Abstract
Rev Bras Ter Intensiva. 2021;33(3):469-476
DOI 10.5935/0103-507X.20210066
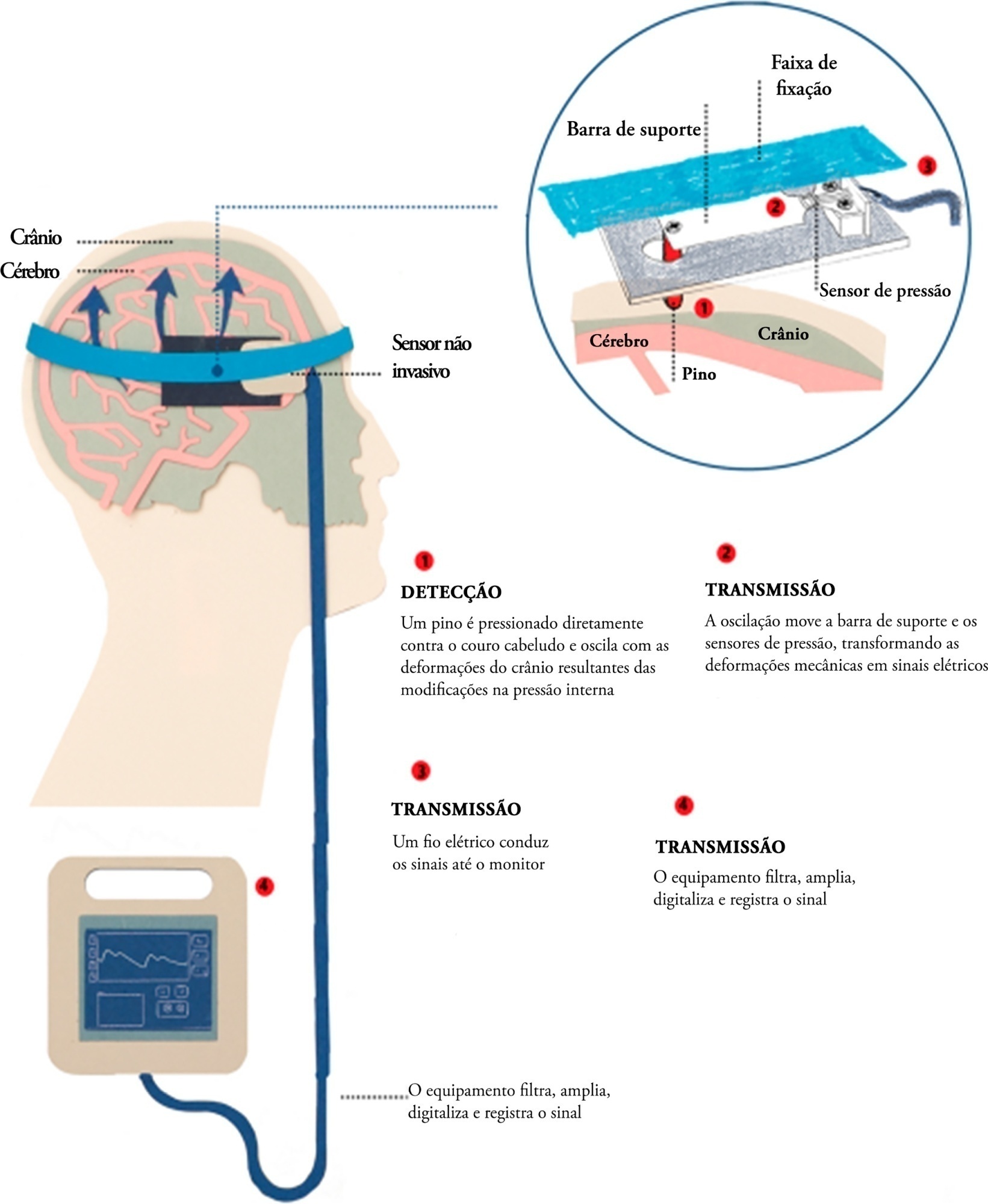
Brain injury caused by extracorporeal circulation during cardiovascular surgical procedures has been a recurring complication since the implementation of extracorporeal circulation five decades ago. There is no unique cause of brain injury due to the use of extracorporeal circulation, but it is known that brain injury affects about 70% of patients who undergo this procedure. Intracranial pressure assessment is one method that can guide the management of patients undergoing procedures associated with neurological disturbances. This study describes two cases of patients who underwent cardiovascular surgery with extracorporeal circulation in whom clinical protocols for neuroprotection in the postoperative phase were guided by intracranial pressure waveform findings obtained with a novel noninvasive intracranial pressure monitoring method.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):412-415
DOI 10.5935/0103-507X.20150069
We report the case of a 2-year-old child who survived an acute episode of severe spontaneous intracranial hemorrhage with clinical and radiological signs of intracranial hypertension and transtentorial herniation. The patient underwent emergency surgery to drain the hematoma, and a catheter was inserted to monitor intracranial pressure. In the initial computed tomography analysis performed prior to hematoma drainage, a brain cyst was evident contralateral to the hematoma, which, based on the analysis by the care team, possibly helped to avoid a worse outcome because the cyst accommodated the brain after the massive hemorrhage. After the investigation, the patient was determined to have previously undiagnosed hemophilia A. The patient underwent treatment in intensive care, which included the control of intracranial pressure, factor VIII replacement and discharge without signs of neurological impairment.

