Abstract
Rev Bras Ter Intensiva. 2013;25(3):181-183
DOI 10.5935/0103-507X.20130031
Abstract
Rev Bras Ter Intensiva. 2013;25(3):184-185
DOI 10.5935/0103-507X.20130032
Abstract
Rev Bras Ter Intensiva. 2013;25(3):186-187
DOI 10.5935/0103-507X.20130033
Abstract
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
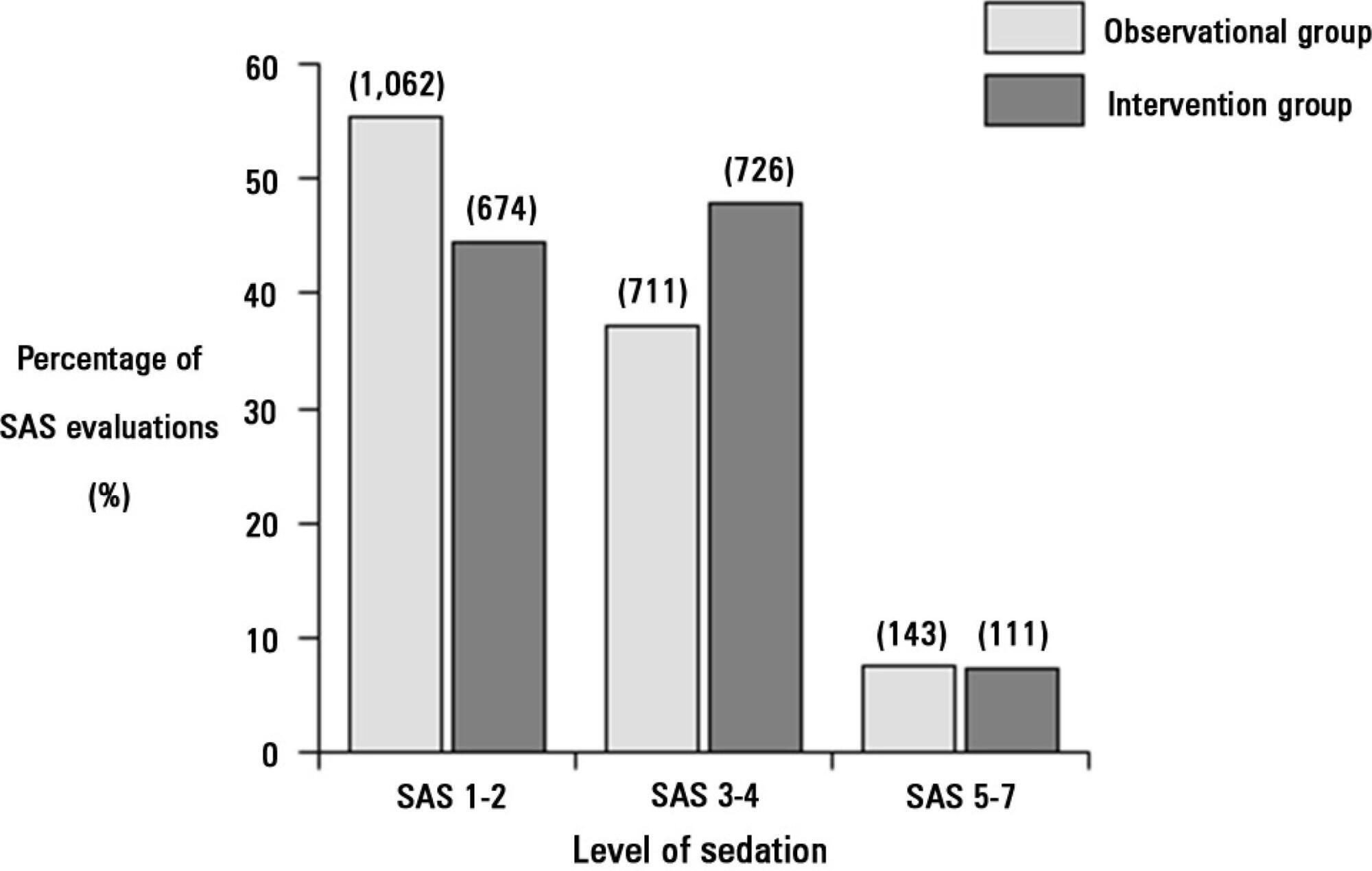
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
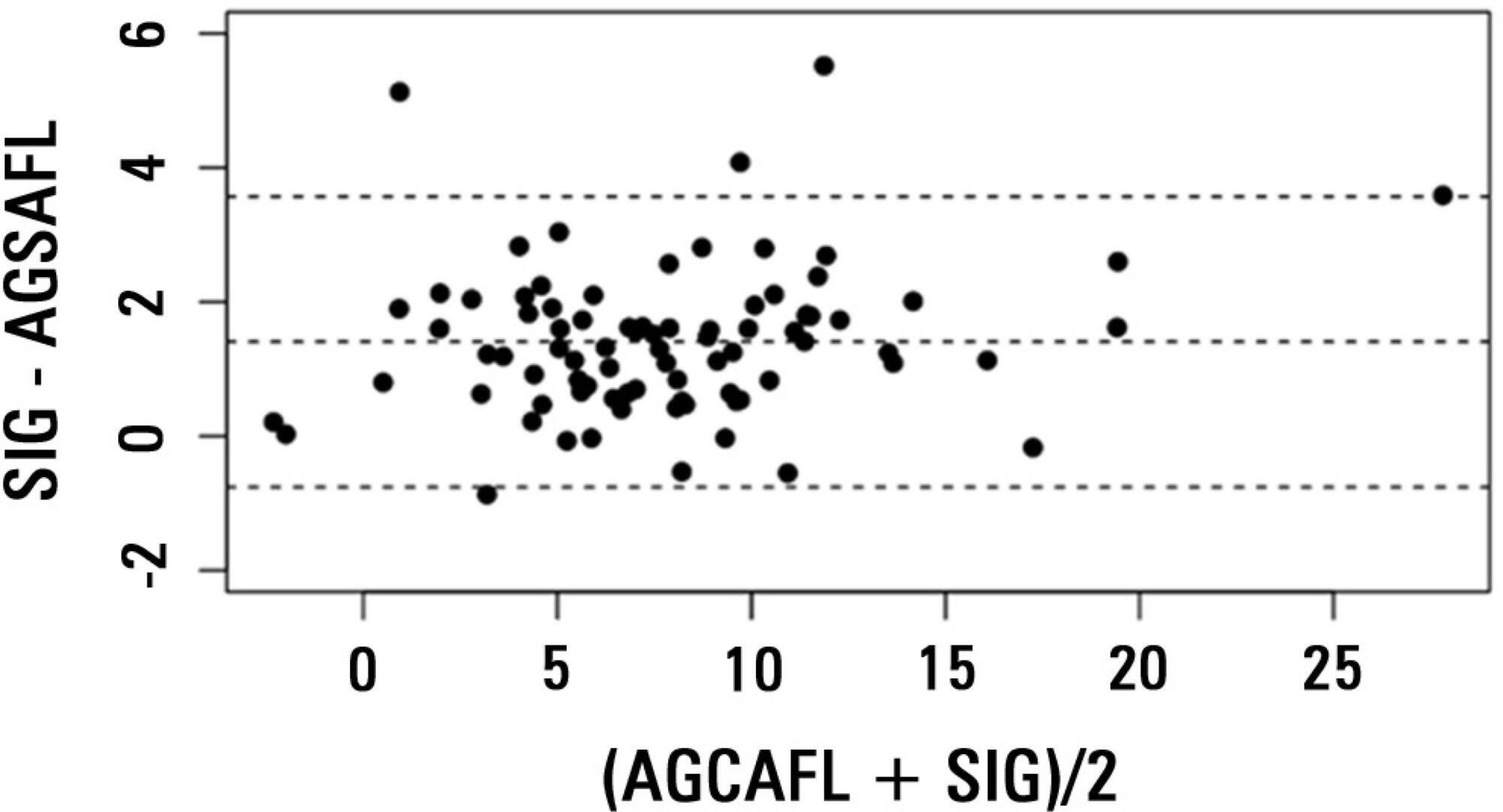
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group - hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
