Abstract
Rev Bras Ter Intensiva. 2022;34(2):272-278
DOI 10.5935/0103-507X.20220025-en
To translate, crossculturally adapt and evaluate the clinimetric properties of the Critical Care Functional Rehabilitation Outcome Measure for evaluating the functionality of patients admitted to intensive care units in Brazil.
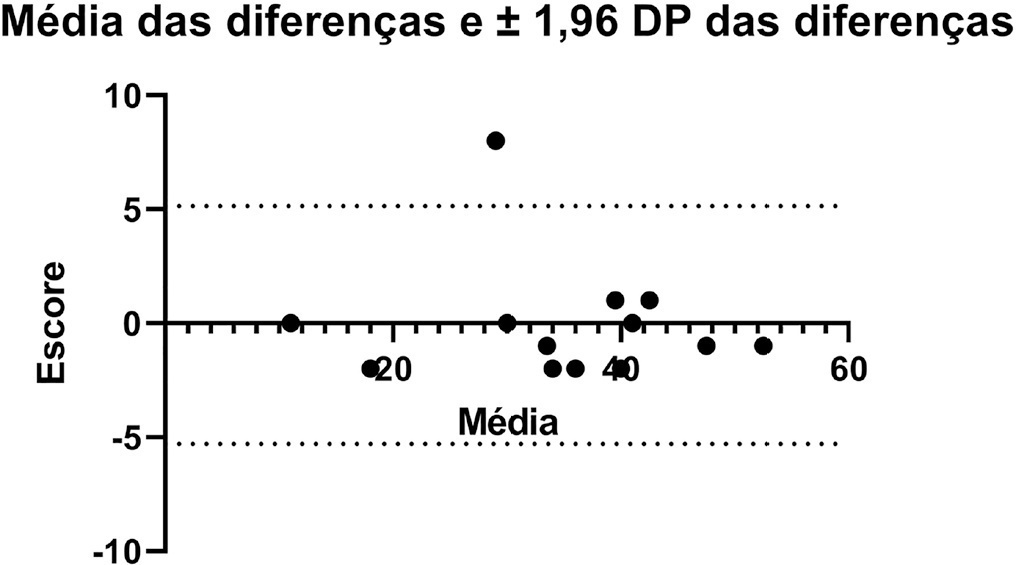
The process of translation and cross-cultural adaptation involved the following steps: initial translation, synthesis, back-translation, expert committee review and pretesting. The intra- and interrater reliability and agreement were analyzed between two physical therapists who evaluated the same group of patients (n = 35). The evaluations were performed by each therapist independently and blinded to the score assigned by the other professional. The qualitative analysis was performed by the review committee, and the experts adapted and synthesized the Portuguese translation of the Critical Care Functional Rehabilitation Outcome Measure.
There was agreement between the initial Brazilian translations of the Critical Care Functional Rehabilitation Outcome Measure scale. The conceptual, idiomatic, semantic and experimental equivalences between the original and translated versions were assessed, resulting in the final Brazilian version of the scale, called the Medida de Resultado da Reabilitação Funcional em Cuidados Intensivos. The evaluation of the clinimetric properties showed evidence of a high degree of agreement and reliability, as all had an intraclass correlation coefficient above 0.75. The overall intraclass correlation coefficient was 0.89.
The translated version of the Critical Care Functional Rehabilitation Outcome Measure scale for assessing the functionality of patients admitted to an intensive care unit can be used reliably in Brazil following translation and cross-cultural adaptation to Brazilian Portuguese and presents evidence of excellent interrater reliability.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):243-250
DOI 10.5935/0103-507X.20210031
To relate functional independence to the degree of pulmonary impairment in adult patients 3 months after discharge from the intensive care unit.
