Abstract
Rev Bras Ter Intensiva. 2018;30(3):286-293
DOI 10.5935/0103-507X.20180051
This study aimed to study the incidence of stress hyperglycemia in critically ill children and to investigate the etiological basis of the hyperglycemia based on homeostasis model assessment.
This was a prospective cohort study in one of the pediatric intensive care units of Cairo University, including 60 critically ill children and 21 healthy controls. Serum blood glucose, insulin, and C-peptide levels were measured within 24 hours of admission. Homeostasis model assessment was used to assess β-cell function and insulin sensitivity.
Hyperglycemia was estimated in 70% of patients. Blood glucose values ≥ 180mg/dL were associated with a poor outcome. Blood glucose levels were positively correlated with Pediatric Risk for Mortality (PRISM III) score and number of organ dysfunctions (p = 0.019 and p = 0.022, respectively), while insulin levels were negatively correlated with number of organ dysfunctions (r = −0.33, p = 0.01). Homeostasis model assessment revealed that 26 (43.3%) of the critically ill patients had low β-cell function, and 18 (30%) had low insulin sensitivity. Combined pathology was detected in 2 (3.3%) patients only. Low β-cell function was significantly associated with the presence of multi-organ dysfunction; respiratory, cardiovascular, and hematological dysfunctions; and the presence of sepsis.
β-Cell dysfunction appeared to be prevalent in our cohort and was associated with multi-organ dysfunction.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):496-507
DOI 10.5935/0103-507X.20180071
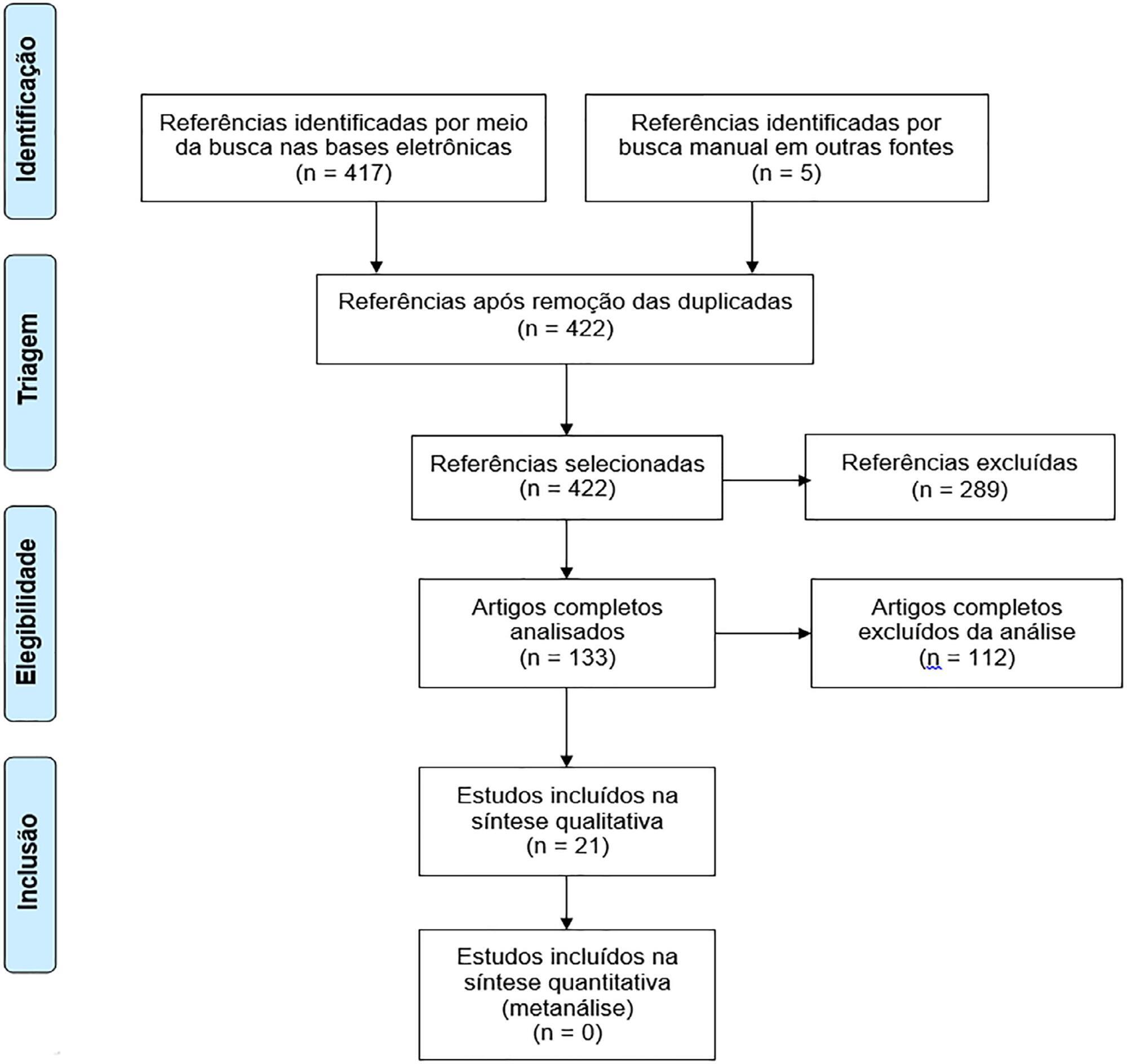
To assess the long-term, health-related quality of life of intensive care unit survivors by systematic review.
The search for, and selection and analysis of, observational studies that assessed the health-related quality of life of intensive care unit survivors in the electronic databases LILACS and MEDLINE® (accessed through PubMed) was performed using the indexed MESH terms "quality of life [MeSH Terms]" AND "critically illness [MeSH Terms]". Studies on adult patients without specific prior diseases published in English in the last 5 years were included in this systematic review. The citations were independently selected by three reviewers. Data were standardly and independently retrieved by two reviewers, and the quality of the studies was assessed using the Newcastle-Ottawa scale.
