Abstract
Rev Bras Ter Intensiva. 2020;32(4):542-550
DOI 10.5935/0103-507X.20200091
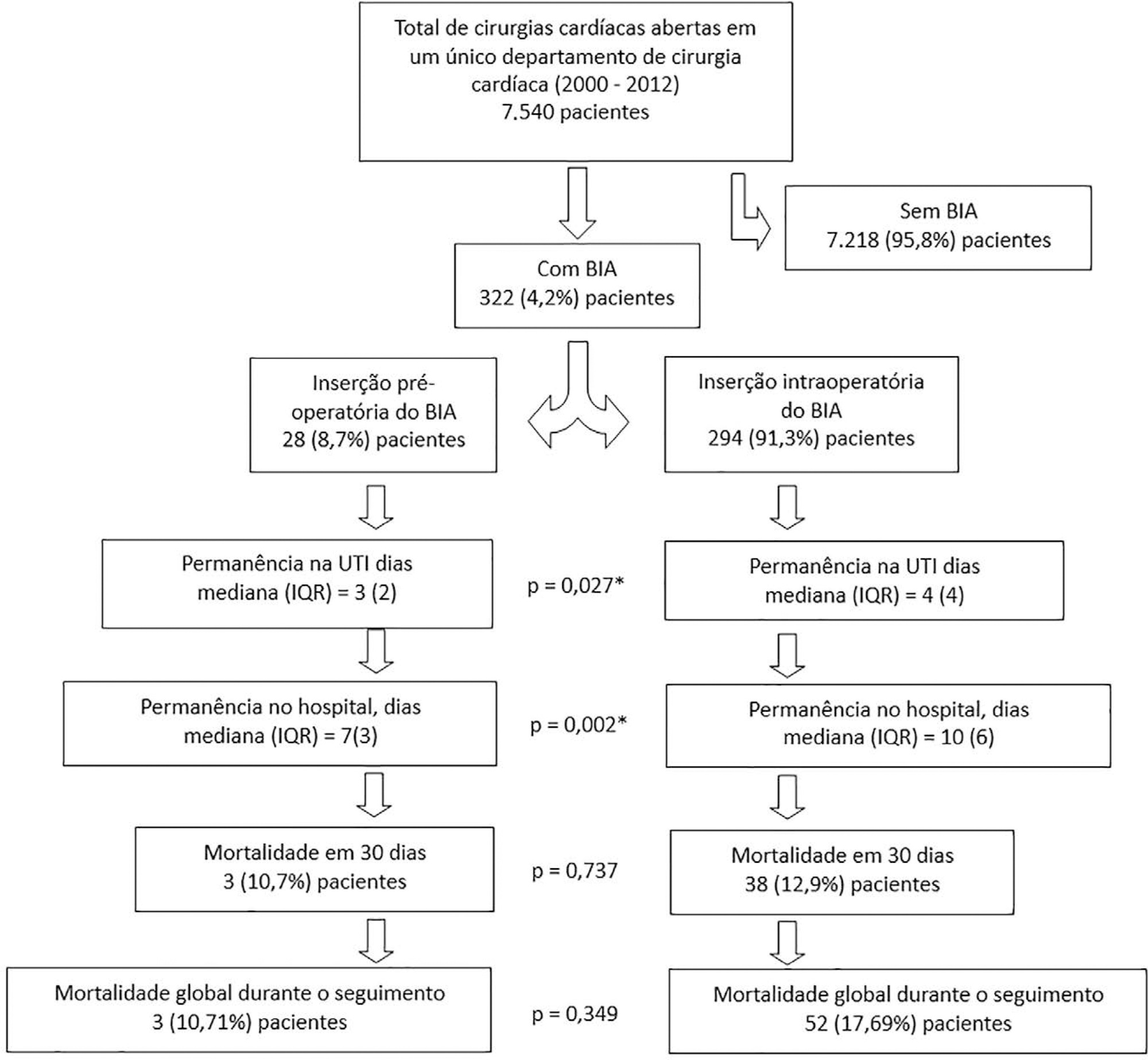
To assess whether preoperative versus intraoperative insertion of an intra-aortic balloon pump is associated with lower 30-day mortality or reduced length of hospital stay among patients who had an intra-aortic balloon pump inserted for cardiac surgery.
