Abstract
Revista Brasileira de Terapia Intensiva. 2016;28(1):49-54
DOI 10.5935/0103-507X.20160013
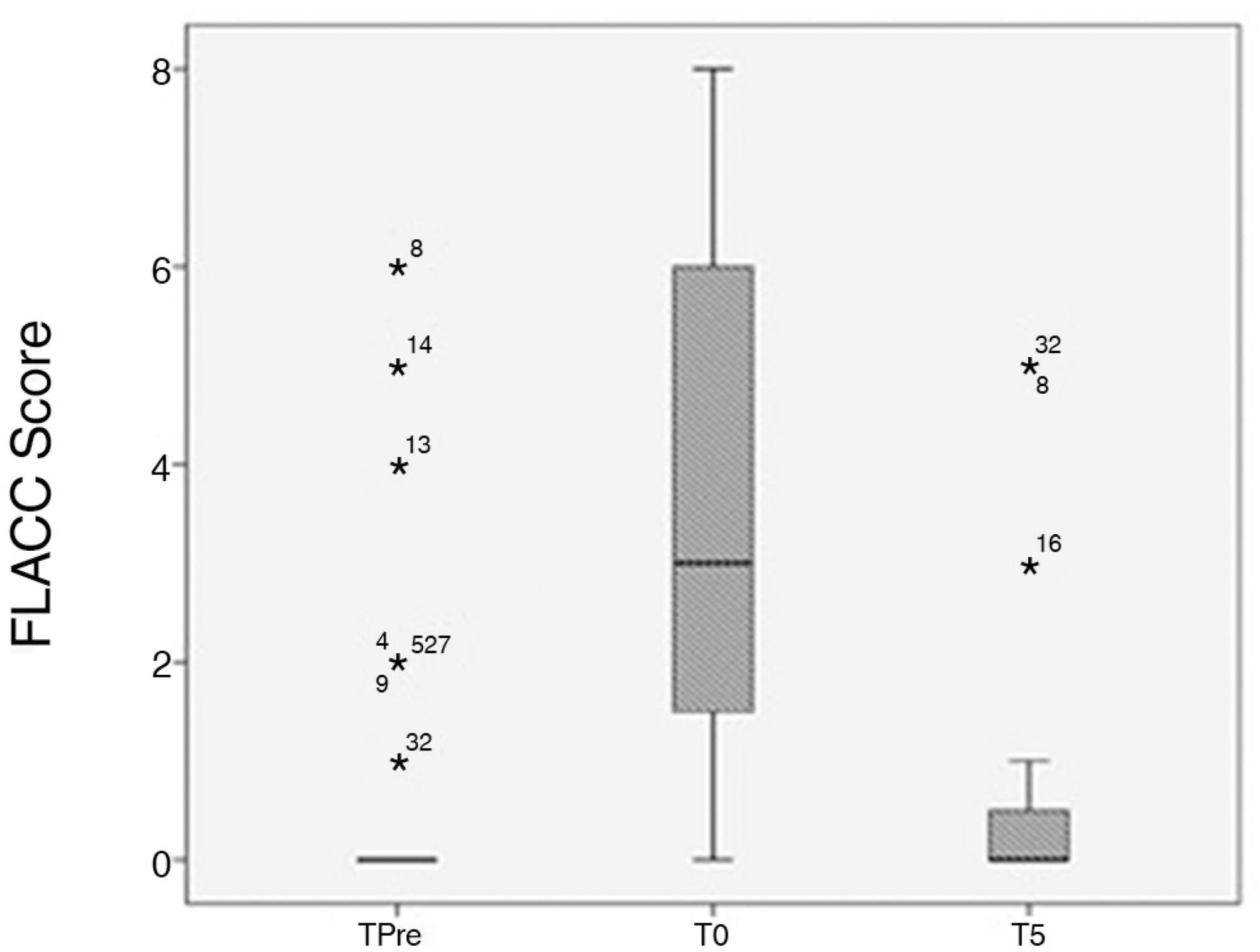
This study assessed pain and observed physiological parameters in sedated and mechanically ventilated children during a routine procedure.
