You searched for:"Cassiano Teixeira"
We found (44) results for your search.-
Original Articles
Appropriate medical professionals communication reduces intensive care unit mortality
Rev Bras Ter Intensiva. 2010;22(2):112-117
Abstract
Original ArticlesAppropriate medical professionals communication reduces intensive care unit mortality
Rev Bras Ter Intensiva. 2010;22(2):112-117
DOI 10.1590/S0103-507X2010000200003
Views0See moreOBJECTIVES: Communication issues between healthcare professionals in intensive care units may be related to critically ill patients’ increased mortality. This study aimed to evaluate if communication issues involving assistant physicians and routine intensive care unit physicians would impact critically ill patients’ morbidity and mortality. METHODS: This was a cohort study that included non-consecutive patients admitted to the intensive care unit for 18 months. The patients were categorized in 3 groups according to their assistant doctors’ versus routine doctors communication uses: DC – daily communication during the stay (>75% of the days); EC – eventual communication (25 to 75% of the days); RC – rare communication (< 25% of the days). Demographic data, severity scores, reason for admission to the intensive care unit and interventions were recorded. The consequences of the medical professionals communication failures (delayed procedures, diagnostic tests, antibiotics, ventilatory weaning, vasopressors) and medical prescriptions inadequacies (no bed head elevation, no stress ulceration and deep venous thrombosis drug prophylaxis), and their relationship with the patients outcomes were analyzed. RESULTS: 792 patients were included, and categorized as follows: DC (n=529); EC (n=187) and RC (n=76). The mortality was increased in the RC patients group (26.3%) versus the remainder groups (DC = 13.6% and EC = 17.1%; p<0.05). A multivariate analysis showed that delayed antibiotics [RR 1.83 (CI95%: 1.36 -2.25)], delayed ventilatory weaning [RR 1.63 (CI95%: 1.25-2.04)] and no deep venous thrombosis prophylaxis [RR 1.98 (CI95%: 1.43 - 3.12)] contributed independently for the increased mortality. CONCLUSION: The failure in the assistant and routine intensive care doctors communication may increase the patients’ mortality, particularly due to delayed antibiotics and ventilation weaning, and lack of deep venous thrombosis prophylaxis prescription.
-
Original Articles
Profile and long-term prognosis of glucose tight control in intensive care unit – patients: a cohort study
Rev Bras Ter Intensiva. 2009;21(4):398-403
Abstract
Original ArticlesProfile and long-term prognosis of glucose tight control in intensive care unit – patients: a cohort study
Rev Bras Ter Intensiva. 2009;21(4):398-403
DOI 10.1590/S0103-507X2009000400010
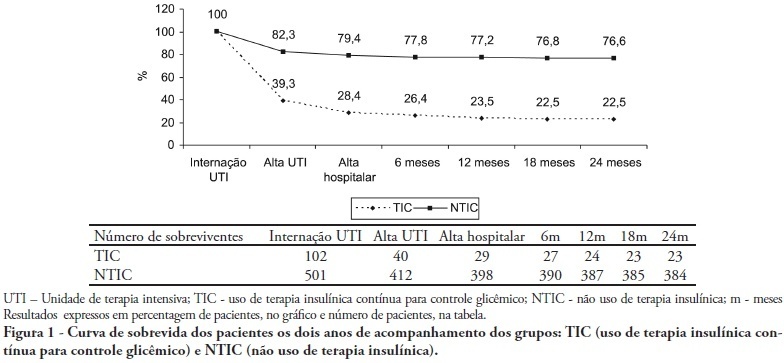
Views0See moreOBJECTIVES: Stress-induced hyperglycemia is frequent in critically ill patients and has been associated with increased mortality and morbidity (both in diabetic and non-diabetic patients). This study objective was to evaluate the profile and long-term prognosis of critically ill patients undergoing tight glucose-control. METHODS: Prospective cohort. All patients admitted to the intensive care unit over 1-year were enrolled. We analyzed demographic data, therapeutic intervention, and short- (during the stay) and long-term (2 years after discharge) mortality. The patients were categorized in 2 groups: tight glucose control and non-tight glucose-control, based on the unit staff decision. RESULTS: From the 603 enrolled patients, 102 (16.9%) underwent tight control (glucose <150 mg/dL) while 501 patients (83.1%) non-tight control. Patients in the TGC-group were more severely ill than those in the non-tight control group [APACHE II score (14 ± 3 versus 11 ± 4, P=0.04), SOFA (4.9 ± 3.2 versus 3.5 ± 3.4, P<0.001) and TISS-24h (25.7 ± 6.9 versus 21.1 ± 7.2, P< 0.001)]. The tight control group patients also had worse prognosis: [acute renal failure (51% versus 18.5%, P<0.001), critical illness neuropathy (16.7% versus 5.6%, P<0.001)] and increased mortality (during the ICU-stay [60.7% versus 17.7%, P<0.001] and within 2-years of the discharge [77.5% versus 23.4%; P<0.001]). CONCLUSION: Critically ill patients needing tight glucose control during the unit stay have more severe disease and have worse short and long-term prognosis.
