Abstract
Rev Bras Ter Intensiva. 2014;26(3):305-312
DOI 10.5935/0103-507X.20140043
The number of studies investigating circulating nucleic acids as potential biomarkers has increased in recent years. The detection of such biomarkers is a minimally invasive alternative for the diagnosis and prognosis of various clinical conditions. The value of circulating DNA levels as a predictive biomarker has been demonstrated in patients suffering from numerous acute pathologies that have a high risk of intensive care needs and in-hospital deaths. The mechanism by which circulating DNA levels increase in patients with these conditions remains unclear. In this review, we focused on the potential use of this biomarker for prognosis prediction in critically ill and trauma patients. The literature review was performed by searching MedLine using PubMed in the English language.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):155-161
DOI 10.5935/0103-507X.20130027
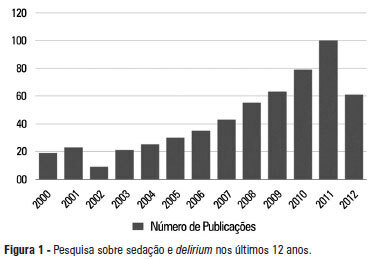
A significant number of landmark studies have been published in the last decade that increase the current knowledge on sedation for critically ill patients. Therefore, many practices that were considered standard of care are now outdated. Oversedation has been shown to be hazardous, and light sedation and no-sedation protocols are associated with better patient outcomes. Delirium is increasingly recognized as a major form of acute brain dysfunction that is associated with higher mortality, longer duration of mechanical ventilation and longer lengths of stay in the intensive care unit and hospital. Despite all the available evidence, translating research into bedside care is a daunting task. International surveys have shown that practices such as sedation interruption and titration are performed only in the minority of cases. Implementing best practices is a major challenge that must also be addressed in the new guidelines. In this review, we summarize the findings of sedation and delirium research over the last years. We also discuss the gap between evidence and clinical practice and highlight ways to implement best practices at the bedside.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):362-368
DOI 10.1590/S0103-507X2012000400012
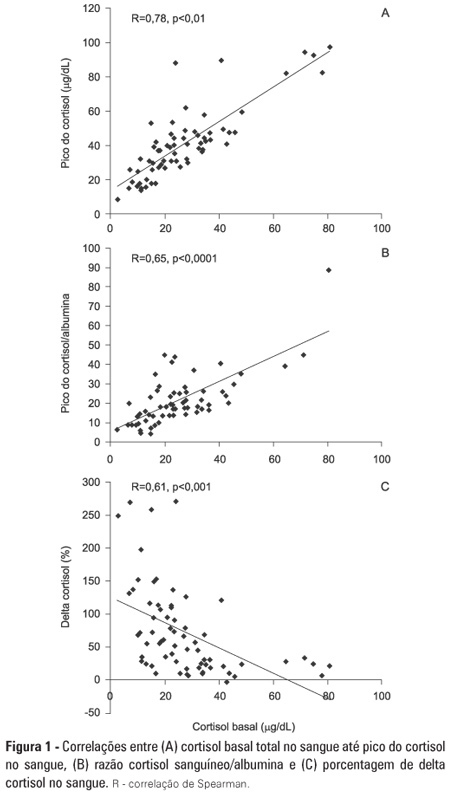
