Abstract
Rev Bras Ter Intensiva. 2008;20(2):165-172
DOI 10.1590/S0103-507X2008000200009
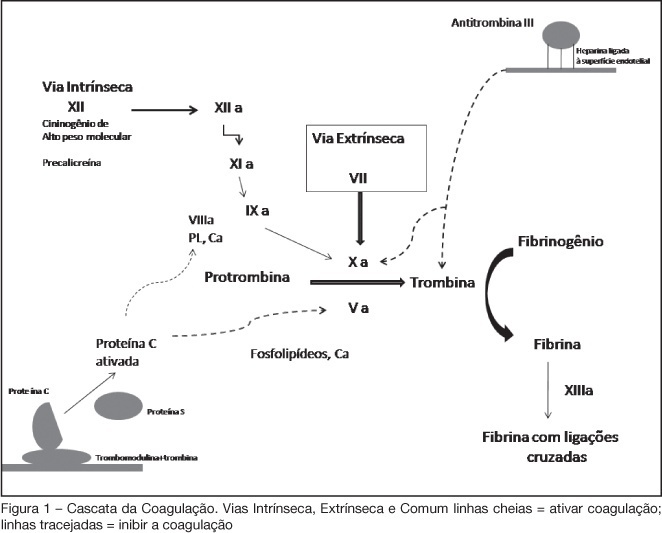
BACKGROUND AND OBJECTIVES: Acute coronary syndromes (ACS) are one of the most common causes of ICU admissions. New drugs have been developed for management of ACS. These drugs reduced morbidity and mortality; however their adverse effects or their incorrect use may cause excessive bleeding. The objective of this review is to present the principal peculiarities, doses, and indications of these drugs in ACS settings. METHODS: Original articles were retrieved crossing the terms acute coronary syndromes and antithrombotic therapy in the MedLine database as well as search for Brazilian and international guidelines in http://sumsearch.uthscsa.edu. RESULTS: In the treatment of acute coronary syndromes with non-ST-segment elevation enoxaparin was as efficient as UFH, but with a simpler management (SYNERGY and A to Z studies). In this same setting, fondaparinux was non inferior to enoxaparin and had lesser bleedings (OASIS 5), bivalirudin, combined or not with GPIIbIIIa blockers, was not inferior when compared with other heparins (ACUITY). In ST-segment elevation ACS, enoxaparin was superior to HNF in patients treated with fibrinolysis (EXTRACT TIMI 25); in OASIS 6 fondaparinux was superior to UFH in patients treated with thrombolytic therapy and not submitted to reperfusion. CONCLUSIONS: The correct management and individual combination of antithrombotic drugs are mandatory for decreased mortality and of major cardiovascular events, reducing the undesirable risk of additional bleeding.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):173-177
DOI 10.1590/S0103-507X2008000200010
BACKGROUND AND OBJECTIVES: The debate on efficacy and patient safety related to the use of drotrecogin alfa (DrotAA) is timely, principally due to the negative results observed in clinical studies performed after the PROWESS study, and the economic cost-related impact of the drug on the healthcare system. The aim of this study was to review the main studies on the use of DrotAA in patients with severe sepsis. The focus was on drug efficacy-and patient safety-related issues. CONTENTS: Articles were selected by a MedLine search for studies on the use of DrotAA in patients with sepsis using the following key words: activated protein C; drotrecogin alfa; sepsis; septic shock; Xigris®. Additional references were retrieved from the studies initially selected. CONCLUSIONS: Mortality and bleeding complications associated with the use of DrotAA were more frequent in large observational studies than those reported in randomized trials. In the light of the current knowledge, routine use of DrotAA should be reevaluated until well-designed confirmatory clinical trials can clarify the true efficacy and safety of the drug and help identify the subgroup of patients that can benefit from use of DrotAA. Physicians should be cautious with the rapid transfer of evidences not well-documented, to the guidelines and recommendations practiced in the care and treatment of patients with severe sepsis.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):178-183
DOI 10.1590/S0103-507X2008000200011
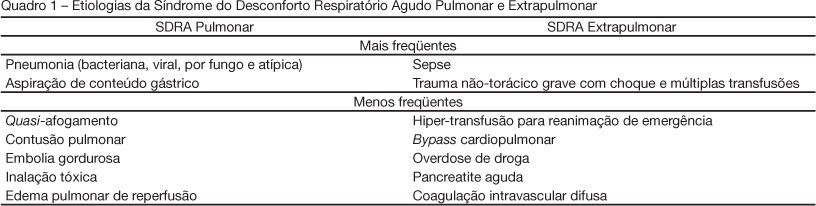
BACKGROUND AND OBJECTIVES: The pathogenesis of acute respiratory distress syndrome (ARDS) has been described by the presence of direct (pulmonary) and/or indirect (extrapulmonary) insult to the lung parenchyma. Evidence indicates that the pathophysiology of ARDS may differ according to the type of primary insult. This article presents a brief overview of differences between pulmonary and extrapulmonary ARDS, and discusses the interactions between morpho-functional aspects and response to differents therapies, both in experimental and clinical studies. CONTENTS: This systematic review included clinical and experimental ARDS studies found in MedLine and SciElo databases in the