Abstract
Rev Bras Ter Intensiva. 2006;18(3):219-228
DOI 10.1590/S0103-507X2006000300002
BACKGROUND AND OBJECTIVES: There are few epidemiological studies in mechanical ventilation, and the aim of the study is to show how this procedure is being used in Brazil. METHODS: A 1-day point prevalence study was performed in 40 ICUs, with 390 patients; 217 of these patients were in mechanical ventilation. The results evaluated were the characteristics of ventilated patients, their distribution in Brazil, the mechanical ventilation's causes, the main ventilatory modes, the more important ventilators settings, and the weaning stage of mechanical ventilation. RESULTS: The median age of the ventilated patients was 66 years old. The median APACHE II was 20, while the median time of mechanical ventilation was 11 days. Acute respiratory failure occurred in 71% of the patients, coma in 21.2%, acute exacerbation of chronic respiratory failure in 5.5%, and the neuromuscular disease in 2.3%. The volume-controlled ventilation (VCV) (30%), the pressure support ventilation (PSV) (29.5%), and the pressure-controlled ventilation (PCV) (18%) were the ventilatory modes most used; the PSV had been the main mode in weaning (63.5%). The median of tidal volume (8 mL/kg) was higher in VCV. The median of maximal inspiratory pression (30 cmH2O) and the median of positive end-expiration pressure (PEEP) (8 cmH2O) were higher in PCV. CONCLUSIONS: The predominance of ventilated patients in ICUs was marked by clinical severity of them, and a longer hospital stay time; acute respiratory failure was the principal mechanical ventilation cause; VCV and PSV ventilated more patients, with PSV being more used in weaning patients.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):229-233
DOI 10.1590/S0103-507X2006000300003
BACKGROUND AND OBJECTIVES: Gastrointestinal bleeding due to stress ulcer (GB) complicates critical disease, and must be received prophylaxis based on defined criteria. To evaluate the GB prophylaxis in Intensive Care Units (ICU), and to compare with the guidelines. METHODS: We carried out a cross-sectional multicenter study in 21 medical-surgical ICU in Brazil to investigate this issue. For data analysis, these were distributed in 3 sub-groups (high, moderate and low risk for GB). RESULTS: 235 patients were evaluated, with mean age of 57.7 ± 19.5 years and days on ICU 13 ± 19.7. The more common admission ICU diagnoses were sepsis (26%) and postoperative (16.2%) patients. Seventy-three (73%) of the patients were GB high risk, 21.5% moderate and 5.5% low risk. Of the 187 high risk patients, 139 were receiving GB prophylaxis (60% with histamine blockers (HB2) and 39% with proton pump inhibitors (PPI). Of these patients, 25.7% did not receive GU prophylaxis, although indicated it. Of the 55 moderate risk patients, 70.9% wer e receiving GU prophylaxis (22 with HB2 and 17 with PPI). Of the 14 low risk patients, 71% were using GU prophylaxis (6 with HB2 and 4 with PPI). CONCLUSIONS: Almost 80% of the patients made use of GB prophylactic drugs, with no agreement GU risk stratification. This study demonstrated the no adequate GU prophylaxis in the Brazilian ICU.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):234-241
DOI 10.1590/S0103-507X2006000300004
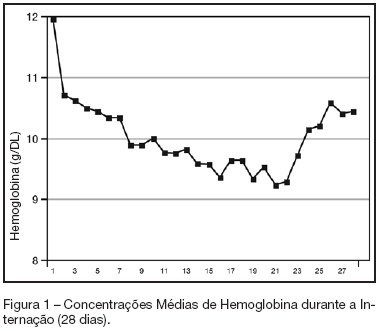
BACKGROUND AND OBJECTIVES: Anemia of critical illness is a multifactorial condition caused by blood loss, frequent phlebotomies and inadequate production of red blood cells (RBC). Controversy surrounds the most appropriate hemoglobin concentration "trigger" for transfusion of RBC. We aimed to evaluate transfusion practices in Brazilian ICUs. METHODS: A prospective study throughout a 2-week period in 19 Brazilian ICUs. Hemoglobin (Hb) level, transfusion rate, organ dysfunction assessment and 28-day mortality were evaluated. Primary indication for transfusion and pretransfusion hemoglobin level were collected for each transfusion. RESULTS: Two hundred thirty-one patients with an ICU length of stay longer than 48h were included. An Hb level lower than 10 g/dL was found in 33% on admission in the ICU. A total of 348 RBC units were transfused in 86 patients (36.5%). The mean pretransfusion hemoglobin level was 7.7 ± 1.1 g/dL. Transfused-patients had significantly higher SOFA score (7.9 ± 4.6 vs 5.6 ± 3.8, p < 0.05, respectively), days on mechanical ventilation (10.7 ± 8.2 vs 7.2 ± 6.4, p < 0.05) and days on vasoactive drugs (6.7 ± 6.4 vs 4.2 ± 4.0, p < 0.05) than non-transfused patients despite similar APACHE II scores (15.2 ± 8.1 vs 14.2 ± 8.1, NS). Transfused patients had higher mortality rate (43.5%) than non-transfused patients (36.3%) (RR 0.60-1.15, NS). Only one patient (0.28%) had febrile non-hemolytic transfusion and urticarial reactions. CONCLUSIONS: Anemia is common in critically ill patients.It seems from the present study that transfusion practices in Brazil have had a more restrictive approach with a lower limit "transfusion trigger".