OBJECTIVE: To evaluate if cortisol responses to 250 µg of intravenously administered adrenocorticotropic hormone are related to disease severity and, hence, mortality. METHODS: This is a retrospective study in a medical-surgical intensive care unit of a university hospital. We studied 69 consecutive patients with septic shock over a 1-yr period; these patients underwent a short 250-µg adrenocorticotropic hormone test because they exhibited >6 hours of progressive hemodynamic instability requiring repeated fluid challenges and vasopressor treatment to maintain blood pressure. The test was performed by intravenously injecting 250 µg of synthetic adrenocorticotropic hormone and measuring cortisol immediately before injection, 30 minutes post-injection and 60 minutes post-injection. RESULTS: The mean APACHE II score was 22±7. The intensive care unit mortality rate at day 28 was 55%. Median baseline cortisol levels (19 [11-27] µg/dL versus 24 [18-34] µg/dL, p=0.047) and median baseline cortisol/albumin ratios (7.6 [4.6-12.3] versus 13.9 [8.8-18.5]; p=0.01) were lower in survivors than in non-survivors. Responders and non-responders had similar baseline clinical data and outcomes. The variables that were significantly correlated with outcome based on the area under the ROC curves (AUC) were APACHE II (AUC=0.67 [0.535 to 0.781]), baseline cortisol (µg/dl) (AUC=0.662 [0.536 to 0.773], peak cortisol (µg/dl) (AUC=0.642 [0.515 to 0.755]) and baseline cortisol/albumin (AUC=0.75 [0.621 to 0.849]). CONCLUSIONS: Increased basal cortisol is associated with mortality and disease severity. Cortisol responses upon adrenocorticotropic hormone stimulation were not related to outcome. The cortisol/albumin ratio does not predict unfavorable outcomes better than total cortisol levels or help to improve the accuracy of the adrenocorticotropic hormone test.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
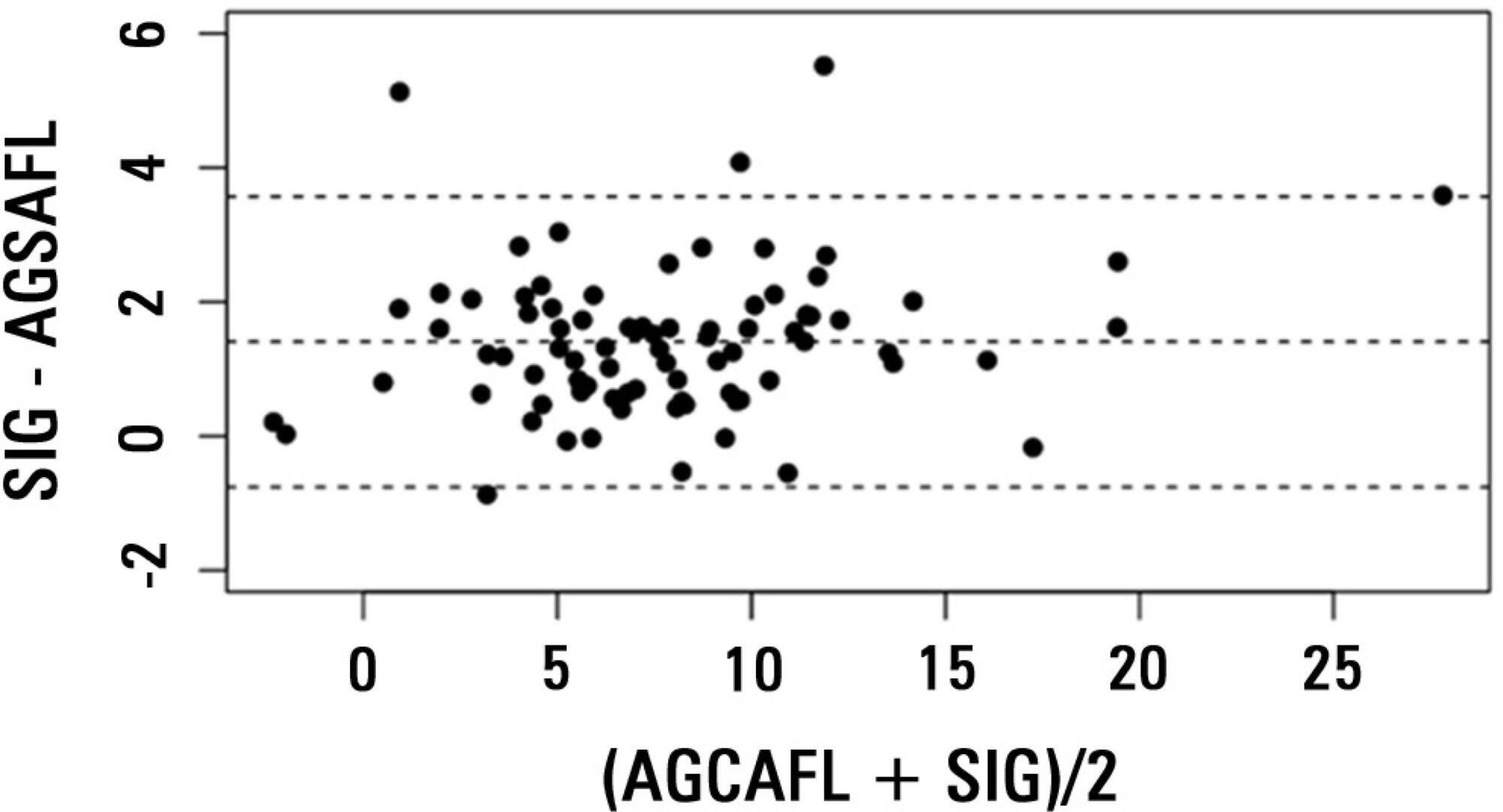
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group - hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):6-22
DOI 10.1590/S0103-507X2012000100003
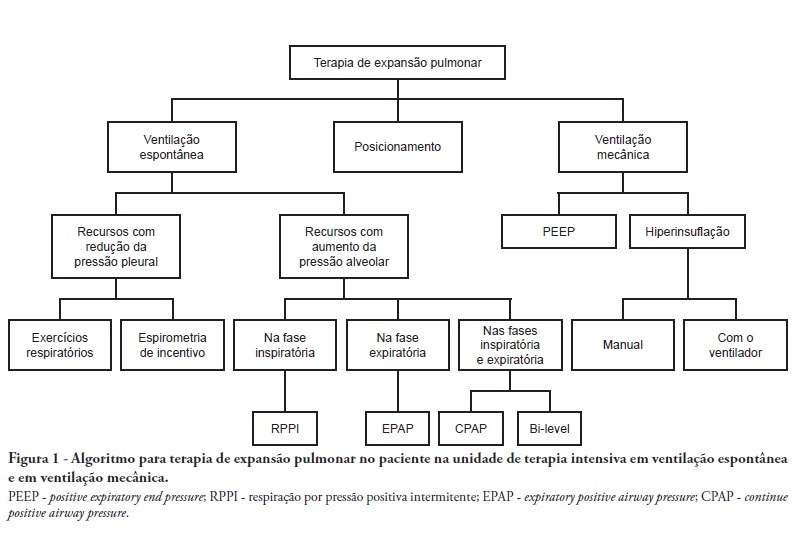
Complications from immobility in intensive care unit patients contribute to functional decline, increased healthcare costs, reduced quality of life and higher post-discharge mortality. Physical therapy focuses on promoting recovery and preserving function, and it may minimize the impact of these complications. A group of Brazilian Association of Intensive Care Medicine physical therapy experts developed this document that contains minimal physical therapy recommendations appropriate to the Brazilian