This observational study was performed in a pediatric intensive care unit. Thirty-five children between 1 month and 12 years of age were assessed before, during, and five minutes after an arterial blood collection for gas analysis (painful procedure). Face, Legs, Activity, Cry and Consolability scale was used to assess pain. In addition, patients' heart rate, respiratory rate, peripheral saturation of oxygen and blood pressure (diastolic and systolic) were recorded. COMFORT-B scale was applied before the pain and physiological parameter assessments to verify sedation level of the subjects.
There was an increase in Face, Legs, Activity, Cry and Consolability score (p = 0.0001) during painful stimuli. There was an increase in heart rate (p = 0.03), respiratory rate (p = 0.001) and diastolic blood pressure (p = 0.006) due to pain caused by the routine procedure.
This study suggests that assessments of pain using standard scales, such as Face, Legs, Activity, Cry and Consolability score, and other physiological parameters should be consistently executed to optimize pain management in pediatric intensive care units.
Abstract
Revista Brasileira de Terapia Intensiva. 2016;28(4):472-482
DOI 10.5935/0103-507X.20160080
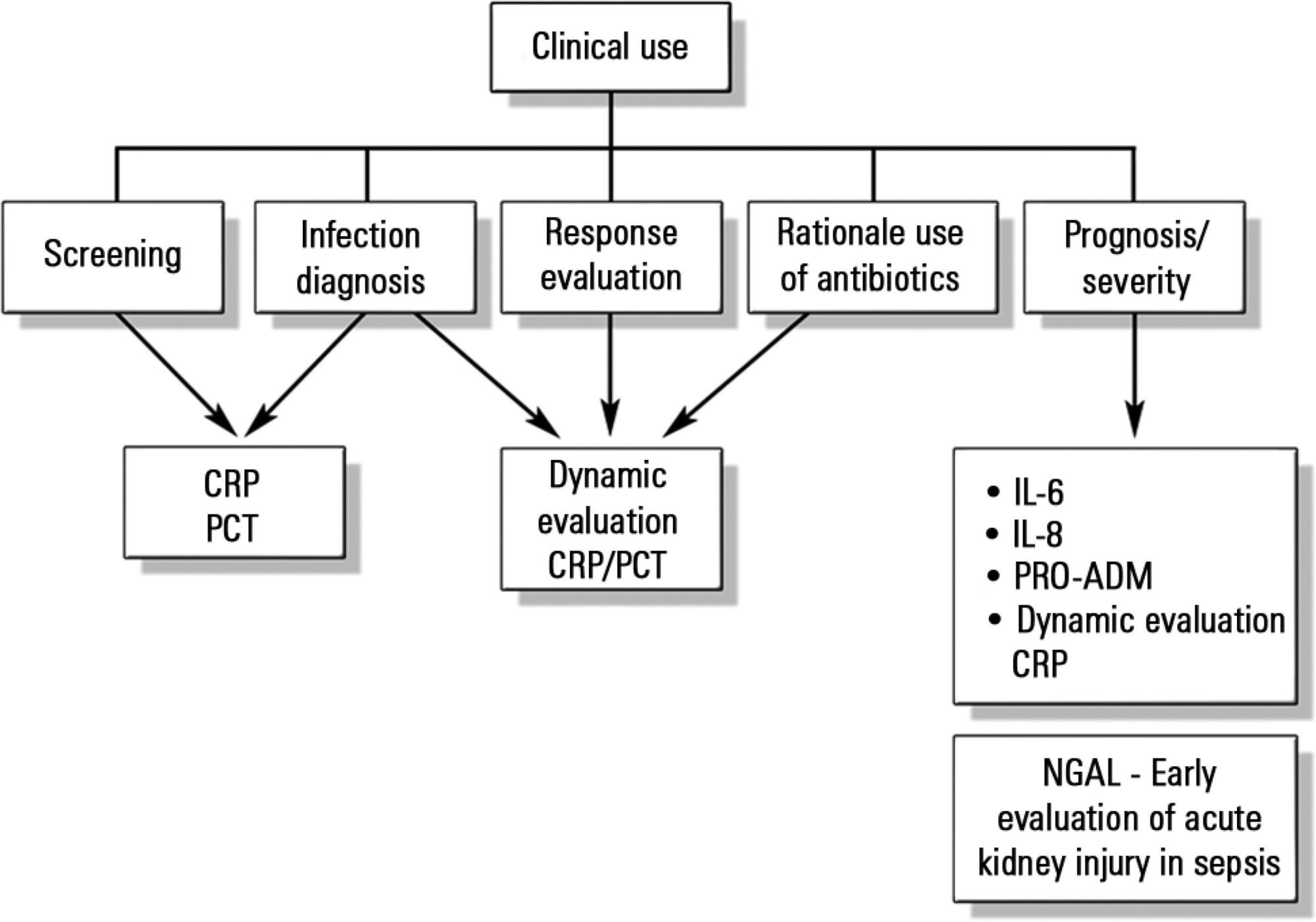
Despite advances in recent years, sepsis is still a leading cause of hospitalization and mortality in infants and children. The presence of biomarkers during the response to an infectious insult makes it possible to use such biomarkers in screening, diagnosis, prognosis (risk stratification), monitoring of therapeutic response, and rational use of antibiotics (for example, the determination of adequate treatment length). Studies of biomarkers in sepsis in children are still relatively scarce. This review addresses the use of biomarkers in sepsis in pediatric patients with emphasis on C-reactive protein, procalcitonin, interleukins 6, 8, and 18, human neutrophil gelatinase, and proadrenomedullin. Assessment of these biomarkers may be useful in the management of pediatric sepsis.