In total, 19 observational cohort and 2 case-control studies of 57,712 critically ill patients were included. The follow-up time of the studies ranged from 6 months to 6 years, and most studies had a 6-month or 1-year follow up. The health-related quality of life was assessed using two generic tools, the EuroQol and the Short Form Health Survey. The overall quality of the studies was low.
Long-term, health-related quality of life is compromised among intensive care unit survivors compared with the corresponding general population. However, it is not significantly affected by the occurrence of sepsis, delirium, and acute kidney injury during intensive care unit admission when compared with that of critically ill patient control groups. High-quality studies are necessary to quantify the health-related quality of life among intensive care unit survivors.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):317-326
DOI 10.5935/0103-507X.20180052
To characterize the transport of severely ill patients with extracorporeal respiratory or cardiovascular support.
A series of 18 patients in the state of São Paulo, Brazil is described. All patients were consecutively evaluated by a multidisciplinary team at the hospital of origin. The patients were rescued, and extracorporeal membrane oxygenation support was provided on site. The patients were then transported to referral hospitals for extracorporeal membrane oxygenation support. Data were retrieved from a prospectively collected database.
From 2011 to 2017, 18 patients aged 29 (25 - 31) years with a SAPS 3 of 84 (68 - 92) and main primary diagnosis of leptospirosis and influenza A (H1N1) virus were transported to three referral hospitals in São Paulo. A median distance of 39 (15 - 82) km was traveled on each rescue mission during a period of 360 (308 - 431) min. A median of one (0 - 2) nurse, three (2 - 3) physicians, and one (0 - 1) physical therapist was present per rescue. Seventeen rescues were made by ambulance, and one rescue was made by helicopter. The observed complications were interruption in the energy supply to the pump in two cases (11%) and oxygen saturation < 70% in two cases. Thirteen patients (72%) survived and were discharged from the hospital. Among the nonsurvivors, there were two cases of brain death, two cases of multiple organ dysfunction syndrome, and one case of irreversible pulmonary fibrosis.