last 20 years. Many researchers acknowledge that experimental pulmonary and extrapulmonary ARDS are not identical with regard to morpho-functional aspects, the response to positive end-expiratory pressure (PEEP), recruitment manoeuvre, prone position and other adjunctive therapies. However, contradictory results have been reported in different clinical studies, which could be attributed to the difficulty of classifying ARDS in one or the other category, and to the assurance regarding the onset, phase and severity of ARDS in all patients. CONCLUSIONS: Heterogeneous ARDS patients are still considered as belonging to one syndrome, and are therefore treated in a similar manner. Thus, it is important to understand the pathophysiology of pulmonary and extrapulmonary ARDS in an attempt to better treat these patients.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):184-189
DOI 10.1590/S0103-507X2008000200012
BACKGROUND AND OBJECTIVES: Chronic obstructive pulmonary disease (COPD) is defined as a syndrome characterized by usually progressive chronic airflow limitation which is associated to a bronchial hyperresponsiveness and is partially reversible. Noninvasive mechanical ventilation is an alternative treatment for patients with COPD exacerbations. The objective of the literature reviews was to verify noninvasive mechanical ventilation benefits and complications in acute exacerbations of chronic obstructive pulmonary disease in patients. CONTENTS: This national and international's scientific literature review was developed according to criteria established for documentary research in the MedLine, LILACS, SciElo, PubMed and Cochrane, databases using the key words: chronic obstructive pulmonary disease and noninvasive mechanical ventilation. Inclusion criteria were articles published from 1995 to 2007; in English, Spanish and Portuguese; studies in the human model and with no gender restriction. CONCLUSIONS: Noninvasive mechanical ventilation can reduce partial pressure of carbon dioxide, improve gas exchange, alleviate symptoms as dyspnea caused by fatigue of the respiratory muscles, reduce duration of hospitalization, decrease need for invasive mechanical ventilation, reduce number of complications and also lessen hospital mortality. The main complications found were: facial skin erythema, claustrophobia, nasal congestion, face pain, eye irritation, aspiration pneumonia, hypotension, pneumothorax, aerophagia, hypercapnia, gastric insufflation, vomit, bronchoaspiration, morning headaches, face injuries, air embolism and, last but not least, discomfort of the patient. Noninvasive mechanical ventilation can be more effective in patients with moderate-severe exacerbations of COPD and these complications can be minimized by an adequate interface also by the contribution of the physiotherapist experience.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):190-196
DOI 10.1590/S0103-507X2008000200013
BACKGROUND AND OBJECTIVES: Out-of-hospital cardiac arrest is a major cause of death with survival rates as low as 5% to 35%. A large number of patients who survive resuscitation will face significant neurological damage, as a result of the ischemia that occurs both during cardiac arrest and reperfusion. However understanding of the mechanisms responsible for brain damage has not resulted in prognostic improvement. Therapeutic hypothermia after resuscitation may be a valid option associated to reduction of neurological damage. The purpose of this study was to review scientific evidence related to a therapy for patients resuscitated from cardiac arrest. CONTENTS: Description and analysis of the main risk factors associated with neurological damage after resuscitation from cardiac arrest as well as prognostic criteria was carried out. A non-systematic search was conducted in the PubMed data base for papers on a therapeutic approach for patients resuscitated from cardiac arrest. Bibliographic references of reviewed papers were also analyzed. Practical rules were drafted for such an approach. CONCLUSIONS: Patients resuscitated from cardiac arrest face a high level of risk of neurological damage. Therapeutic hypothermia and control of physiological parameters to optimise brain perfusion, may improve prognosis.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):197-204
