Abstract
Rev Bras Ter Intensiva. 2006;18(3):242-250
DOI 10.1590/S0103-507X2006000300005
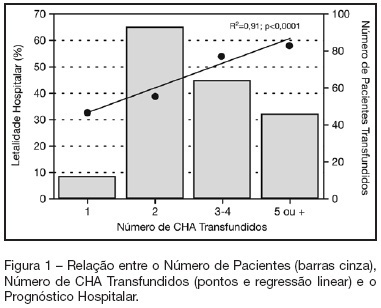
BACKGROUND AND OBJECTIVES: Packed red blood cell (PRBC) transfusion is frequent in intensive care unit (ICU). However, the consequences of anemia in ICU patients are poorly understood. Our aim was to evaluate the prevalence, indications, pre-transfusion hematocrit and hemoglobin levels, and outcomes of ICU patients transfused with PRBC. METHODS: Prospective cohort study conducted at a medical-surgical ICU of a teaching hospital during a 16-month period. Patients' demographic, clinical, laboratory and transfusion-related data were collected. Logistic regression was used after univariate analyses. RESULTS: A total of 698 patients were evaluated and 244 (35%) received PRBC, mainly within the first four days of ICU (82.4%). Transfusion was more frequent in medical and emergency surgical patients. The mean pre-transfusion hematocrit and hemoglobin were 22.8% ± 4.5% and 7.9 ± 1.4 g/dL, respectively. Transfused patients received 4.4 ± 3.7 PRBC during ICU stay and 2.2 ± 1 PRBC at each transfusion. The ICU (39.8% versus 13.2%; p < 0.0001) and hospital (48.8% versus 20.3%; p < 0.0001) mortality rates were higher in transfused patients. Mortality increased as the number of transfused PRBC increased (R² = 0.91). In logistic regression, predictive factors for PRBC transfusion were hepatic cirrhosis, mechanical ventilation (MV), type and duration of ICU admission, and hematocrit. The independent factors associated to hospital mortality were MV, transfusions of more than five PRBC and SAPS II score. CONCLUSIONS: PRBC transfusions are frequent in ICU patients, especially in those with medical and emergency surgical complications, longer ICU stay, and hepatic cirrhosis and in need of MV. Pre-transfusion hemoglobin levels were lower than those previously reported. In our study, PRBC transfusion was associated with increased mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):390-395
DOI 10.1590/S0103-507X2006000400012
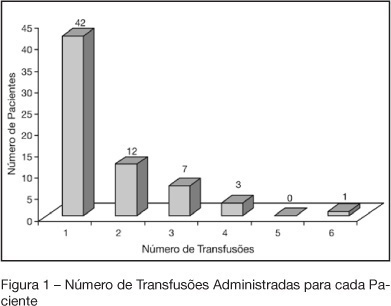
BACKGROUND AND OBJECTIVES: Indications of red blood cell transfusion in critically ill children are not very well determined. This study aims to describe red blood cells transfusion practice at the PICU of UNESP-Botucatu Medical School. METHODS: Retrospective observational study of all patients who received transfusion during 2003. RESULTS: Seventy five patients received transfusion and 105 indications were recorded. 53.3% of the patients were less than one year of age. Increased respiratory rate (75.2%), paleness (65.7%), and hypotension (51.4%) were the alterations more frequently recorded, before transfusion. Also, metabolic acidosis (68.08%) e and hipoxemia (63.8%) were very frequently observed. From 93 hemoglobin (Hb) values recorded, 54 (58.1%) varied from 7 to 10 g/dL and from 90 records of hematocrit (Ht) 66 (73.3%) varied from 21% to 30%. The main indications of the transfusion were anemia, in 75 children (71.4%), and active bleeding in 26 (24.7%). The mean value of Hb before transfusion was 7.82 ± 2.82 g/dL. Seven transfusions were indicated for patients with Hb levels higher than 10 g/dL (postoperative heart surgery and septic patients). CONCLUSIONS: red blood cells transfusion is carefully prescribed at the PICU by using restrictive indications (Hb between 7 and 10 g/dL). Not always is possible to find out records of the Hb levels immediately before transfusion. Hence, a protocol to better prescribe red blood cell transfusion at the PICU was adopted.