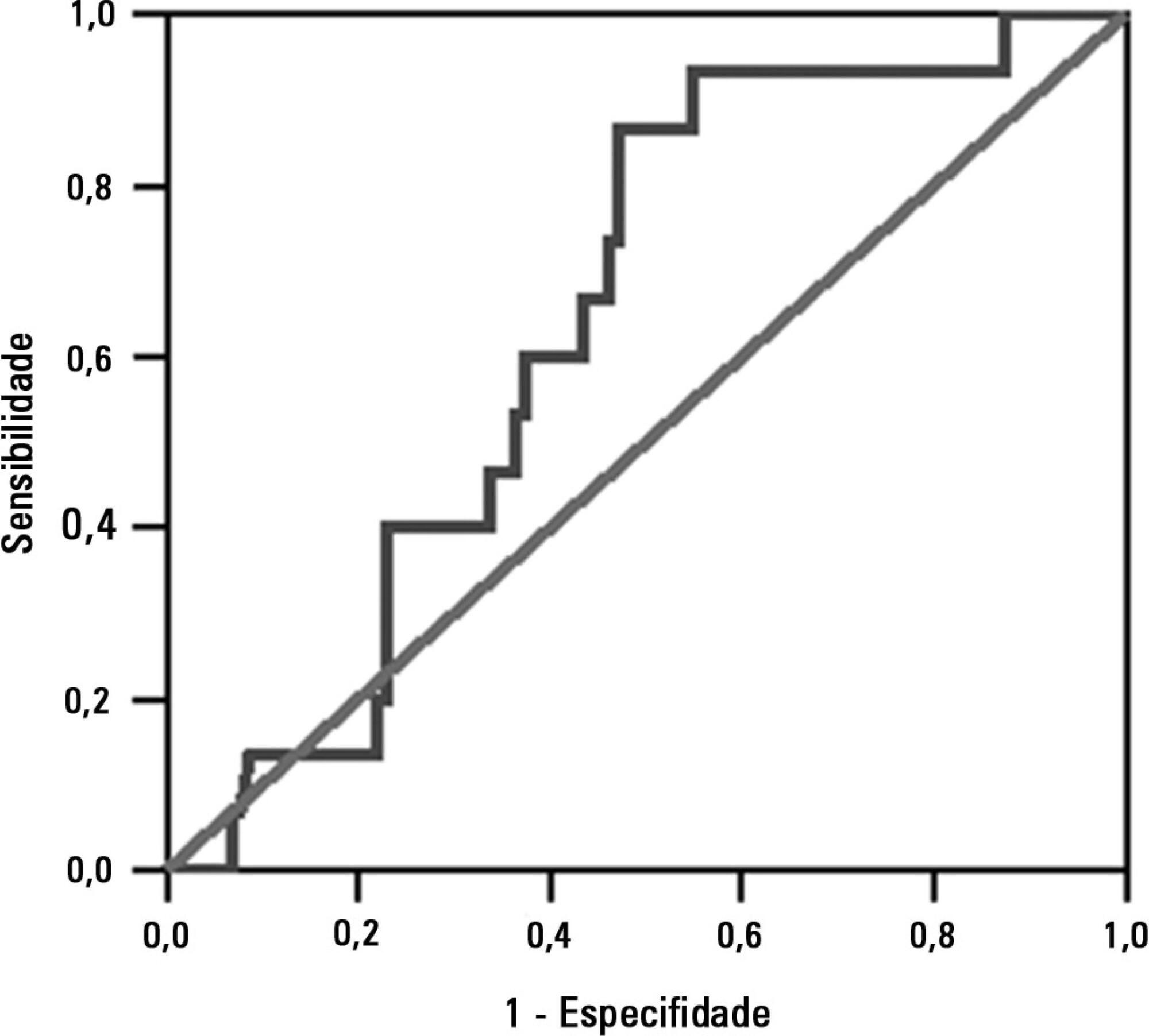
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):218-224
DOI 10.5935/0103-507X.20130038
To assess the functional and psychological features of patients immediately after discharge from the intensive care unit.
