You searched for:"Heraldo Possolo de Souza"
We found (4) results for your search.-
Original Articles
sRAGE in septic shock: a potential biomarker of mortality
Rev Bras Ter Intensiva. 2014;26(4):392-396
Abstract
Original ArticlessRAGE in septic shock: a potential biomarker of mortality
Rev Bras Ter Intensiva. 2014;26(4):392-396
DOI 10.5935/0103-507X.20140060
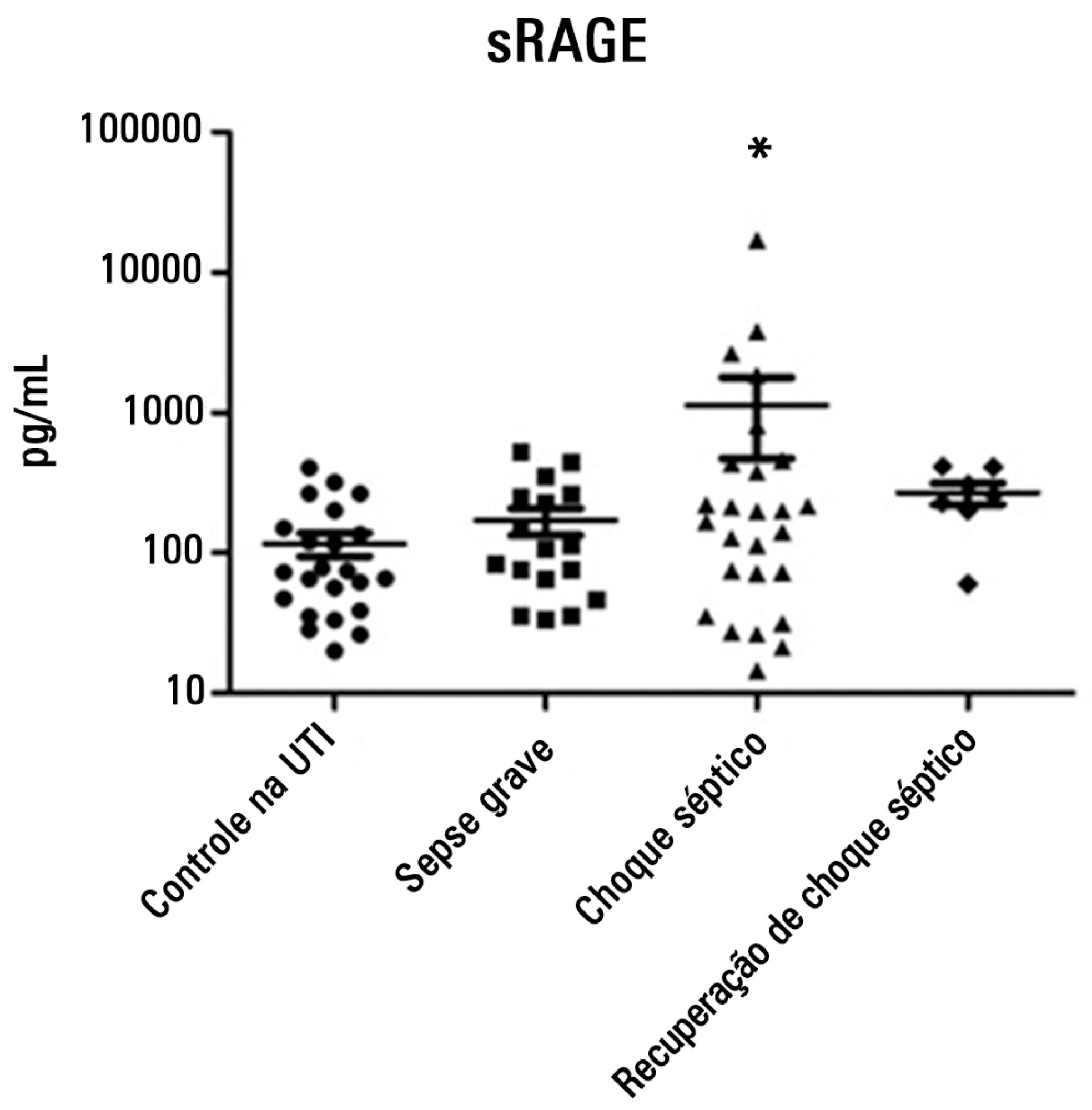
Views0See moreObjective:
To evaluate and understand the clinical implications of the plasma levels of a soluble isoform of a receptor for advanced glycation end products (sRAGE) in different stages of sepsis.
Methods:
Serum sRAGE values in patients who were divided into intensive care unit control, severe sepsis, septic shock and recovery from septic shock groups were statistically analyzed to assess quantity (Kruskal-Wallis), variability (Levine test) and correlation (Spearman rank test) with certain inflammatory mediators (IL-1 α, IL-6, IL-8, IL-10, IP-10, G-CSF, MCP-1, IFN-γ and TNF-α).