This was an observational study of patients who had an intra-aortic balloon pump inserted in the preoperative or intraoperative period of cardiac surgery in our department between 2000 and 2012. We assessed the association between preoperative versus intraoperative insertion of an intra-aortic balloon pump and 30-day mortality in a multivariable logistic regression analysis, including preoperative New York Heart Association class, postoperative atrial fibrillation, reoperation, postoperative creatinine and isolated coronary bypass grafting as cofactors. We used a multivariate linear model to assess whether a preoperative versus intraoperative intra-aortic balloon pump was associated with length of postoperative hospital stay, adjusting for reoperation, isolated coronary bypass grafting, heart valve surgery, sex, age, cardiopulmonary bypass time, aortic cross-clamp time, preoperative patients’ status (elective, urgency or emergency surgery) and preoperative myocardial infarction.
Overall, 7,540 consecutive patients underwent open heart surgery in our department, and an intra-aortic balloon pump was inserted pre- or intraoperatively in 322 (4.2%) patients. The mean age was 67 ± 10.2 years old, the 30-day mortality was 12.7%, and the median length of hospital stay was 9 days (7 - 13). Preoperative versus intraoperative intra-aortic balloon pump insertion did not affect the incidence of 30-day mortality (adjusted OR = 0.69; 95% CI, 0.15 - 3.12; p = 0.63) and length of postoperative hospital stay (β = 5.3; 95%CI, -1.6 to 12.8; p = 0.13).
