS: Review of selected studies on the care of family members of patients at the end-of-life admitted to the ICU published at the PubMed database during the last 20 years. CONCLUSIONS: Recent literature is plenty of evidence that strategies directed to care of family members, such as improvement of the communication process, prevention of conflicts, and spiritual care, can improve satisfaction and perception of quality on the care of patients at the end-of-life in the ICU.
Abstract
Rev Bras Ter Intensiva. 2007;19(2):137-143
DOI 10.1590/S0103-507X2007000200001
BACKGROUND AND OBJECTIVES: There is a growing tendency of looking for "dying with dignity", rather than to prolong death and suffering of terminal patients on intensive care units (ICU). This study aims to evaluate medical practices that suggest therapeutic limitation (TL) in patients who died in an adult ICU. METHODS: A retrospective exploratory study was carried out to evaluate medical records of patients who died in a general adult ICU of a private hospital in Salvador-BA, between January and August of 2003, after at least 24 hours from the admission. The patients were classified, in relation to their deaths, in: "not responding to cardiopulmonary resuscitation", "brain death", "decision not to resuscitate" (DNR) and "withhold or withdrawal life-support measures". RESULTS: Sixty seven patients were included, corresponding to 90.4% of the deaths occurred in this ICU during the referred period. The most of them (56.7%) were women and the patients’ mean age was 66.58 ± 17.86 years. Suggestive measures of TL were found in 59.7% of the patients, being "withhold of life-support measures" the most important (35.8%), followed by DNR (17.9%) and "withdrawal of life-support measures" (6%). The procedures most commonly omitted were use of vasoactive drugs and dialysis, while antibiotics were the most discontinued. The use of TL measures was more frequent in clinical patients. CONCLUSIONS: The results of the present study suggest high frequencies of medical conducts suggestive of TL in a general ICU in Northeast of Brazil. Therapeutic methods that could cause discomfort or suffering to the patients, as nutrition, sedation and analgesia, were rarely omitted or discontinued.