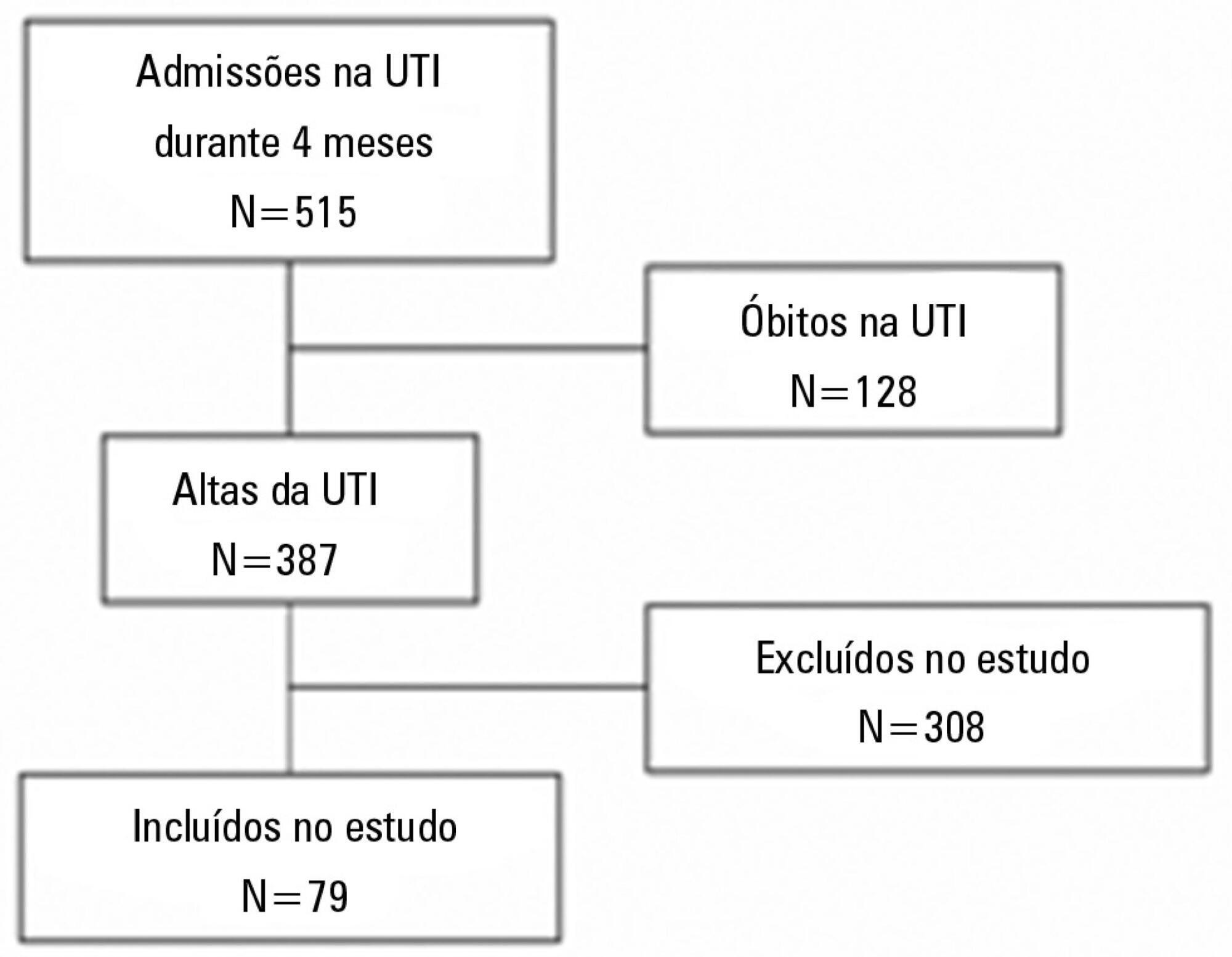
Prospective cohort study. Questionnaires and scales assessing the degree of dependence and functional capacity (modified Barthel and Karnofsky scales) and psychological problems (Hospital Anxiety and Depression Scale), in addition to the Epworth Sleepiness Scale, were administered during interviews conducted over the first week after intensive care unit discharge, to all survivors who had been admitted to this service from August to November 2012 and had remained longer than 72 hours.
The degree of dependence as measured by the modified Barthel scale increased after intensive care unit discharge compared with the data before admission (57±30 versus 47±36; p<0.001) in all 79 participants. This impairment was homogeneous among all the categories in the modified Barthel scale (p<0.001) in the 64 participants who were independent or partially dependent (Karnofsky score ≥40) before admission. The impairment affected the categories of personal hygiene (p=0.01) and stair climbing (p=0.04) only in the 15 participants who were highly dependent (Karnofsky score <40) before admission. Assessment of the psychological changes identified mood disorders (anxiety and/or depression) in 31% of the sample, whereas sleep disorders occurred in 43.3%.
Patients who remained in an intensive care unit for 72 hours or longer exhibited a reduced functional capacity and an increased degree of dependence during the first week after intensive care unit discharge. In addition, the incidence of depressive symptoms, anxiety, and sleep disorders was high among that population.