Abstract
Rev Bras Ter Intensiva. 2013;25(4):327-333
DOI 10.5935/0103-507X.20130055
To analyze the outcomes of increased or decreased intracranial pressure and/or the decrease in cerebral perfusion pressure resulting from respiratory physiotherapy on critically ill patients admitted to the intensive care unit.
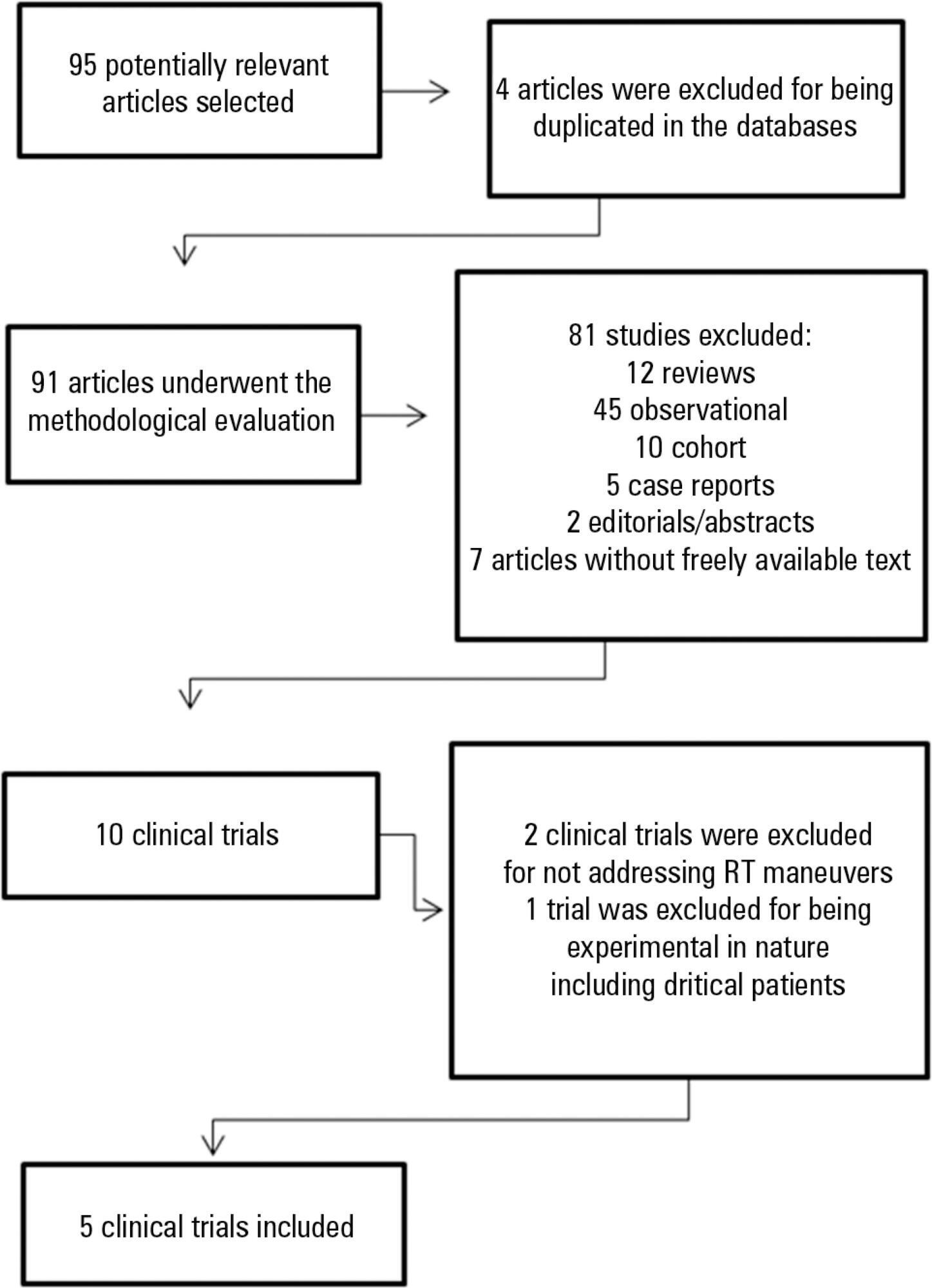
Through a systematic review of the literature, clinical trials published between 2002 and 2012 were selected. The search involved the LILACS, SciELO, MedLine and PEDro databases using the keywords "physical therapy", "physiotherapy", "respiratory therapy" and "randomized controlled trials" combined with the keyword "intracranial pressure".
In total, five studies, including a total of 164 patients between 25 and 65 years of age, reporting that respiratory physiotherapy maneuvers significantly increased intracranial pressure without changing the cerebral perfusion pressure were included. The articles addressed several techniques including vibration, vibrocompression, tapping, postural drainage, and the endotracheal aspiration maneuver. All patients required invasive mechanical ventilation.
Respiratory physiotherapy leads to increased intracranial pressure. Studies suggest that there are no short-term hemodynamic or respiratory repercussions or changes in the cerebral perfusion pressure. However, none of the studies evaluated the clinical outcomes or ensured the safety of the maneuvers.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):291-296
DOI 10.1590/S0103-507X2011000300006
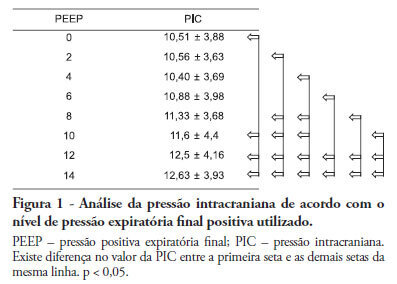
Positive intrathoracic pressure may cause hemodynamic changes, which can be transmitted to the cranial compartment, changing intracranial pressure and cerebral perfusion pressure. This can be increased when high positive end-expiratory pressure values are used. OBJECTIVE: To measure the impact of different positive end-expiratory pressure levels on intracranial pressure, cerebral perfusion pressure