Abstract
Revista Brasileira de Terapia Intensiva. 2015;27(3):240-246
DOI 10.5935/0103-507X.20150044
To determine the etiology and clinical disease progression variables of sepsis associated with the prognosis of patients admitted to a pediatric intensive care unit.
Prospective and retrospective case series. Data were collected from the medical records of patients diagnosed with sepsis who were admitted to the pediatric intensive care unit of a general hospital from January 2011 to December 2013. Bacteria were identified in blood and fluid cultures. Age, sex, vaccination schedule, comorbidities, prior antibiotic use, clinical data on admission, and complications during disease progression were compared in the survival and death groups at a 5% significance level.
A total of 115 patients, with a mean age of 30.5 months, were included in the study. Bacterial etiology was identified in 40 patients. Altered peripheral perfusion on admission and diagnosis of severe sepsis were associated with complications. A greater number of complications occurred in the group of patients older than 36 months (p = 0.003; odds ratio = 4.94). The presence of complications during hospitalization was associated with death (odds ratio = 27.7). The main etiological agents were Gram-negative bacteria (15/40), Staphylococcus aureus (11/40) and Neisseria meningitidis (5/40).
Gram-negative bacteria and Staphylococcus aureus predominated in the etiology of sepsis among children and adolescents admitted to an intensive care unit. The severity of sepsis and the presence of altered peripheral perfusion on admission were associated with complications. Moreover, the presence of complications was a factor associated with death.