Results:
No changes in sRAGE levels were observed among the groups; however, the septic shock group showed differences in the variability of sRAGE compared to the other groups. A positive correlation with all the inflammatory mediators was reported in the septic shock group.
Conclusion:
sRAGE levels are associated with worse outcomes in patients with septic shock. However, a statistical correlation analysis with other proinflammatory cytokines indicated that the pathways leading to those outcomes are different depending on the sRAGE levels. Future studies to elucidate the pathophysiological mechanisms involving sRAGE in models of sepsis are of great clinical importance for the safe handling of this biomarker.
-
Original Article – Basic Research
Volume replacement with saline solutions during pancreatitis in rats and the hepatic profiles of apoptotic proteins and heat-shock proteins
Rev Bras Ter Intensiva. 2012;24(4):326-333
Abstract
Original Article – Basic ResearchVolume replacement with saline solutions during pancreatitis in rats and the hepatic profiles of apoptotic proteins and heat-shock proteins
Rev Bras Ter Intensiva. 2012;24(4):326-333
DOI 10.1590/S0103-507X2012000400006
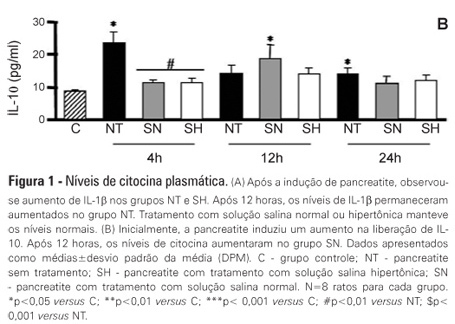
Views0See moreOBJECTIVE: Liver failure can occur as a consequence of the systemic inflammation after acute pancreatitis. We assessed the effect of volume repositioning with hypertonic saline solution or normal saline on hepatic cytokine production and the expression of heat-shock proteins and apoptotic proteins after acute pancreatitis. METHODS: Wistar rats were divided in four groups: C – control animals that were not subjected to insult or treatment; NT – animals that were subjected to acute pancreatitis and received no treatment; normal saline – animals that were subjected to acute pancreatitis and received normal saline (NaCl 0.9%); and HS – animals that were subjected to acute pancreatitis and received hypertonic saline solution (NaCl 7.5%). Acute pancreatitis was induced by retrograde transduodenal infusion of 2.5% sodium taurocholate into the pancreatic duct. At 4, 12 and 24 h following acute pancreatitis induction, TNF-alpha, IL-1-beta, IL-6 and IL-10, caspase-2 and -7, Apaf-1, AIF and HSP60 and 90 were analyzed in the liver. RESULTS: Casp2 decreased in the normal saline and hypertonic saline groups (p<0.05 versus. C) at 12 h. Apaf-1, AIF and HSP90 remained unchanged. At 4 h, Casp7 increased in the NT group (p<0.01 versus C), although it remained at the baseline levels in the reperfused groups. HSP60 increased in all of the groups at 4 h (p< 0.001 vs. C). However, the hypertonic saline group showed lower expression of HSP60 than the normal saline group (p<0.05). Hypertonic saline solution maintained the production of cytokines at normal levels. Volume reperfusion with normal or hypertonic saline significantly modulated the expression of Casp7. CONCLUSION: Volume replacement with hypertonic or normal saline was effective in reducing caspase 7. However, only hypertonic solution was capable of regulating cytokine production and HSP60 expression at all time points.