and mean blood pressure. METHOD: This study was conducted in a neurological intensive care unit and included 25 adult hemorrhagic stroke patients who were mechanically ventilated on airway pressure control mode. Patients were subjected to various positive end-expiratory values ranging between 0 and 14 cmH2O. The order of these values were randomized, and the variables were assessed five minutes after each new positive end-expiratory pressure level was initiated. RESULTS: Incremental positive end-expiratory pressures led to increased intracranial pressure (p < 0.001), however, no statistically significant changes were observed in mean blood pressure or cerebral perfusion pressure. CONCLUSION: In this population of patients with hemorrhagic stroke, positive end-expiratory pressure values up to 14 cmH2O did not alter cerebral perfusion pressure or mean blood pressure. Increased intracranial pressures were noted, although these elevations were not clinically significant
Abstract
Rev Bras Ter Intensiva. 2011;23(2):164-169
DOI 10.1590/S0103-507X2011000200008
OBJECTIVE: To evaluate the effects of hemodynamic, respiratory and metabolic changes on intracranial pressure in a model of acute lung injury and abdominal compartment syndrome. METHODS: Eight Agroceres pigs were submitted to five different clinical scenarios after instrumentation: 1) a baseline condition with low intra-abdominal pressure and healthy lungs; 2) pneumoperitoneum with 20 mmHg intra-abdominal pressure; 3) acute lung injury induced by pulmonary lavage with surfactant deactivation; 4) pneumoperitoneum with 20 mmHg intra-abdominal pressure with lung pulmonary injury and low positive end-expiratory pressure; and 5) 27 cmH2O positive end-expiratory pressure with pneumoperitoneum and acute lung injury. Respiratory and hemodynamic variables were collected. A multivariate analysis was conducted to search for variables associated with increased intracranial pressure in the five scenarios. RESULTS: