Abstract
Rev Bras Ter Intensiva. 2012;24(3):278-283
DOI 10.1590/S0103-507X2012000300012
OBJECTIVE: This study analyzed acute respiratory failure caused by acute pulmonary edema, as well as chronic obstructive pulmonary disease exacerbation, that was treated with non-invasive mechanical ventilation to identify the factors that are associated with the success or failure non-invasive mechanical ventilation in urgent and emergency service. METHODS: This study was a prospective, descriptive and analytical study. We included patients of both genders aged >18 years who used non-invasive mechanical ventilation due to acute respiratory failure that was secondary to acute pulmonary edema or chronic obstructive pulmonary disease exacerbation. Patients with acute respiratory failure that was secondary to pathologies other than acute pulmonary edema and chronic obstructive pulmonary disease or who presented with contraindications for the technique were excluded. Expiratory pressures between 5 and 8 cmH2O and inspiratory pressures between 10 and 12 cmH2O were used. Supplemental oxygen maintained peripheral oxygen saturation at >90%. The primary outcome was endotracheal intubation. RESULTS: A total of 152 patients were included. The median non-invasive mechanical ventilation time was 6 hours (range 1 - 32 hours) for chronic obstructive pulmonary disease patients (n=60) and 5 hours (range 2 - 32 hours) for acute pulmonary edema patients (n=92). Most (75.7%) patients progressed successfully. However, reduced APACHE II scores and lower peripheral oxygen saturation were observed. These results were statistically significant in patients who progressed to intubation (p<0.001). BiPAP (Bi-level Positive Airway Pressure portable ventilator), as continuous positive airway pressure use increased the probability of endotracheal intubation 2.3 times (p=0.032). Patients with acute pulmonary edema and elevated GCS scores also increased the probability of success. CONCLUSION: Respiratory frequency >25 rpm, higher APACHE II scores, BiPAP use and chronic obstructive pulmonary disease diagnosis were associated with endotracheal intubation. Higher GCS and SpO2 values were associated with NIV success. Non-invasive mechanical ventilation can be used in emergency services in acute respiratory failure cases caused by acute pulmonary edema and chronic obstructive pulmonary disease exacerbation, but patients with variables related to a higher percentage of endotracheal intubation should be specially monitored.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):199-206
DOI 10.1590/S0103-507X2011000200013
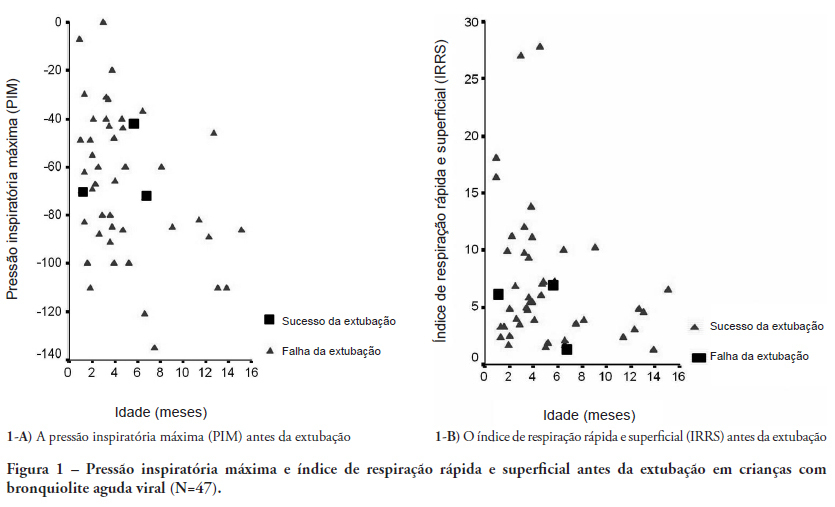
OBJECTIVES: Between 10% and 20% of children submitted to mechanical ventilation in the pediatric intensive care unit present extubation failure. Several ventilatory indexes have been proposed to predict extubation failure. The aim of this study was to analyze the accuracy of these indices in predicting successful extubation in children and to evaluate these variables according to the age of the patient and the specific disease. METHODS: A prospective observational study including all children submitted to mechanical ventilation in a Brazilian referral pediatric intensive care unit was conducted between August 2007 and August 2008. The tidal volume, maximal negative inspiratory pressure, rapid shallow breathing index and other ventilatory indexes were measured before extubation. These variables were analyzed according to the extubation outcome (success or failure) as well as age and specific disease (post cardiac surgery and acute viral bronchiolitis). RESULTS: A total of 100 patients were included (median age of 2.1 years old). Extubation failure was observed in 13% and was associated with lower weight (10.3+8.1 Kg vs. 5.5+2.4 Kg; p=0.01). We also evaluated the relationship between extubation failure and the main cause indicating mechanical ventilation: children who had received cardiac surgery (n=17) presented an extubation failure rate of 29.4% with a relative risk of 4.6 (1.2-17.2) when compared to children with acute viral bronchiolitis (n=47, extubation failure rate of 6.4%). The maximal inspiratory pressure was the only physiologic variable independently associated with the outcome. However, this variable showed a wide dispersion and lack of accuracy for predicting extubation success (sensitivity of 82% and specificity of 55% for a cut point of -37.5 cmH2O predicting successful extubation). The same wide dispersion was observed with other ventilatory indexes. CONCLUSION: The indexes for predicting extubation success in children submitted to mechanical ventilation are not accurate; they vary widely depending on age, main disease and other clinical aspects. New formulas including clinical variables should be developed for better prediction of extubation success in children submitted to mechanical ventilation
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)