Transportation with extracorporeal support occurred without serious complications, and the hospital survival rate was high.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):87-95
DOI 10.5935/0103-507X.20170013
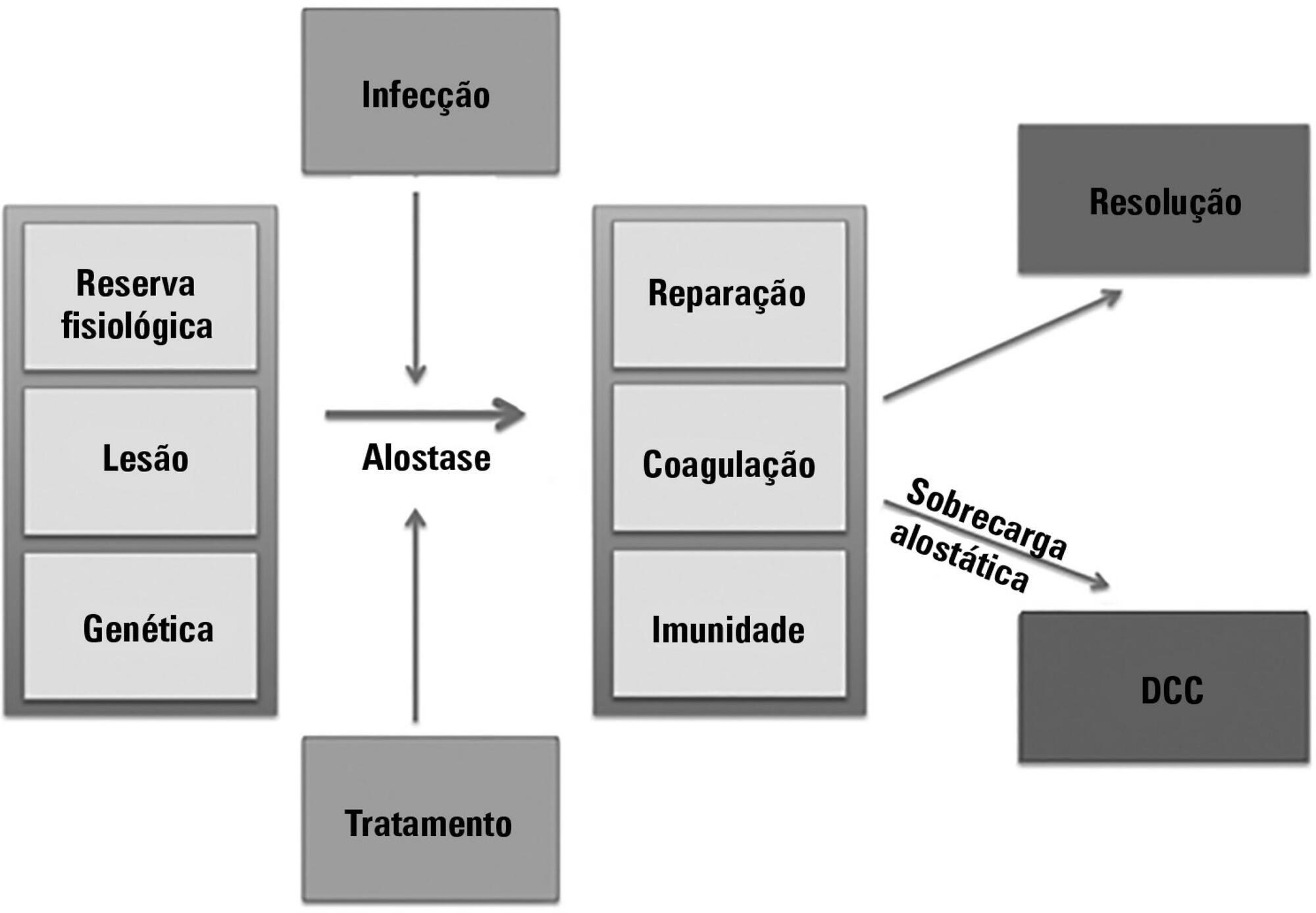
The technological advancements that allow support for organ dysfunction have led to an increase in survival rates for the most critically ill patients. Some of these patients survive the initial acute critical condition but continue to suffer from organ dysfunction and remain in an inflammatory state for long periods of time. This group of critically ill patients has been described since the 1980s and has had different diagnostic criteria over the years. These patients are known to have lengthy hospital stays, undergo significant alterations in muscle and bone metabolism, show immunodeficiency, consume substantial health resources, have reduced functional and cognitive capacity after discharge, create a sizable workload for caregivers, and present high long-term mortality rates. The aim of this review is to report on the most current evidence in terms of the definition, pathophysiology, clinical manifestations, treatment, and prognosis of persistent critical illness.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):436-443
DOI 10.5935/0103-507X.20170070
To define the frequency of cytomegalovirus disease among kidney transplant patients in an intensive care unit in which this complication was suspected and to identify predisposing factors and their possible impact on clinical outcome.