Only plateau airway pressure showed a positive correlation with intracranial pressure in the multivariate analysis. In the models with acute lung injury, plateau airway pressure, CO2 arterial pressure, end tidal CO2 and central venous pressure were positively correlated with increased intracranial pressure. CONCLUSION: In a model of multiple organ dysfunction with associated clinical conditions causing increased intra-thoracic and abdominal pressure, increased intracranial pressure triggered by elevated intra-abdominal pressure is apparently caused by worsened respiratory system compliance and a reduced brain venous drainage gradient due to increased central venous pressure.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):72-79
DOI 10.1590/S0103-507X2009000100011
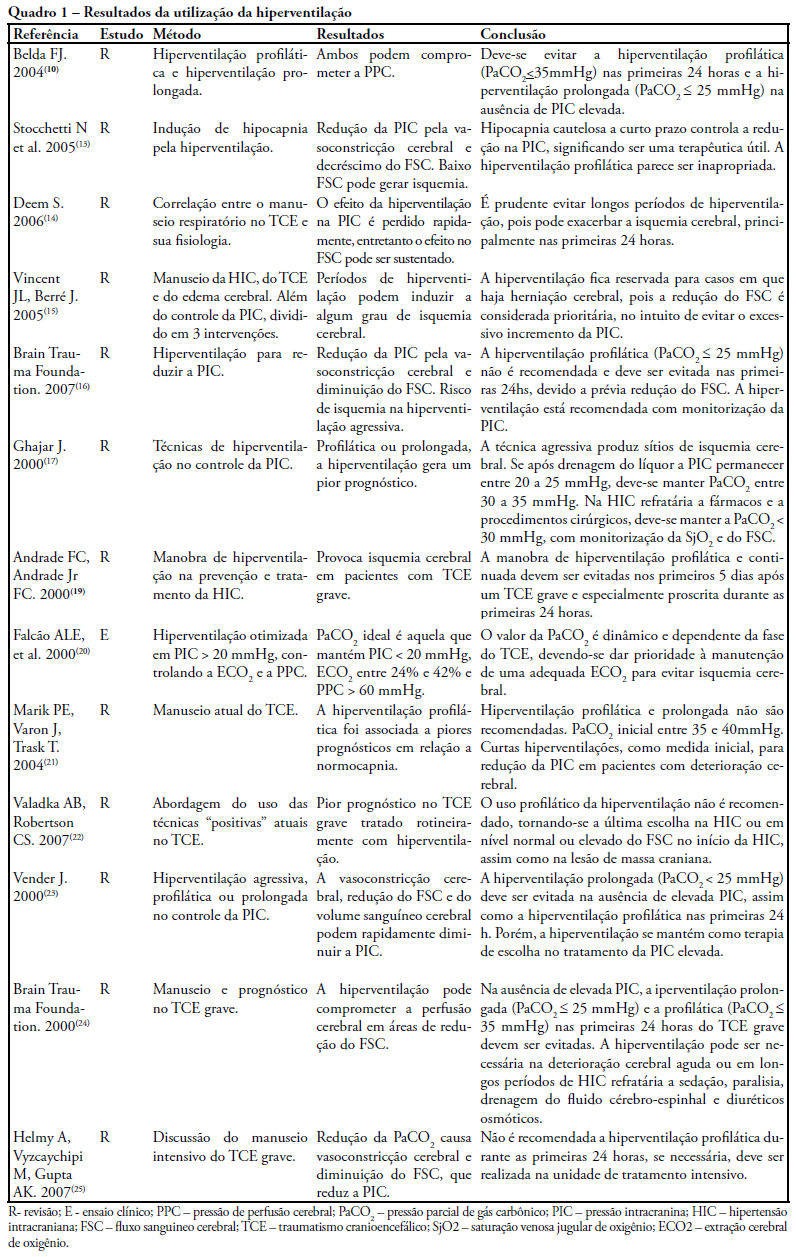
The study intended to make a critical review on use of pulmonary hyperventilation maneuvers and the different positive end-expiratory pressures applied to traumatic brain injury patients. As a reference were used publications in English, Spanish and Portuguese, contained in the following databases: MedLine, SciELO and LILACS, from 2000 to 2007, we included all studies about the use of pulmonary hyperventilation maneuvers and the different positive end-expiratory levels used for adult patients with brain injury at acute or chronic stage. Thirty one trials were selected, 13 about pulmonary hyperventilation, as prophylaxis, prolonged or optimized and 9 shows the levels of positive end-expiratory pressures used, ranging from 0 to 15 cmH2O. The prophylactic hyperventilation maneuver in the first 24 hours can lead to an increase of cerebral ischemia; the prolonged hyperventilation must be avoided if intracranial pressure did not increase; however optimized hyperventilation seems to be the most promising technique for control of the intracranial pressure and cerebral perfusion pressure; the rise of the positive end-expiratory pressure, up to 15cmH2O, can be applied in a conscientious form aiming to increase arterial oxygen saturation in lung injury.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):339-343