Preoperative insertion of an intra-aortic balloon pump was not associated with a lower 30-day mortality or reduced length of postoperative hospital stay compared to intraoperative insertion.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):551-556
DOI 10.5935/0103-507X.20200092
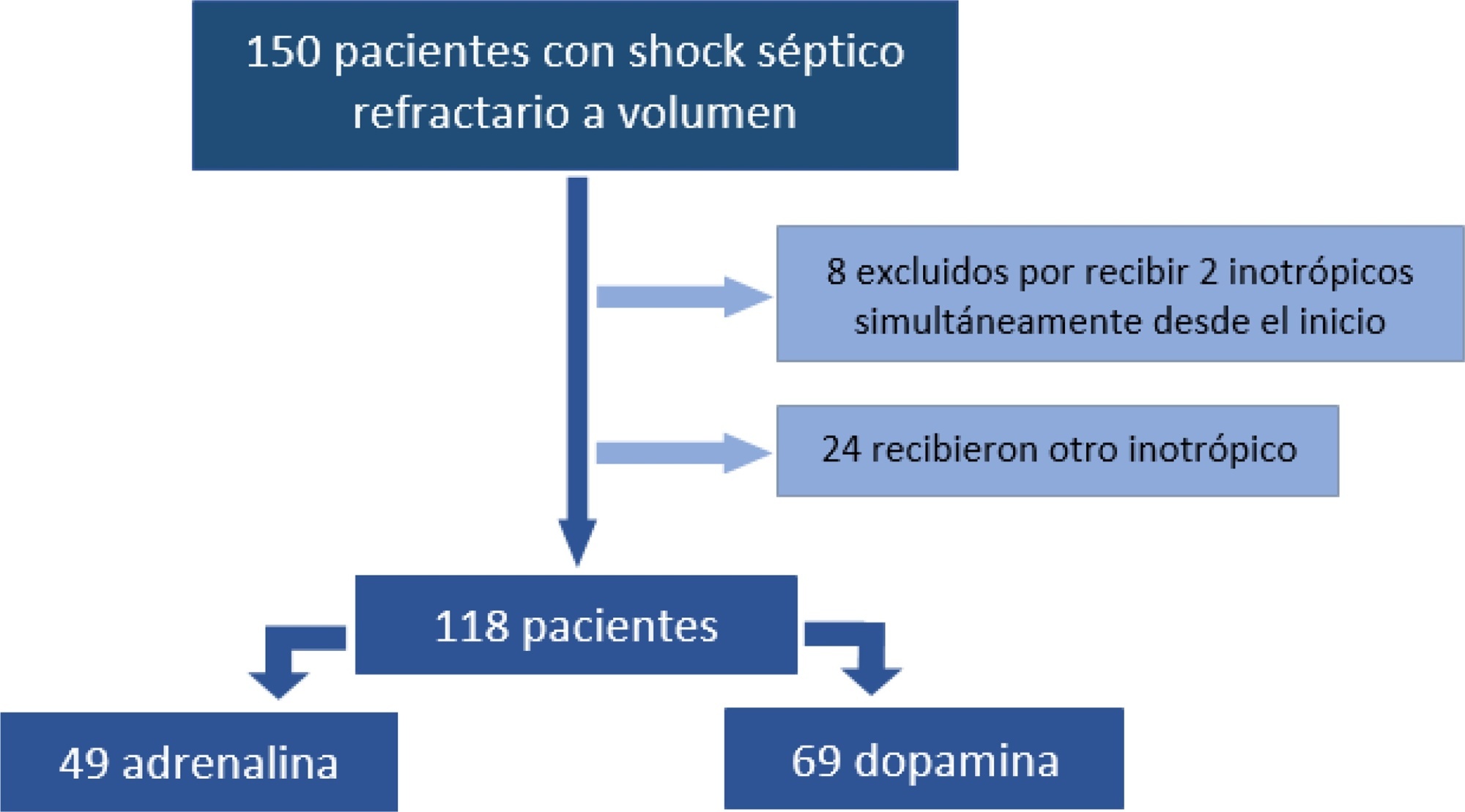
To analyze the clinical outcome of children with fluid-refractory septic shock initially treated with dopamine or epinephrine.
A retrospective cohort study was conducted at a pediatric emergency department of a tertiary hospital. Population: children admitted because of fluid-refractory septic shock. Clinical outcome was compared between two groups: Dopamine and Epinephrine. Variables evaluated were use of invasive mechanical ventilation, days of inotropic therapy, length of hospital stay, intensive care stay, and mortality. For numerical and categorical variables, we used measures of central tendency. They were compared by the Mann-Whitney U-test and the (2 test.
We included 118 patients. A total of 58.5% received dopamine and 41.5% received epinephrine. The rate of invasive mechanical ventilation was 38.8% for epinephrine versus 40.6% for dopamine (p = 0.84), with a median of 4 days for the Epinephrine Group and 5.5 for the Dopamine Group (p = 0.104). Median time of inotropic therapy was 2 days for both groups (p = 0.714). Median hospital stay was 11 and 13 days for the Epinephrine and Dopamine groups, respectively (p = 0.554), and median stay in intensive care was 4 days (0 - 81 days) in both groups (p = 0.748). Mortality was 5% for the Epinephrine Group versus 9% for the Dopamine Group (p = 0.64).