Retrospective observational study in which kidney transplant patients over the age of 18 years were hospitalized for any reason in an intensive care unit with at least one collection of samples to test for the presence of antigenemia or cytomegalovirus via polymerase chain reaction during hospitalization. Cytomegalovirus disease was defined as positive antigenemia or polymerase chain reaction above 500 copies/mL in the presence of symptoms and in the appropriate clinical setting, as judged by the attending physician.
A total of 99 patients were included (age: 53.4 ± 12.8 years, 71.6% male). Cytomegalovirus disease was diagnosed in 39 patients (39.4%). Respiratory symptoms (51%), non-specific clinical worsening (20%) or gastrointestinal symptoms (14%) were the main reasons for exam collection. Transplant time was lower in those with cytomegalovirus disease than in those without this diagnosis (6.5 months and 31.2 months, p = 0.001), along with pulse therapy in the last 6 months (41% and 16.9%, p = 0.008) and previous use of thymoglobulin in the last year (35.9% and 6.8%, p < 0.001). In the logistic regression model, only the transplant time and the use of thymoglobulin were associated with a higher frequency of cytomegalovirus. There was no difference in clinical evolution between patients with and without cytomegalovirus disease.
In kidney transplant patients suspected of cytomegalovirus disease, the prevalence was high. Transplant time less than 6 months, and the use of thymoglobulin in the last year should increase the intensivist's suspicion for this complication.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):247-251
DOI 10.5935/0103-507X.20150045
To evaluate the incidence of urinary tract infections due to Trichosporon spp. in an intensive care unit.
This descriptive observational study was conducted in an intensive care unit between 2007 and 2009. All consecutive patients admitted to the intensive care unit with a confirmed diagnosis were evaluated.