-
Original Articles
Anion gap corrected for albumin, phosphate and lactate is a good predictor of strong ion gap in critically ill patients: a nested cohort study
Rev Bras Ter Intensiva. 2013;25(3):205-211
Abstract
Original ArticlesAnion gap corrected for albumin, phosphate and lactate is a good predictor of strong ion gap in critically ill patients: a nested cohort study
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Views1OBJECTIVE:
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
METHODS:
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group – hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
RESULTS:
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
CONCLUSION:
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Keywords:Acid-base equilibrium/ physiologyBlood chemical analysisCritical illnessLactate/bloodPhosphate/ bloodPrognosisSerum albumin/bloodSee more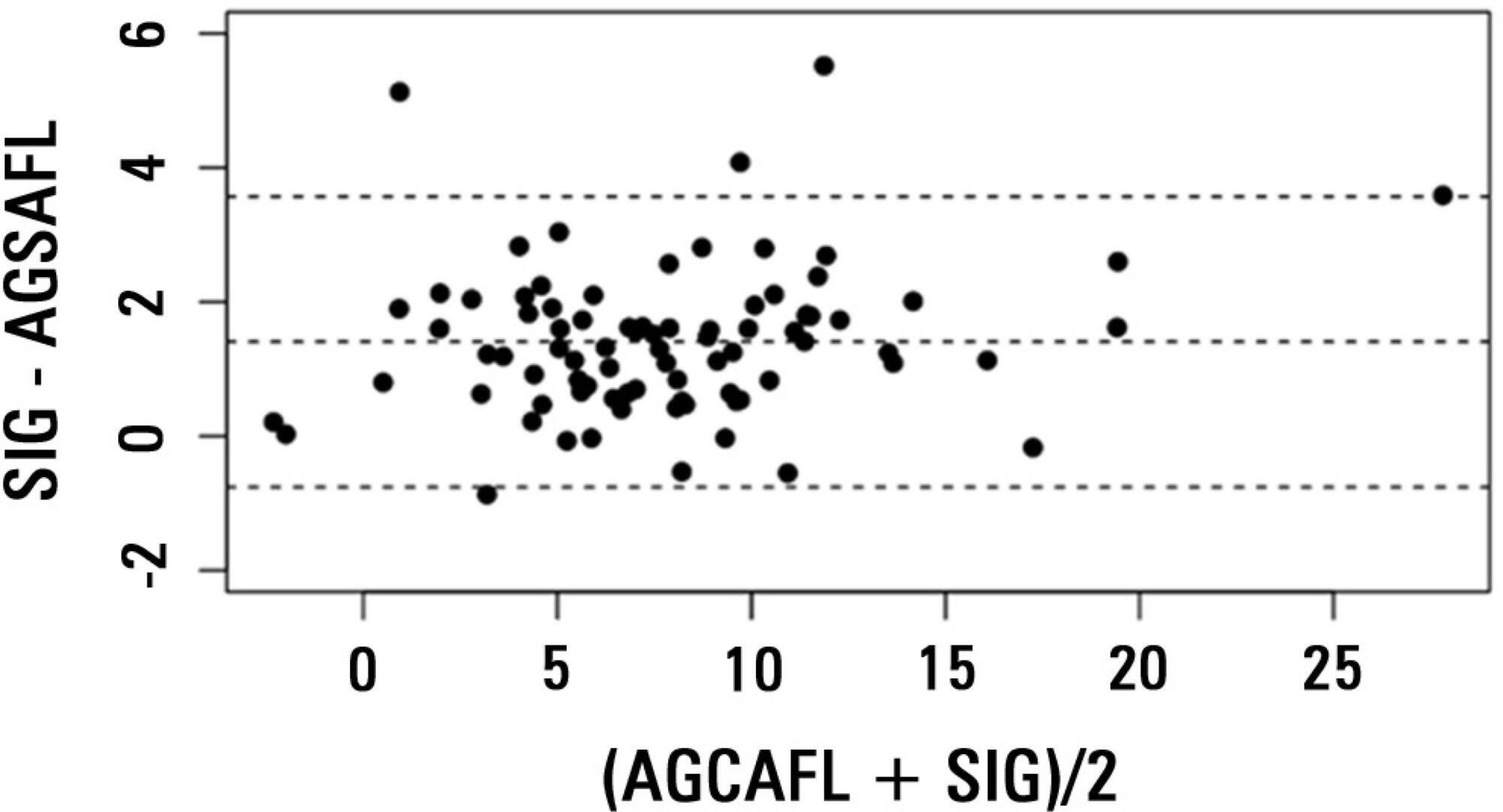
-
Original Articles
HLA-A*31 as a marker of genetic susceptibility to sepsis
Rev Bras Ter Intensiva. 2013;25(4):284-289
Abstract
Original ArticlesHLA-A*31 as a marker of genetic susceptibility to sepsis
Rev Bras Ter Intensiva. 2013;25(4):284-289
DOI 10.5935/0103-507X.20130049
Views0See moreObjective:
The HLA haplotype has been associated with many autoimmune diseases, but no associations have been described in sepsis. This study aims to investigate the HLA system as a possible marker of genetic sepsis susceptibility.
Methods:
This is a prospective cohort study including patients admitted to an intensive care unit and healthy controls from a list of renal transplant donors. Patients with less 18 years of age; pregnant or HIV positive patients; those with metastatic malignancies or receiving chemotherapy; or with advanced liver disease; or with end-of-life conditions were excluded. The DNA was extracted from the whole blood and HLA haplotypes determined using MiliPlex® technology.
Results:
From October 2010 to October 2012, 1,121 patients were included (1,078 kidney donors, 20 patients admitted with severe sepsis and 23 with septic shock). HLA-A*31 positive subjects had increased risk of developing sepsis (OR 2.36, 95%CI 1.26-5.35). Considering a p value <0.01, no other significant association was identified.
Conclusion:
HLA-A*31 expression is associated to risk of developing sepsis.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