At our center, no differences in use of invasive mechanical ventilation, time of inotropic therapy, length of hospital stay, length of intensive care unit stay, or mortality were observed in children admitted to the pediatric emergency department with a diagnosis of fluid-refractory septic shock initially treated with dopamine versus epinephrine.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):564-570
DOI 10.5935/0103-507X.20200094
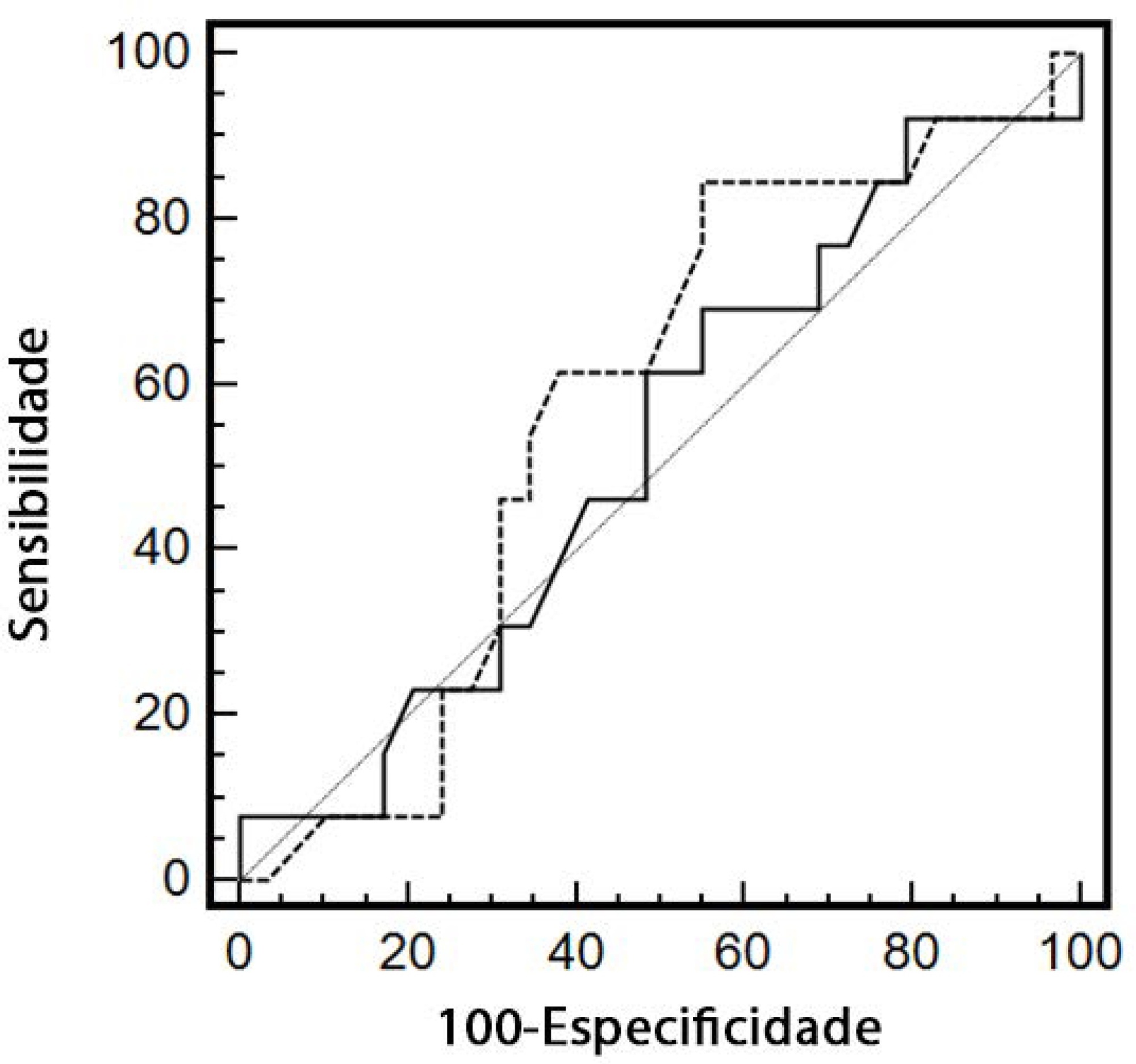
To evaluate renal responsiveness in oliguric critically ill patients after a fluid challenge.
We conducted a prospective observational study in one university intensive care unit. Patients with urine output < 0.5mL/kg/h for 3 hours with a mean arterial pressure > 60mmHg received a fluid challenge. We examined renal fluid responsiveness (defined as urine output > 0.5mL/kg/h for 3 hours) after fluid challenge.