Twenty patients presented with urinary tract infections due to Trichosporon spp. The prevalence was higher among men (65%) and among individuals > 70 years of age (55%). The mortality rate was 20%. The average intensive care unit stay was 19.8 days. The onset of infection was associated with prior use of antibiotics and was more frequent in the fall and winter.
Infection due to Trichosporon spp. was more common in men and among those > 70 years of age and was associated with the use of an indwelling urinary catheter for more than 20 days and with the use of broadspectrum antibiotics for more than 14 days. In addition, patients with urinary infection due to Trichosporon spp. were most often hospitalized in intensive care units in the fall and winter periods.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):141-148
DOI 10.5935/0103-507X.20150025
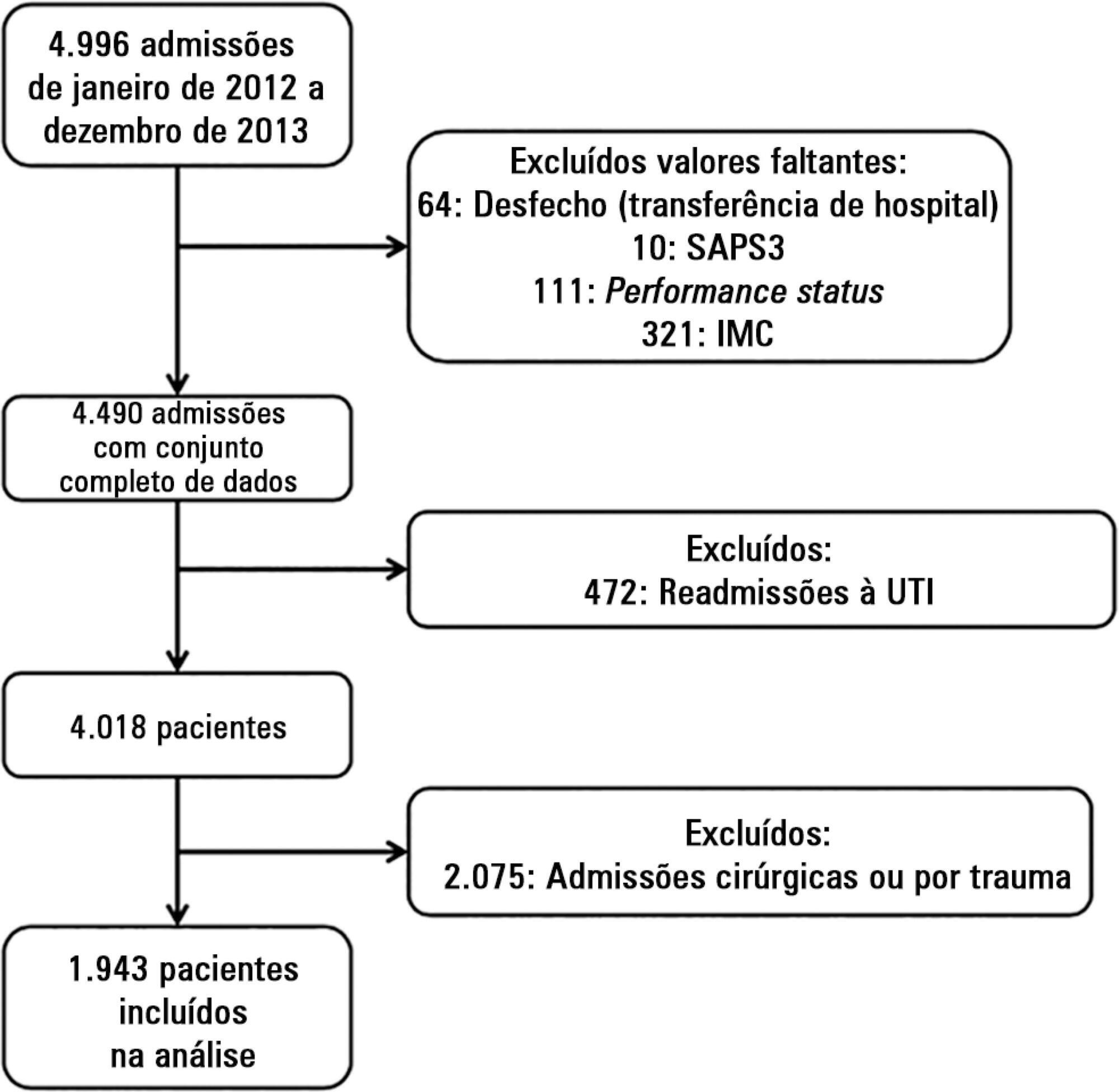
To evaluate the impact of body mass index on the short-term prognosis of non-surgical critically ill patients while controlling for performance status and comorbidities.
We performed a retrospective analysis on a two-year single-center database including 1943 patients. We evaluated the impact of body mass index on hospital mortality using a gradient-boosted model that also included comorbidities and was assessed by Charlson’s comorbidity index, performance status and illness severity, which was measured by the SAPS3 score. The SAPS3 score was adjusted to avoid including the same variable twice in the model. We also assessed the impact of body mass index on the length of stay in the hospital after intensive care unit admission using multiple linear regressions.
A low value (< 20kg/m2) was associated with a sharp increase in hospital mortality. Mortality tended to subsequently decrease as body mass index increased, but the impact of a high body mass index in defining mortality was low. Mortality increased as the burden of comorbidities increased and as the performance status decreased. Body mass index interacted with the impact of SAPS3 on patient outcome, but there was no significant interaction between body mass index, performance status and comorbidities. There was no apparent association between body mass index and the length of stay at the hospital after intensive care unit admission.