Abstract
Revista Brasileira de Terapia Intensiva. 2015;27(3):266-273
DOI 10.5935/0103-507X.20150035
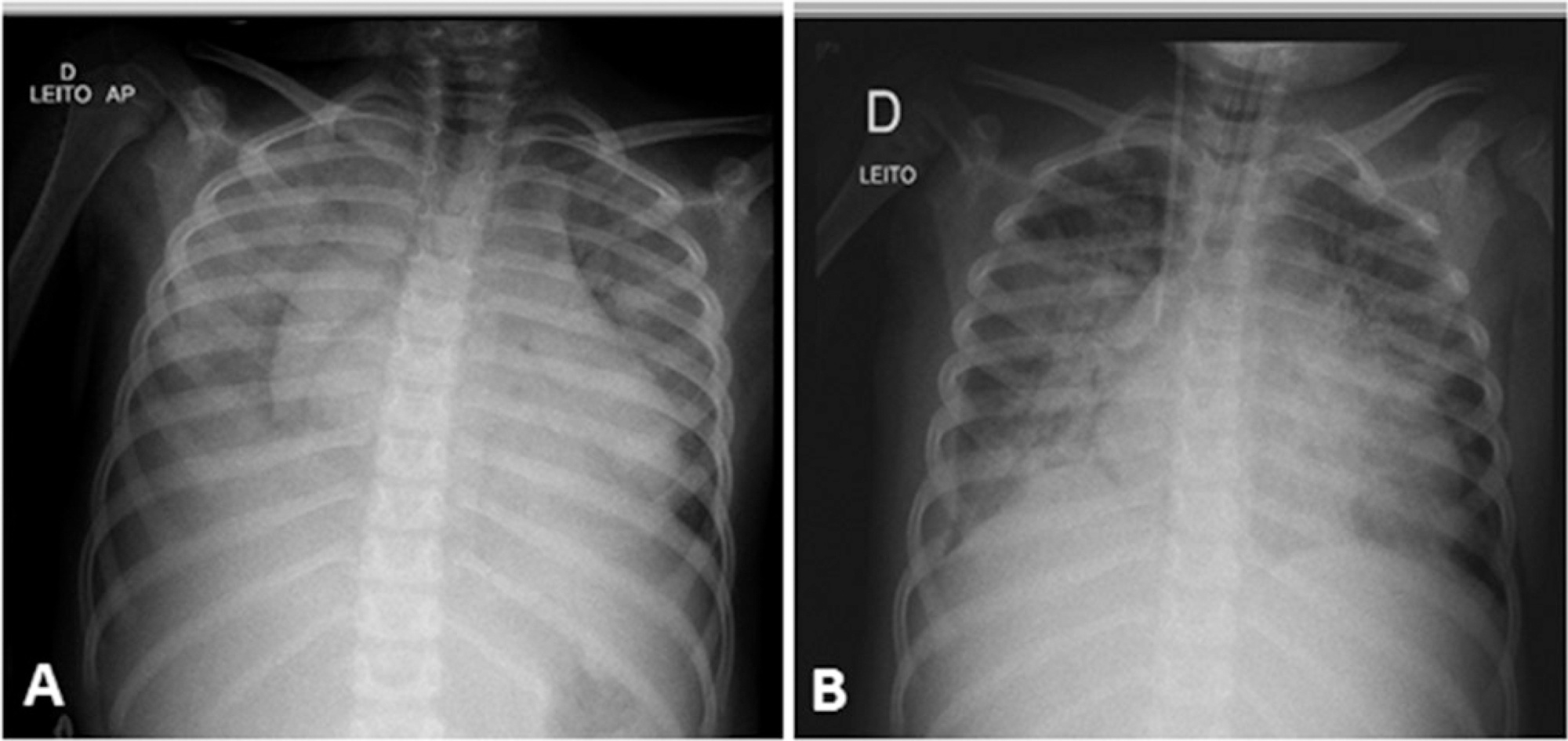
Acute respiratory distress syndrome is a disease of acute onset characterized by hypoxemia and infiltrates on chest radiographs that affects both adults and children of all ages. It is an important cause of respiratory failure in pediatric intensive care units and is associated with significant morbidity and mortality. Nevertheless, until recently, the definitions and diagnostic criteria for acute respiratory distress syndrome have focused on the adult population. In this article, we review the evolution of the definition of acute respiratory distress syndrome over nearly five decades, with a special focus on the new pediatric definition. We also discuss recommendations for the implementation of mechanical ventilation strategies in the treatment of acute respiratory distress syndrome in children and the use of adjuvant therapies.
