Abstract
Rev Bras Ter Intensiva. 2007;19(2):176-181
DOI 10.1590/S0103-507X2007000200006
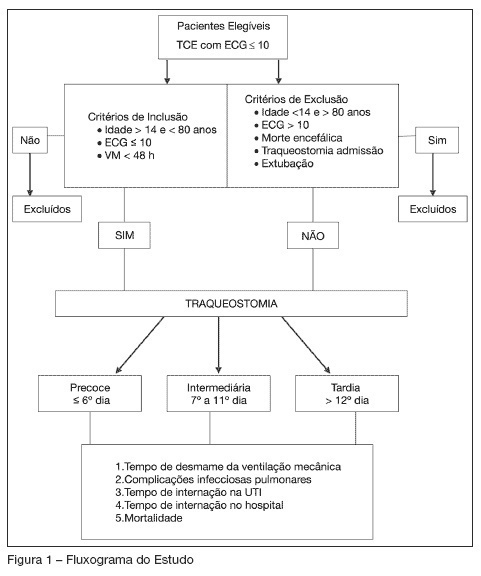
BACKGROUND AND OBJECTIVES: Actually, It’s doubtful if early tracheostomy (ET) can influence mechanical ventilation (MV) weaning time or the hospital length of stay in patients with traumatic brain injury (TBI). The main objective of this trial was to verify the influence of ET on weaning time of patients with severe TBI. METHODS: Prospective, observational study, including 33 patients with severe TBI (GCS < 10 at hospital admission), evaluated according to tracheostomy performance time (early: t < 6 days; intermediate: t = 7 to 11 days; and late: t > 12 days) and the weaning from MV. RESULTS: Total ventilation mechanical time has been reduced in the early tracheostomy group (n = 10; p < 0.0001). A lower GCS punctuation (mean 5.3 ± 2.5) in ET group has been negatively correlated with hospital length of stay (LOS) (p = 0.02). CONCLUSIONS: Early tracheostomy can decrease mechanical ventilation time, but does not influence hospital LOS in patients with severe traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2007;19(1):44-52
DOI 10.1590/S0103-507X2007000100006
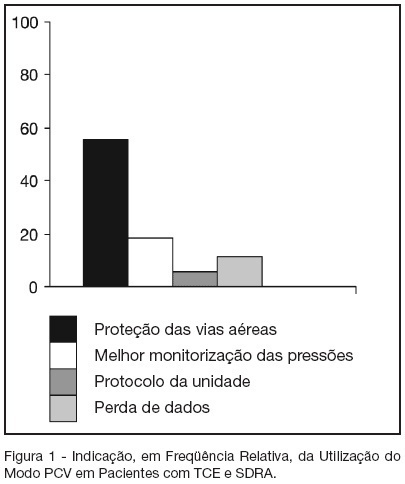
BACKGROUND AND OBJECTIVES: The traumatic brain injury (TBI) is a healthy-world problem, some of his patients develop respiratory failure, requiring intubation and mechanical ventilation, and the most common complications are the acute respiratory distress syndrome (ARDS). In this way, this study has the objective describe the daily clinical practice of respiratory care in this patients submit mechanical ventilation. METHODS: The methods and ventilatories parameters used to ventilate the patients with TBI and ARDS has been evaluated by a sample of physiotherapists from the city of Salvador, BA, from a descriptive study. The data were collected by face-to-face interviews in the period of October 2005 to March 2006. For in such way a half structuralized questionnaire was elaborated contends changeable social-demographic, about the hospital profile and the applied ventilatory strategy in patients with TBI that come to develop ARDS. RESULTS: The sample was composed by 70 physiotherapists, 41 (58.6%) was female, with mean of age of 31.2 ± 6.4 (24-49) years-old and graduated time 7.7 ± 6.4 (1-27) years, which 37 (52.9%) works on public hospital; 67 (95.7%) has any specialization. Sixty four physiotherapists affirm the usage of the pressure controlled ventilation mode. The peak pressure and the plateau pressure wanted to ventilate the patients with TBI and ARDS were in mean 35.6 ± 5,3 (25-50) and 28,4 ± 5,8 (15-35) cmH2O respectively. Forty eighty (68.6%) of the interviewed wants a PaCO2 in 30-35 mmHg. Thirty one (44.3%) of the interviewed finds the ideal PEEP through the best SpO2 with minor FiO2. CONCLUSIONS: It's incontestable that the ventilatory strategy of a patient with severe TBI that become to develop ALI or ARDS is an authentic challenge; a predilection for PCV mode is observed due to the already known protective ventilation strategy.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)