Abstract
Rev Bras Ter Intensiva. 2006;18(3):242-250
DOI 10.1590/S0103-507X2006000300005
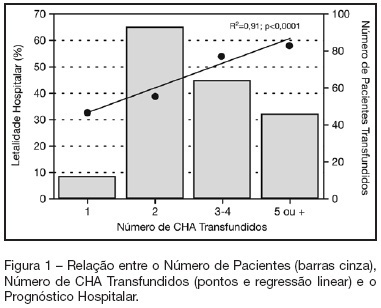
BACKGROUND AND OBJECTIVES: Packed red blood cell (PRBC) transfusion is frequent in intensive care unit (ICU). However, the consequences of anemia in ICU patients are poorly understood. Our aim was to evaluate the prevalence, indications, pre-transfusion hematocrit and hemoglobin levels, and outcomes of ICU patients transfused with PRBC. METHODS: Prospective cohort study conducted at a medical-surgical ICU of a teaching hospital during a 16-month period. Patients' demographic, clinical, laboratory and transfusion-related data were collected. Logistic regression was used after univariate analyses. RESULTS: A total of 698 patients were evaluated and 244 (35%) received PRBC, mainly within the first four days of ICU (82.4%). Transfusion was more frequent in medical and emergency surgical patients. The mean pre-transfusion hematocrit and hemoglobin were 22.8% ± 4.5% and 7.9 ± 1.4 g/dL, respectively. Transfused patients received 4.4 ± 3.7 PRBC during ICU stay and 2.2 ± 1 PRBC at each transfusion. The ICU (39.8% versus 13.2%; p < 0.0001) and hospital (48.8% versus 20.3%; p < 0.0001) mortality rates were higher in transfused patients. Mortality increased as the number of transfused PRBC increased (R² = 0.91). In logistic regression, predictive factors for PRBC transfusion were hepatic cirrhosis, mechanical ventilation (MV), type and duration of ICU admission, and hematocrit. The independent factors associated to hospital mortality were MV, transfusions of more than five PRBC and SAPS II score. CONCLUSIONS: PRBC transfusions are frequent in ICU patients, especially in those with medical and emergency surgical complications, longer ICU stay, and hepatic cirrhosis and in need of MV. Pre-transfusion hemoglobin levels were lower than those previously reported. In our study, PRBC transfusion was associated with increased mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):251-255
DOI 10.1590/S0103-507X2006000300006
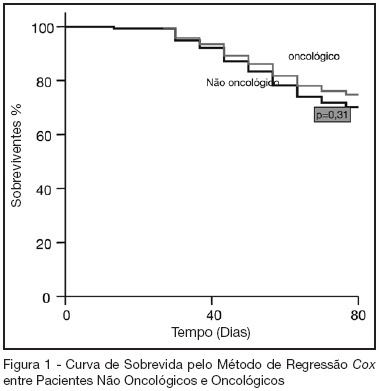
BACKGROUND AND OBJECTIVES: Oncologic diseases are conditions that have influence in the treatment offered to affected patients. The aim of this study was to compare hospitalar outcome of oncologic and non oncologic patients submitted to high risk elective surgery. METHODS: Prospective, observational cohort study realized in an ICU of a tertiary hospital during the period between 04/01/2005 and 07/31/2005. Demographic data, APACHE II and MODS scores and laboratorial and hemodynamic variables were collected and complications like re-intervention need for mechanical ventilation, red blood cell transfusions and pulmonary artery catheter use during the post-operative period were evaluated. All patients were followed until hospital discharge or death. T student and Mann Whitney tests were used to compare numerical variables. Chi-square test was used to compare categorical variables. A p < 0.05 was considered as significant. RESULTS: 119 patients were included in the study. 43 were oncologic and 76 were non-oncologic. 