real-world clinical situation. Prevention and treatment of atelectasis, procedures related to the removal of secretions and treatment of conditions related to physical deconditioning and functional decline are discussed. Equally important is the consideration that prescribing and executing activities, mobilizations and exercises are roles of the physical therapist, whose diagnosis should precede any intervention.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):448-454
DOI 10.1590/S0103-507X2011000400009
OBJECTIVES: This study aimed to assess family member acceptance of orthotanasia as related to symptom management, patient preference and the influence of the medical team's communication on therapy. METHODS: This was a descriptive one-year study conducted at the adult intensive care unit of the Hospital do Servidor Público Estadual. A structured questionnaire based on the Quality of Dying and Death (QODD 22) instrument and prior informal interviews were used. RESULTS: Sixty family members were assessed; the mean age was 51.7 + 12.1 years, and 81.7% were female. The patients were hospitalized for a mean of 31 + 26.9 days, and 17.0% of these days were spent in the intensive care unit. Most of the patients had neurological conditions. Most of the patients (53.3%) had discussed their end-of-life care wishes with family members; however, 76.7% of them had not discussed this issue with their doctors (p < 0.00). The family members reported being favorable to orthotanasia in 83.3% of the cases. Most (85.0%) desired the medical team to clearly approach the subject, and 65.0% wished to take part in the quality of end-of-life decision making process. The family members were generally satisfied with information they received from the doctors: 93.3% believed they had received appropriately frequent communications about the clinical conditions; 81.7% were able to clarify their doubts regarding the patient's clinical status; the communication was understood by 83.3% of the respondents; and 80.0% believed that clear and honest information had been provided. Only 43.3% of the respondents wished to be present at the time of their loved ones' deaths. A significant association between family member acceptance of orthotanasia and participation in end-of-life decisions (p = 0.042) was observed. CONCLUSIONS: Most of the respondents were favorable to orthotanasia and wished to participate in end-of-life discussions.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):217-221