Body mass index does appear to influence the shortterm outcomes of critically ill medical patients, who are generally underweight. This association was independent of comorbidities and performance status.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):176-182
DOI 10.5935/0103-507X.20140026
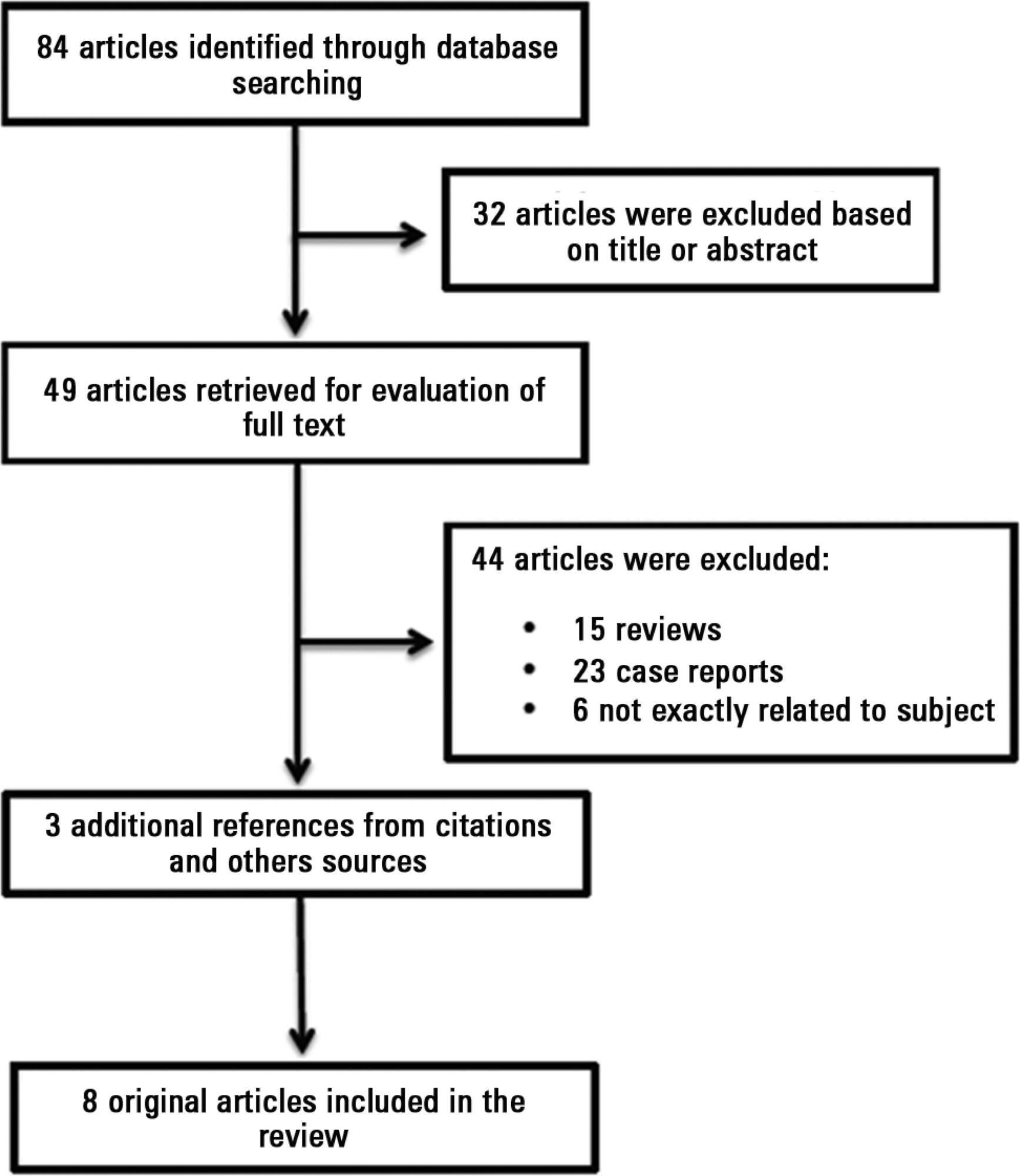
Antiphospholipid antibodies are responsible for a wide spectrum of clinical manifestations. Venous, arterial and microvascular thrombosis and severe catastrophic cases account for a large morbidly/mortality. Through the connection between the immune, inflammatory and hemostatic systems, it is possible that these antibodies may contribute to the development of organ dysfunction and are associated with poor short and long-term prognoses in critically ill patients. We performed a search of the PubMed/MedLine database for articles written during the period from January 2000 to February 2013 to evaluate the frequency of antiphospholipid antibodies in critically ill patients and their impact on the outcomes of these patients. Only eight original studies involving critically ill patients were found. However, the development of antiphospholipid antibodies in critically ill patients seems to be frequent, but more studies are necessary to clarify their pathogenic role and implications for clinical practice.