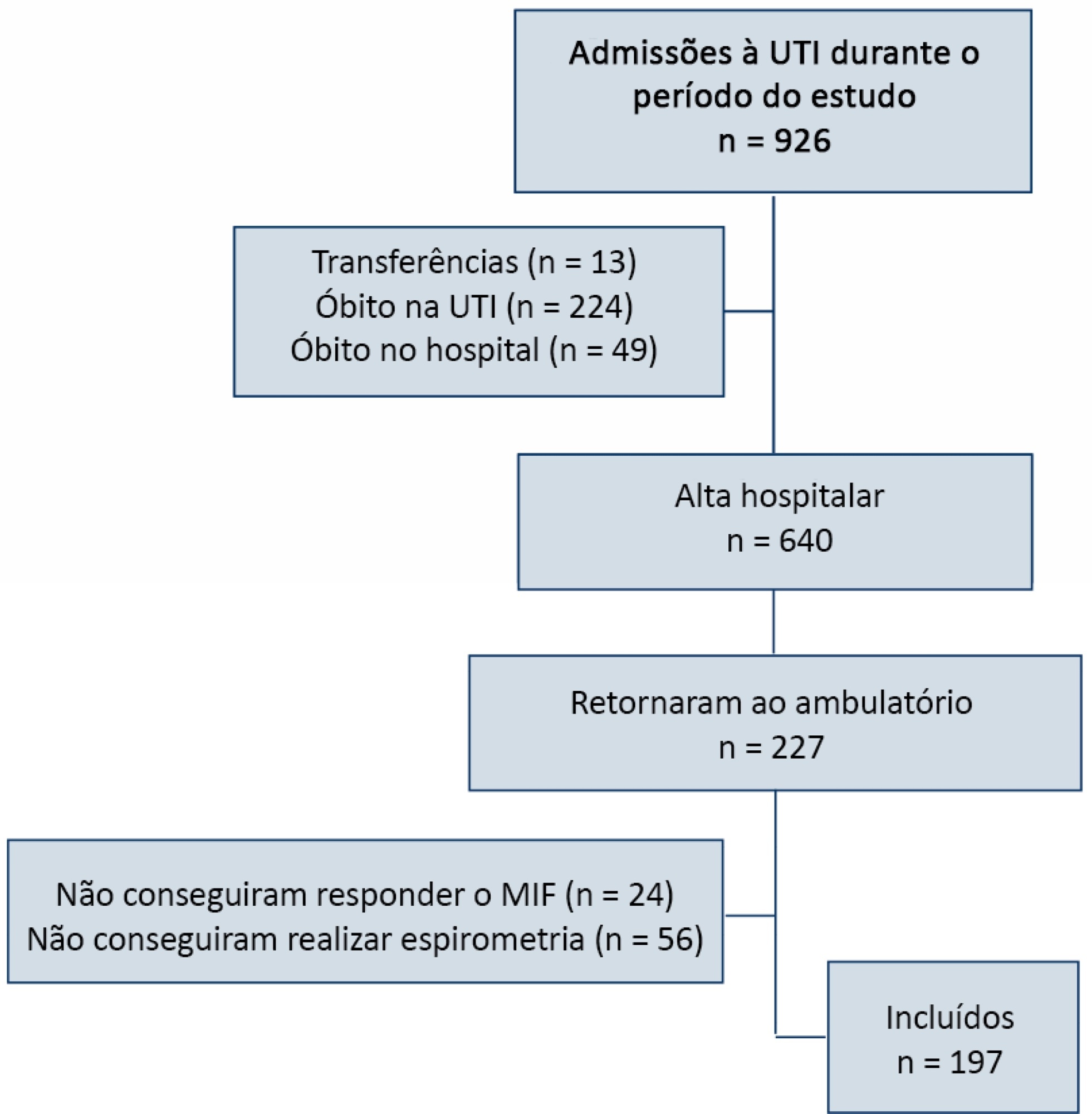
This was a retrospective cohort study conducted in one adult intensive care unit and a multi-professional post-intensive care unit outpatient clinic of a single center. Patients admitted to the intensive care unit from January 2012 to December 2013 who underwent (3 months later) spirometry and answered the Functional Independence Measure Questionnaire were included.
Patients were divided into groups according to the classification of functional independence and spirometry. The study included 197 patients who were divided into greater dependence (n = 4), lower dependence (n = 12) and independent (n = 181) groups. Comparing the three groups, regarding the classification of the Functional Independence Measure, patients with greater dependence had higher Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment values at intensive care unit admission with more advanced age, more days on mechanical ventilation, and longer stay in the intensive care unit and hospital. The majority of patients presented with pulmonary impairment, which was the obstructive pattern observed most frequently. When comparing functional independence with pulmonary function, it was observed that the lower the functional status, the worse the pulmonary function, with a significant difference being observed in peak expiratory flow (p = 0.030).
The majority of patients who returned to the outpatient clinic 3 months after discharge had good functional status but did present with pulmonary impairment, which is related to the degree of functional dependence.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):57-62
DOI 10.5935/0103-507X.20190016
To assess the Perme mobility scale score as a predictor of functional status and complications in the postoperative period in patients undergoing liver transplantation.
The sample consisted of 30 patients who underwent liver transplantation. The patients were evaluated at two time points to determine their perception of pain, degree of dyspnea, peripheral muscle strength, and functional status according to the Perme scale. The collected data were analyzed by descriptive and inferential statistics. To compare the means between the evaluations, Student's t test for paired samples was applied. In case of asymmetry, the Wilcoxon test was used. In the evaluation of the association between the quantitative variables, the Pearson or Spearman correlation tests were applied.
A total of 30 individuals who underwent liver transplantation were included. The patients were predominantly male, and the mean age was 58.4 ± 9.9 years. The most prevalent underlying pathology was cirrhosis C virus (23.3%). Significant associations of the time on mechanical ventilation with the Perme scale score at discharge from the intensive care unit (r = -0.374; p = 0.042) and the number of physical therapy treatments (r = -0.578; p = 0.001) were recorded. When comparing the results of the initial evaluation and the evaluation at hospital discharge, there was a significant improvement in functional status (p < 0.001).
Functional mobility, peripheral muscle strength, pain perception, and dyspnea are significantly improved at hospital discharge compared with those at inpatient unit admission.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):114-119
DOI 10.5935/0103-507X.20160025
To evaluate the variation in mobility during hospitalization in an intensive care unit and its association with hospital mortality.