DOI 10.1590/S0103-507X2011000200015
In recent years, international health quality assurance organizations have been recommending ultrasound guidance for central venous punctures. This article reviews the evidence behind these recommendations. The MEDLINE, PubMed and SCIELO databases were searched for the following MeSH terms: central venous access, ultrasonography, and adults. The search was conducted on September 24, 2010, and selected meta-analyses, randomized clinical trials and reviews, retrieving 291 papers. The 21 most important papers were analyzed in this review. The internal jugular vein is the most studied ultrasound-guided puncture site, with meta-analysis showing lower relative risks of failure and complications. In addition, the largest available randomized clinical trial demonstrated a reduced central venous catheter-associated blood stream infection rate. There are few studies involving subclavian vein puncture; however, ultrasound was shown to be beneficial in two meta-analyses (however, with small numbers of patients). Regarding the femoral venous site, only one randomized clinical trial (20 patients) was identified, showing positive findings. In a British cost-effectiveness study, ultrasound use lead to resource savings for different sites of venous puncture. There is strong evidence for ultrasound benefit for internal jugular vein puncture. Although the method appears attractive for the other sites, the data are not sufficient to support any recommendation.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):24-29
DOI 10.1590/S0103-507X2011000100005
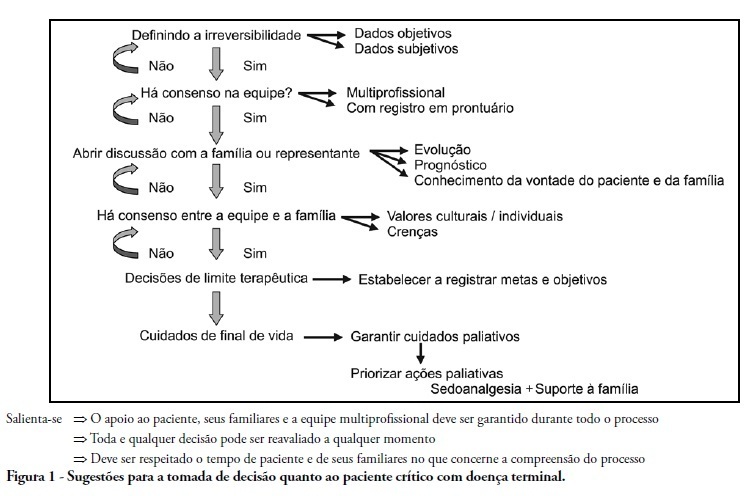
Palliative care is aimed to improve the quality of life of both patients and their family members during the course of life-threatening diseases through the prevention, early identification and treatment of the symptoms of physical, psychological, spiritual and social suffering. Palliative care should be provided to every critically ill patient; this requirement renders the training of intensive care practitioners and education initiatives fundamental. Continuing the Technical Council on End of Life and Palliative Care of the Brazilian Association of Intensive Medicine activities and considering previously established concepts, the II Forum of the End of Life Study Group of the Southern Cone of America was conducted in October 2010. The forum aimed to develop palliative care recommendations for critically ill patients.