DOI 10.1590/S0103-507X2008000200014
BACKGROUND AND OBJECTIVES: Acute coronary syndromes result from a disruption of a vulnerable coronary plaque complicated by intraluminal thrombus formation, embolisation, and variable degrees of coronary obstruction. Patients with total occlusion may present with acute ST Elevation Myocardial Infarction (STEMI). Partial vessel obstruction may result in Non-ST-Elevation Acute Myocardial Infarction (NSTEMI) or unstable angina (UA). Clinical symptoms and electrocardiographic changes are the main components of identification of ACS. The rapid and effective triage of such patients regarding presence or absence of ST-segment elevation is critical to dictate further therapeutic strategies. The objective of this chapter was to review current evidence and recommendations for the evaluation and early treatment of acute coronary syndromes. CONTENTS: We performed a clinical review using the electronic databases MedLine and LILACS from January 1990 to September 2007. CONCLUSIONS: Reperfusion of the infarct-related artery is the cornerstone of therapy for STEMI. Fibrinolysis and percutaneous coronary intervention are both well established as effective options. Management of UA/NSTEMI patients requires early risk stratification. High-risk patients should undergo an early invasive strategy that consists in performance of cardiac catheterization in the first 24 to 48 hours of presentation.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):205-209
DOI 10.1590/S0103-507X2008000200015
BACKGROUND AND OBJECTIVES: Palliative care is based on prevention and relief of suffering, identifying, assessing and treating pain and other physical, psychological, social and spiritual problems. Sudden dyspnea is frequently observed in terminal oncologic patients. In these cases, noninvasive ventilation can be an adequate option to control dyspnea promoting comfort and allowing patient interaction with their relatives. The aim of this article was to present the benefits of noninvasive ventilation in the palliative care setting. CASE REPORT: The case of a 29 year old patient, admitted in intensive care unit (ICU), after cesarean section delivery, for clinical treatment of acute respiratory failure is reported. Chest X-ray showed pulmonary mass in the right lung. After clinical and image investigation, metastatic thoracic sarcoma was diagnosed and palliative cares were introduced. The ICU interdisciplinary team chose to use noninvasive ventilation (modality CPAP + PSV) to relieve dyspnea and discomfort, as well as to allow interaction with her baby and family. CONCLUSIONS: Palliative care with noninvasive ventilation contributed to increase comfort of the patient by controlling dyspnea.

Abstract
Rev Bras Ter Intensiva. 2008;20(2):210-212
DOI 10.1590/S0103-507X2008000200016
BACKGROUND AND OBJECTIVES: Pneumocystis jirovecii pneumonia has been one of the most common diseases and life-threatening infectious complications in acquired immunodeficiency syndrome patients. The objective of the case report was to present a patient with probable diagnosis of Pneumocystis jirovecii pneumonia who received noninvasive positive pressure ventilation. CASE REPORT: A female patient, 25 years old, with probable diagnosis of Pneumocystis jirovecii pneumonia received noninvasive positive pressure ventilation. CONCLUSIONS: All respiratory parameters progressively improved in the first five days. Results suggest the efficacy of this support to improve oxygenation, to revert hypoxemia and to prevent orotracheal intubation.