-
Original Articles
Mortality assessment and quality of life two years after discharge from the ICU: preliminary data from a prospective cohort
Rev Bras Ter Intensiva. 2009;21(1):18-24
Abstract
Original ArticlesMortality assessment and quality of life two years after discharge from the ICU: preliminary data from a prospective cohort
Rev Bras Ter Intensiva. 2009;21(1):18-24
DOI 10.1590/S0103-507X2009000100003
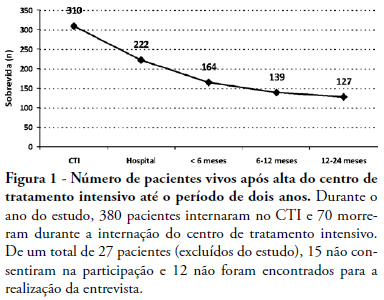
Views0See moreOBJECTIVES: To evaluate mortality and long term quality of life of patients who were discharged from the intensive care unit. METHODS: A prospective cohort, in which all the admitted patients in a intensive care unit (ICU) during 6 months were evaluated and interviewed by telephone after two years of discharge, aiming the completion of two quality of live scales: Karnofsky scale and activities of daily living (ADL) scale. RESULTS: From a total of 380 patients, 100 (26.5%) individuals were alive at the time of interview, 94% living in their homes and 90% without the need for family or specialized care. There was a significant reduction in quality of life of the survivors (Karnofsky pre-ICU = 90±10 vs. Karnofsky after two years = 79±11; p<0.05), although maintaining their functional capacity (ADL pre-ICU = 28±4 vs. ADL after two years = 25±8; p=0.09). This drop in the quality of life occurred mainly to patients who suffered stroke (Karnofsky pre-ICU = 88±7 vs. Karnofsky after two years = 60±15; p<0. 01). CONCLUSION: These preliminary data suggest that the performance of patients after two years of the intensive care discharge is preserved, since they retain the ability to perform self care, except in those with brain damage which shows an inferior quality of life.
-
Stress ulcer prophylaxis in intensive care units: an observational multicenter study
Rev Bras Ter Intensiva. 2006;18(3):229-233
Abstract
Stress ulcer prophylaxis in intensive care units: an observational multicenter study
Rev Bras Ter Intensiva. 2006;18(3):229-233
DOI 10.1590/S0103-507X2006000300003
Views0See moreBACKGROUND AND OBJECTIVES: Gastrointestinal bleeding due to stress ulcer (GB) complicates critical disease, and must be received prophylaxis based on defined criteria. To evaluate the GB prophylaxis in Intensive Care Units (ICU), and to compare with the guidelines. METHODS: We carried out a cross-sectional multicenter study in 21 medical-surgical ICU in Brazil to investigate this issue. For data analysis, these were distributed in 3 sub-groups (high, moderate and low risk for GB). RESULTS: 235 patients were evaluated, with mean age of 57.7 ± 19.5 years and days on ICU 13 ± 19.7. The more common admission ICU diagnoses were sepsis (26%) and postoperative (16.2%) patients. Seventy-three (73%) of the patients were GB high risk, 21.5% moderate and 5.5% low risk. Of the 187 high risk patients, 139 were receiving GB prophylaxis (60% with histamine blockers (HB2) and 39% with proton pump inhibitors (PPI). Of these patients, 25.7% did not receive GU prophylaxis, although indicated it. Of the 55 moderate risk patients, 70.9% wer e receiving GU prophylaxis (22 with HB2 and 17 with PPI). Of the 14 low risk patients, 71% were using GU prophylaxis (6 with HB2 and 4 with PPI). CONCLUSIONS: Almost 80% of the patients made use of GB prophylactic drugs, with no agreement GU risk stratification. This study demonstrated the no adequate GU prophylaxis in the Brazilian ICU.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