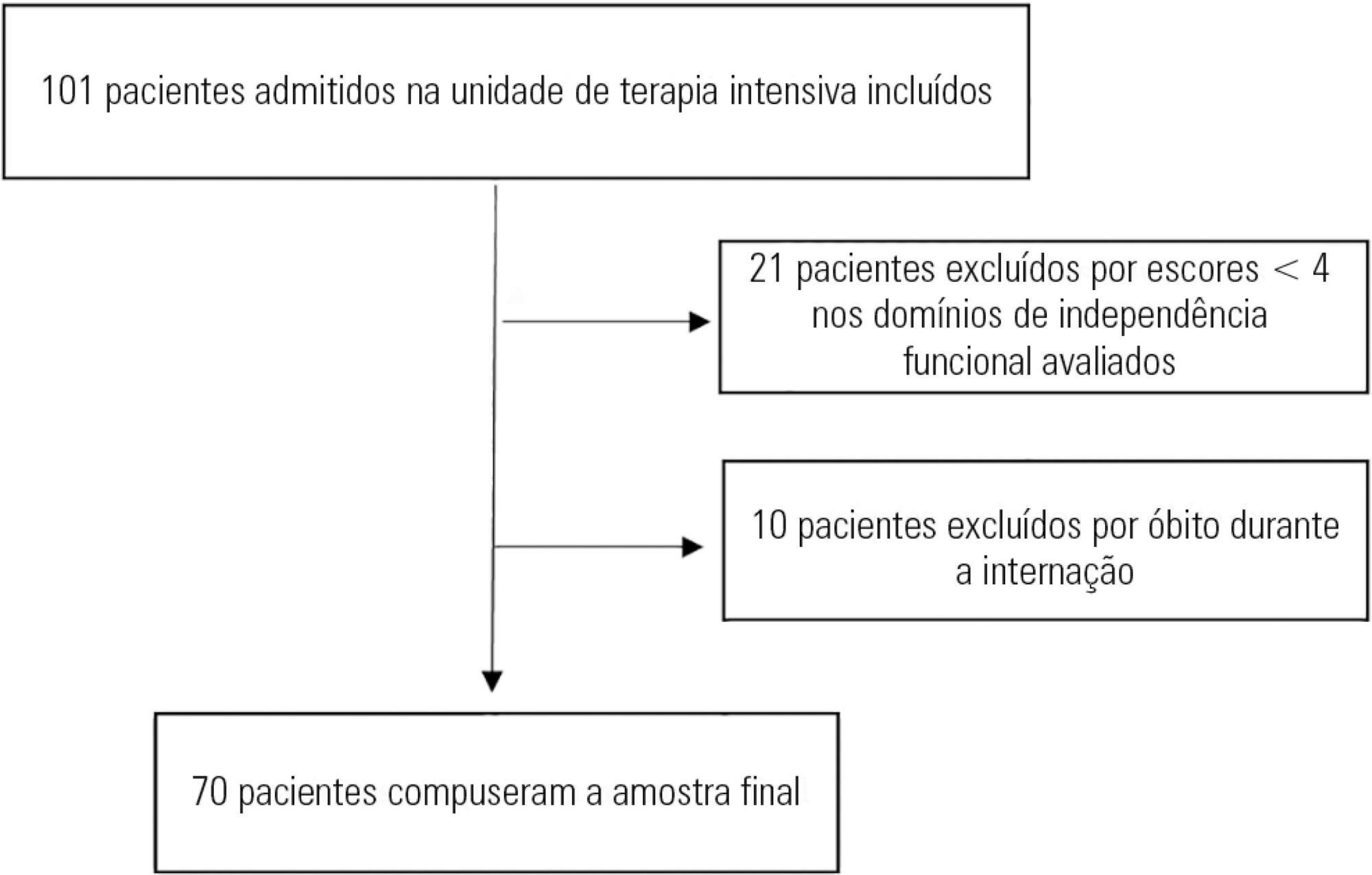
This prospective study was conducted in an intensive care unit. The inclusion criteria included patients admitted with an independence score of ≥ 4 for both bed-chair transfer and locomotion, with the score based on the Functional Independence Measure. Patients with cardiac arrest and/or those who died during hospitalization were excluded. To measure the loss of mobility, the value obtained at discharge was calculated and subtracted from the value obtained on admission, which was then divided by the admission score and recorded as a percentage.
The comparison of these two variables indicated that the loss of mobility during hospitalization was 14.3% (p < 0.001). Loss of mobility was greater in patients hospitalized for more than 48 hours in the intensive care unit (p < 0.02) and in patients who used vasopressor drugs (p = 0.041). However, the comparison between subjects aged 60 years or older and those younger than 60 years indicated no significant differences in the loss of mobility (p = 0.332), reason for hospitalization (p = 0.265), SAPS 3 score (p = 0.224), use of mechanical ventilation (p = 0.117), or hospital mortality (p = 0.063).
There was loss of mobility during hospitalization in the intensive care unit. This loss was greater in patients who were hospitalized for more than 48 hours and in those who used vasopressors; however, the causal and prognostic factors associated with this decline need to be elucidated.