Abstract
Revista Brasileira de Terapia Intensiva. 2015;27(4):412-415
DOI 10.5935/0103-507X.20150069
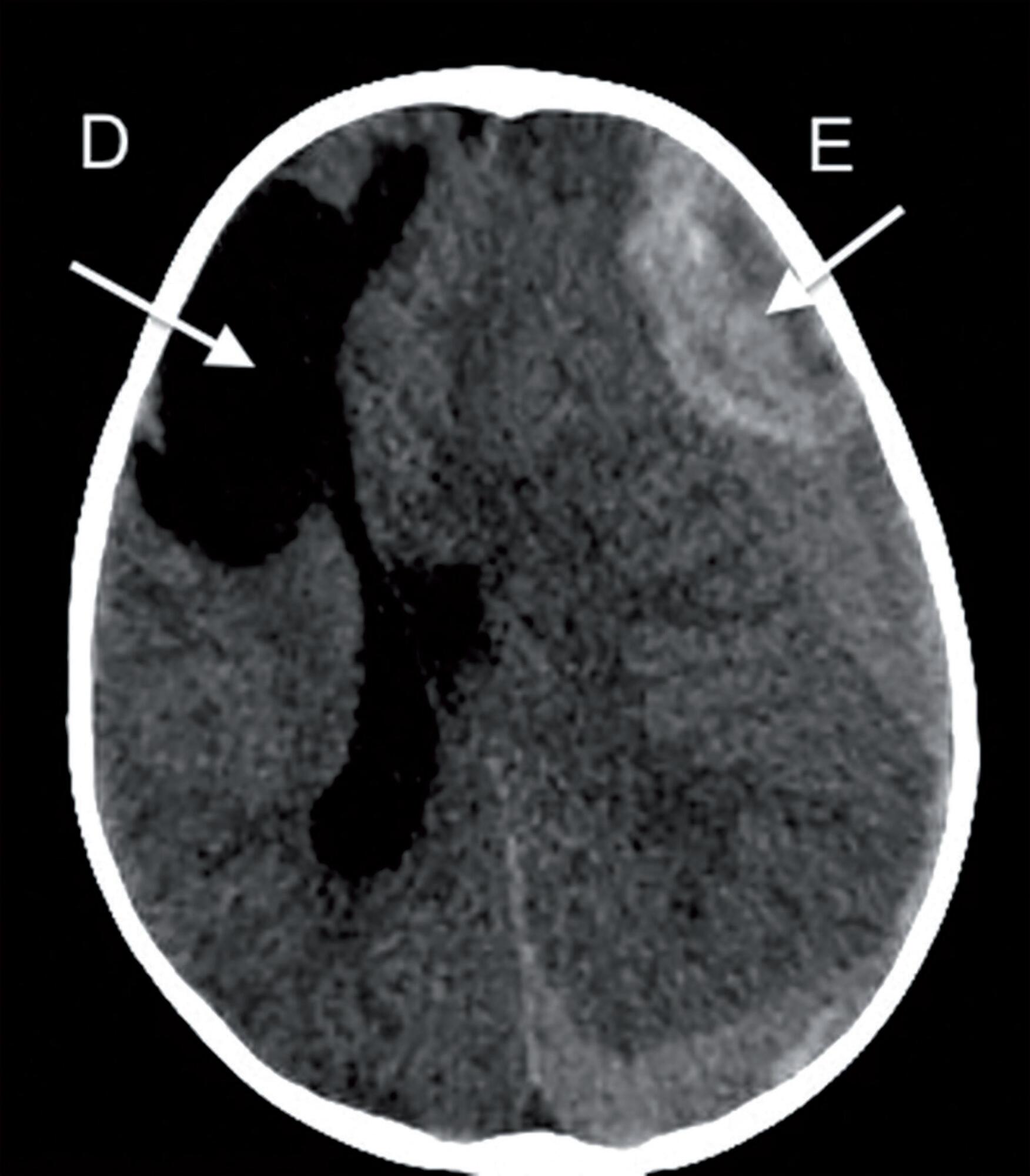
We report the case of a 2-year-old child who survived an acute episode of severe spontaneous intracranial hemorrhage with clinical and radiological signs of intracranial hypertension and transtentorial herniation. The patient underwent emergency surgery to drain the hematoma, and a catheter was inserted to monitor intracranial pressure. In the initial computed tomography analysis performed prior to hematoma drainage, a brain cyst was evident contralateral to the hematoma, which, based on the analysis by the care team, possibly helped to avoid a worse outcome because the cyst accommodated the brain after the massive hemorrhage. After the investigation, the patient was determined to have previously undiagnosed hemophilia A. The patient underwent treatment in intensive care, which included the control of intracranial pressure, factor VIII replacement and discharge without signs of neurological impairment.