DOI 10.1590/S0103-507X2008000400004
OBJECTIVE: After brain injury intracranial hypertension is the major cause of mortality, in addition to the possibility of functional, behavioral and cognitive sequels. Scarcity of studies on the effects of respiratory physiotherapy on these patients may lead to contradictory performances. This study aimed to assess the effects of customary respiratory physiotherapy maneuvers on intracranial and cerebral perfusion pressures in patients with severe brain injury. METHODS: Clinical, prospective trial with patients with severe traumatic brain injury, mechanically ventilated and with a continued measurement of intracranial pressure. The effects of manual vibrocompression maneuvers and intratracheal aspiration with or without saline infusion on the measurements of intracranial and cerebral perfusion pressures, between the first and third day after cerebral injury were evaluated. RESULTS: Data were collected from 11 patients, 41 years of age (median) and APACHE II of 19.5 ± 5. The manual vibrocompression maneuver did not cause an increase of intracranial pressure on any of the days assessed. Intracranial pressure significantly increased after intratracheal aspiration maneuvers in relation to the basal measurement (day1, 9.5 ± 0.9 mm Hg vs 18.0 ± 3.2 mm Hg; day 2, 10.6 ± 1.7 mm Hg vs 21.4 ± 3.8 mm Hg; day 3, 14.4 ± 1.0 vs 24.9 ± 2.7 mm Hg; p<0.05 for all). However, these elevations were transient (about 27 seconds) and accompanied by compensatory increases of the cerebral perfusion pressure. CONCLUSION: The manual vibrocompression maneuver did not increase intracranial pressure or cerebral perfusion pressure in patients with severe brain injury. Intratracheal aspiration induced a significant and transient increase of the intracranial and cerebral perfusion pressures.