52.9% were female. Mean age was 65.1 ± 14.1 years. Mean APACHE II score was 16.5 ± 5.8 and MODS median was 3 (2-6). Median length of surgery was 5 (3.3-7) hours and ICU and hospital mortality were 10.9% and 25.2%, respectively. Oncologic patients had greater length of hospital stay and length of stay before surgery. These results were statistically significant. Hospital mortality of oncologic patients was not greater than non-oncologic patients (22.4% versus 30.2%, p = 0.32). CONCLUSIONS: In this series, oncologic patients submitted to high risk surgery had the same mortality rate as non-onconlogic patients with similar disease severity.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):256-262
DOI 10.1590/S0103-507X2006000300007
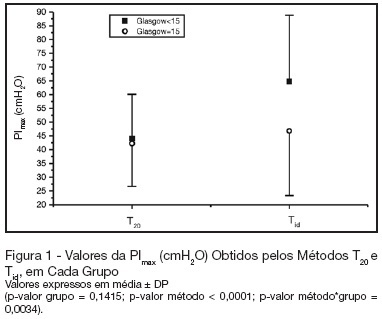
BACKGROUND AND OBJECTIVES: There is no literature consensus about the time of airway occlusion sufficient enough to get a true PImax during weaning from mechanical ventilation (MV). So, the main objectives of the present study were to compare two methods PImax measurement and to evaluate the influence of patients' level of conscience on them. METHODS: The population was composed by 28 general ICU patients, with MV > 48h, in a weaning process, divided into two groups according to Glasgow coma scale score: with (GCS < 15) and without (GCS = 15) alterations of conscience level. The airway was occluded by using an unidirectional valve for 20s (PImaxT20), or for a maximum time of one minute if a plateau of inspiratory pressure was not observed during three consecutive inspirations (PImaxTid). RESULTS: PImaxT20 (mean ± SD, cmH2O) values were similar in both groups (44 ± 16 vs42 ± 15, p = 0.52). However, PImaxTid values, as long as the time needed to their attainment, were greater in GCS < 15 group (65 ± 24 vs 47 ± 23cmH2O and 37 ± 10 vs24 ± 8s, p = 0.04 and 0.0019, respectively). CONCLUSIONS: The method commonly used of 20s airway occlusion seems to be inadequate to get the true PImax in patients with alterations of the level of conscience. Additional studies, now in a more homogeneous group (e. g.: patients with structural brain lesion), are needed to clarify these findings.
Abstract
Rev Bras Ter Intensiva. 2006;18(3):263-267
DOI 10.1590/S0103-507X2006000300008
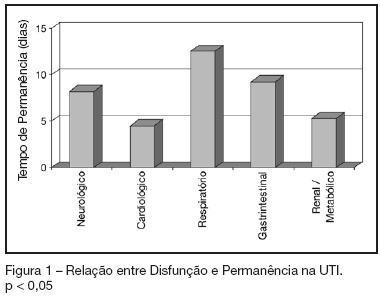
BACKGROUND AND OBJECTIVES: To identify the severity of elderly patients admitted to the intensive care unit (ICU) in a university hospital, relating it to the in-ICU mortality. METHODS: Retrospective study, with analysis of 130 patients admitted to ICU from March 2004 to July 2005. RESULTS: Of the 130 patients, there was a predominance of women, and mean 72.2 ± 7.3 years. There were more patients between 65 and 74 years old. More than 80% of the patients had come from the university hospital itself. The main dysfunctions were from the cardiocirculatory and respiratory systems. Sepsis caused 23.8% of the admissions. Length of stay in ICU was 8.2 ± 7.6 days. The mean of APACHE II was 18.2 ± 7.2. Lesser values of APACHE II, length of stay and mortality were observed in patients with cardiocirculatory dysfunction. The in-ICU mortality was 33.9%, 6.2% before 48 hours. The standardized mortality ratio (SMR) was 0.988. CONCLUSIONS: The age groups did not determine difference between values of APACHE II. They were related neither to higher mortality rate, nor to higher ICU length of stay. Patients with cardiocirculatory dysfunctions had lesser values of APACHE II, ICU length of stay and in-ICU mortality.