Forty-two patients (age 67 ± 13 years; APACHE II score 16 ± 6) were evaluated. Patient characteristics were similar between renal responders and renal nonresponders. Thirteen patients (31%) were renal responders. Hemodynamic or perfusion parameters were not different between those who did and those who did not increase urine output before the fluid challenge. The areas under the receiver operating characteristic curves were calculated for mean arterial pressure, heart rate, creatinine, urea, creatinine clearance, urea/creatinine ratio and lactate before the fluid challenge. None of these parameters were sensitive or specific enough to predict reversal of oliguria.
After achieving hemodynamic stability, oliguric patients did not increase urine output after a fluid challenge. Systemic hemodynamic, perfusion or renal parameters were weak predictors of urine responsiveness. Our results suggest that volume replacement to correct oliguria in patients without obvious hypovolemia should be done with caution.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):571-577
DOI 10.5935/0103-507X.20200095
To describe the results from the implementation of a respiratory care and mechanical ventilation protocol on potential lung donors who met the conditions for procurement. The secondary objective is to compare the results with historical data.
This was a retrospective, observational study. It included potential donors suitable for procurement of organs who had brain death and were hospitalized in critical care units of the Autonomous City of Buenos Aires from April 2017 to March 2018. Main variables: number of potential lung donors that reached the objective of procurement, rate of lungs procured, and rate of implanted lungs. Values of p < 0.05 were considered significant.
Thirty potential lung donors were included, and 23 (88.5%; 95%CI 69.8 - 97.6) met the oxygenation objective. Twenty potential lung donors donated organs, of whom eight donated lungs, with which four double lung transplants and eight single lung transplants were performed. Seven of 12 lungs were procured and implanted in the preprotocol period, while all 12 were under the protocol (p = 0.38). The implantation rate was 58.3% (7/12) in the historical control period and 100% (12/12) (p = 0.04) in the study period.

Abstract
Rev Bras Ter Intensiva. 2020;32(4):578-584
DOI 10.5935/0103-507X.20200096
To determine the concordance of mortality risk classification through the use of the Pediatric Index of Mortality (PIM) 2 and 3.
Through a retrospective cohort, we evaluated patients admitted to the pediatric intensive care unit between April 2016 and December 2018. We calculated the mortality risk with the PIM 2 and 3. Analyses were carried out to determine the concordance between the risk classification obtained with both scales using unweighted and linearly weighted kappa.
A total of 722 subjects were included, and 66.6% had a chronic condition. The overall mortality was 3.7%. The global kappa concordance coefficient for classifying patients according to risk with the PIM 2 and 3 was moderate at 0.48 (95%CI 0.43 - 0.53). After linear weighting, concordance was substantial at 0.64 (95%CI 0.59 - 0.69). For cardiac surgery patients, concordance for risk classification was fair at 0.30 (95%CI 0.21 - 0.39), and after linear weighting, concordance was only moderate at 0.49 (95%CI 0.39 - 0.59). The PIM 3 assigned a lower risk than the PIM 2 in 44.8% of patients in this subgroup.
Our study proves that the PIM 2 and 3 are not clinically equivalent and should not be used interchangeably for quality evaluation across pediatric intensive care units. Validation studies must be performed before using the PIM 2 or PIM 3 in specific settings.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):585-591
DOI 10.5935/0103-507X.20200084
Sepsis is a systemic infection that causes multiple organ dysfunction. HSP70 is a protein responsive to cell stress, in particular oxidative stress. Therefore, this literature review sought to investigate the roles of HSP70 and oxidative stress in the pathophysiology of sepsis and the possibility of HSP70 as a therapeutic target. HSP70 exerts a protective effect when located in cells (iHSP70), and its decrease, as well as its increase in the extracellular environment (eHSP70), under oxidative stress is a biomarker of sepsis severity. In addition, therapies that increase iHSP70 and treatment with HSP70 promote sepsis improvement.