Abstract
Revista Brasileira de Terapia Intensiva. 2015;27(4):390-396
DOI 10.5935/0103-507X.20150065
To evaluate the quality of available evidence to establish guidelines for the use of noninvasive ventilation for the management of status asthmaticus in children unresponsive to standard treatment.
Search, selection and analysis of all original articles on asthma and noninvasive ventilation in children, published until September 1, 2014 in all languages in the electronic databases PubMed, Web of Science, Cochrane Library, Scopus and SciELO, located using the search terms: "asthma", "status asthmaticus", "noninvasive ventilation", "Bronchospasm", "continuous positive airway pressure", "child", "infant", "pediatrics", "hypercapnia", "respiratory failure" and the keywords "BIPAP", "CPAP", "Bilevel", "acute asthma" and "near fatal asthma". The articles were assessed based on the levels of evidence of the GRADE system.
Only nine original articles were located; two (22%) articles had level of evidence A, one (11%) had level of evidence B and six (67%) had level of evidence C.
The results suggest that noninvasive ventilation is applicable for the treatment of status asthmaticus in most pediatric patients unresponsive to standard treatment. However, the available evidence cannot be considered as conclusive, as further high-quality research is likely to have an impact on and change the estimate of the effect.
Abstract
Revista brasileira de terapia intensiva. 2014;26(1):44-50
DOI 10.5935/0103-507X.20140007
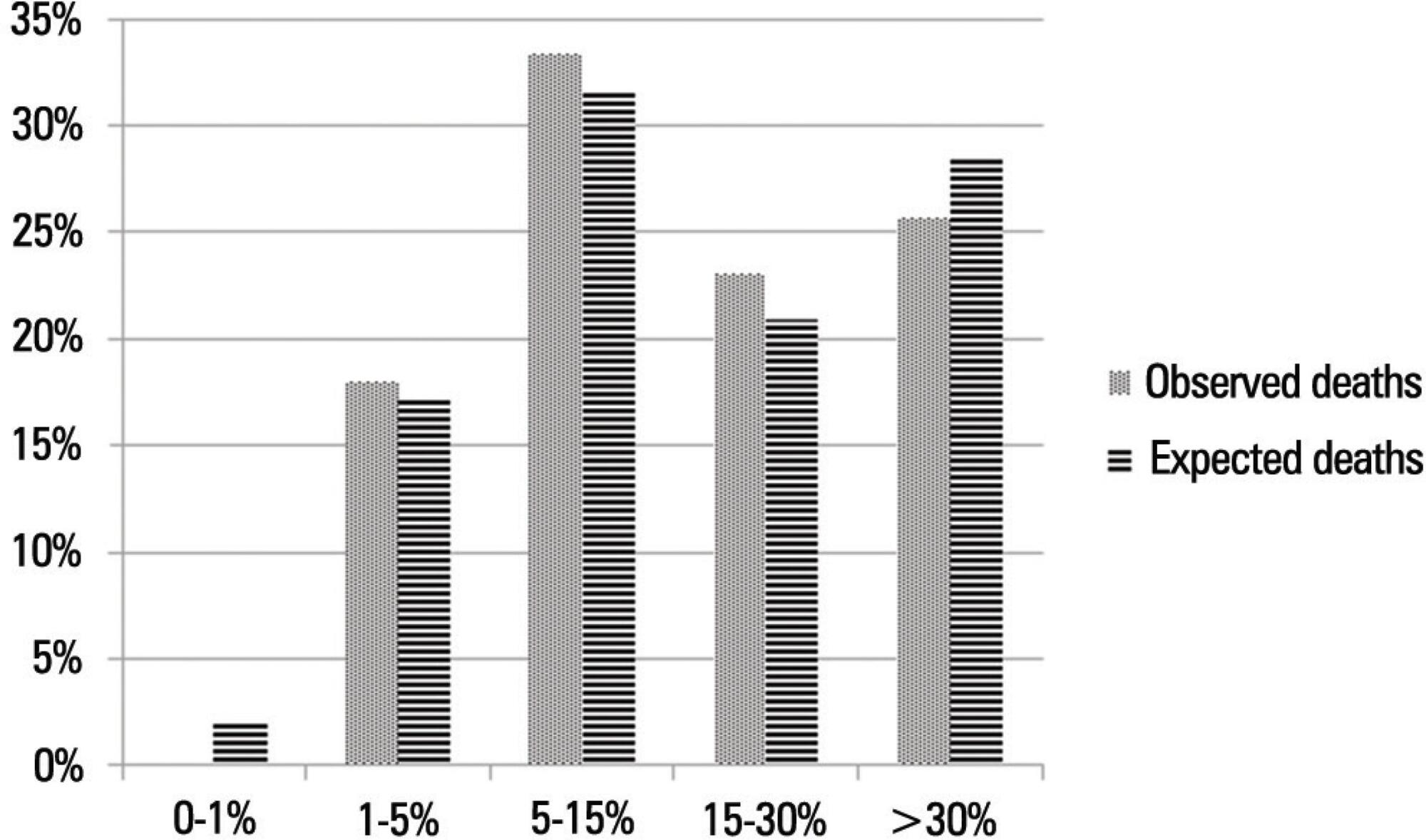
To assess the discrimination and calibration of the Pediatric Index of Mortality 2 in patients admitted to a pediatric intensive care unit.
The study was conducted with a contemporary cohort from November 2005 to November 2006. Patients aged 29 days to 18 years were included in the study. Patients who died within 12 hours of admission and cases of readmission were excluded from the study. The performance of the Pediatric Index of Mortality 2 was assessed by means of the Hosmer-Lemeshow goodness-of-fit test, the standardized mortality ratio and the area under receiver operating characteristic (ROC) curve with 95% confidence interval. The significance level was established as 5%.
