Abstract
Rev Bras Ter Intensiva. 2012;24(4):326-333
DOI 10.1590/S0103-507X2012000400006
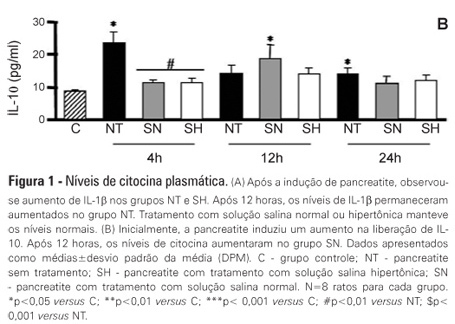
OBJECTIVE: Liver failure can occur as a consequence of the systemic inflammation after acute pancreatitis. We assessed the effect of volume repositioning with hypertonic saline solution or normal saline on hepatic cytokine production and the expression of heat-shock proteins and apoptotic proteins after acute pancreatitis. METHODS: Wistar rats were divided in four groups: C - control animals that were not subjected to insult or treatment; NT - animals that were subjected to acute pancreatitis and received no treatment; normal saline - animals that were subjected to acute pancreatitis and received normal saline (NaCl 0.9%); and HS - animals that were subjected to acute pancreatitis and received hypertonic saline solution (NaCl 7.5%). Acute pancreatitis was induced by retrograde transduodenal infusion of 2.5% sodium taurocholate into the pancreatic duct. At 4, 12 and 24 h following acute pancreatitis induction, TNF-alpha, IL-1-beta, IL-6 and IL-10, caspase-2 and -7, Apaf-1, AIF and HSP60 and 90 were analyzed in the liver. RESULTS: Casp2 decreased in the normal saline and hypertonic saline groups (p<0.05 versus. C) at 12 h. Apaf-1, AIF and HSP90 remained unchanged. At 4 h, Casp7 increased in the NT group (p<0.01 versus C), although it remained at the baseline levels in the reperfused groups. HSP60 increased in all of the groups at 4 h (p< 0.001 vs. C). However, the hypertonic saline group showed lower expression of HSP60 than the normal saline group (p<0.05). Hypertonic saline solution maintained the production of cytokines at normal levels. Volume reperfusion with normal or hypertonic saline significantly modulated the expression of Casp7. CONCLUSION: Volume replacement with hypertonic or normal saline was effective in reducing caspase 7. However, only hypertonic solution was capable of regulating cytokine production and HSP60 expression at all time points.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):302-307
DOI 10.1590/S0103-507X2012000300015
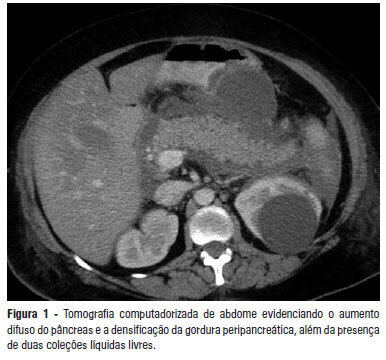
Acute pancreatitis is an inflammatory condition that is clinically manifested by abdominal pain and elevated serum levels of pancreatic enzymes. Hypertriglyceridemia is the third most common cause of acute pancreatitis. The present report aimed to describe a case of hypertriglyceridemia-induced acute pancreatitis, where the therapeutic approach was plasmapheresis. A 48-year-old female patient was admitted to the hospital with complaints of "severe abdominal pain". She reported the onset of such symptoms as nausea, vomiting and abdominal pain with a burning feeling in the epigastric area. The patient denied having a fever. The initial examination revealed that she was obese, oriented, tachypneic, normotensive, tachycardic, dehydrated, afebrile, anicteric and acyanotic and had normal color. Her abdomen was distended with bowel sounds, tympanic and diffusely painful, which was mostly in the supramesocolic compartment. The initial laboratory exams showed 10.932 mg/dL triglycerides, 1.548 mg/dL cholesterol, 226 mg/dL amylase and 899 mg/dL lipase. The abdominal computed tomography exhibited increased pancreatic volume (Balthazar E). The patient's condition worsened, and she was sent to the intensive care center. Plasmapheresis was performed with no complications. On the 14th day after admission, the patient was discharged from the intensive care center and was sent to the gastroenterology ward, where an oral diet was resumed with good acceptance. The patient progressed well and was discharged from the hospital on the 25th day after admission. High triglyceride levels are necessary to cause pancreatitis, and it is important to exclude the most common causes. Importantly, the therapeutic approach reduced the high hypertriglyceridemia quickly, thereby avoiding tissue damage.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):362-369
DOI 10.1590/S0103-507X2008000400008
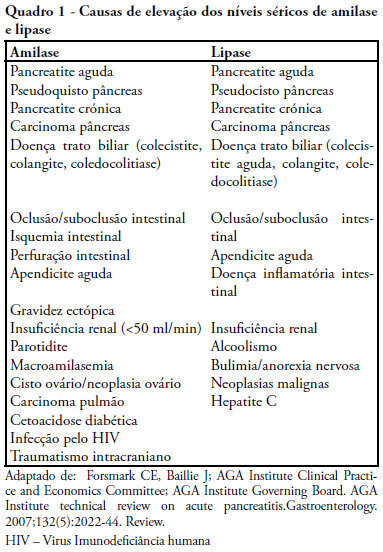
OBJECTIVES: Elevated lipase and amylase are commonly found in patients in intensive care unit without a previously recognized pancreatic illness, constituting a diagnostic and therapeutic challenge. The authors therefore proposed to determine the frequency of asymptomatic high serum lipase in critically ill patients, involved risk factors and outcome. METHODS: Retrospective study of patients admitted in an intensive care unit from January 1 to December 31, 2006, excluding admissions for acute pancreatitis, history of pancreatic disease, renal insufficiency or lacking of data. Patients were divided in two groups (with and without high serum lipase) that were compared for clinical, laboratory and radiological variables. Statistical analysis: SPSS 13; Student's t test and Chi-square test (CI 95%) with statistical significance if p< 0.05). RESULTS: 102 patients were included with high serum lipase was present in 39.2% of patients, mean lipase of 797U/L. Patients with high serum lipase had longer hospital stay (p< 0.001), parenteral nutrition (p< 0.001), ventilator support (p=0.04), fever (p< 0.001), hyperamylasemia (p<0.05), hyperbilirrubinemia (p=0.003) and rise of transaminases (p=0.001), with no significant differences in diagnosis, gender, age, APACHE II, SOFA, SAPS, mortality, hypotension, alkaline phosphatase, hemoglobin, lactate, tolerance to enteral nutrition and use of propofol. Imaging study revealed pancreatic alterations in two patients with high serum lipase. CONCLUSIONS: Elevated lipase was commonly found in critical patients, it related with longer length of stay but was not accompanied by increased clinical severity or mortality. It was more frequent with parenteral nutrition. A minority of patients met the criteria of acute pancreatitis.