A total of 276 admissions to the pediatric intensive care unit were included in the analysis. The mortality rate was 14.13%, and the efficiency of admission 0.88%. The median age of the sample was 42.22 months, and most participants were male (60.1%). Most admissions were referrals from the emergency department. The mean duration of stay in pediatric intensive care unit was 6.43±5.23 days. Approximately 72.46% of admissions were for clinical reasons and exhibited an association with the outcome death (odds ratio: 2.9; 95%CI: 1.09-7.74; p=0.017). Calibration of the Pediatric Index of Mortality 2 with the chi-square statistic was 12.2686 (p=0.1396) in the Hosmer-Lemeshow goodness-of-fit test, and the standardized mortality ratio was 1.0. The area under the ROC curve assessing model discrimination was 0.778.
Pediatric Index of Mortality 2 exhibited satisfactory performance.
Abstract
Revista brasileira de terapia intensiva. 2014;26(3):321-326
DOI 10.5935/0103-507X.20140046
A case of fulminant myocarditis associated with the H1N1 influenza virus. This case report describes the patient's clinical course and emphasizes the importance of bedside echocardiography as an aid in the early diagnosis and management of children with severe myocardial dysfunction. It also discusses aspects relevant to the treatment and prognosis of fulminant myocarditis. The patient was a female, 4 years and 8 months old, previously healthy and with a history of flu symptoms in the past two weeks. The patient was admitted to the emergency room with signs of hemodynamic instability, requiring ventilatory support and vasoactive drugs. The laboratory tests, chest X-ray and echocardiogram suggested the presence of myocarditis. The test for H1N1 in nasopharyngeal secretions was positive. The patient evolved to refractory cardiogenic shock despite the clinical measures applied and died 48 hours after admission to the intensive care unit. The H1N1 influenza virus is an etiological agent associated with acute myocarditis, but there are few reported cases of fulminant myocarditis caused by the H1N1 virus. The identification of signs and symptoms suggestive of fulminant progression should be immediate, and bedside echocardiography is a useful tool for the early detection of myocardial dysfunction and for therapeutic guidance. The use of immunosuppressive therapy and antiviral therapy in acute myocarditis of viral etiology is controversial; hence, the treatment is based on hemodynamic and ventilatory support. The use of hemodynamic support by extracorporeal membrane oxygenation emerges as a promising treatment.