You searched for:"Fernando Gutierrez"
We found (2) results for your search.-
Red blood cell transfusion in the intensive care setting: controversies amongst evidence
Rev Bras Ter Intensiva. 2009;21(3):315-323
Abstract
Red blood cell transfusion in the intensive care setting: controversies amongst evidence
Rev Bras Ter Intensiva. 2009;21(3):315-323
DOI 10.1590/S0103-507X2009000300013
Views0See moreAnemia is a prevalent issue in intensive care units. It appears in the first days, and may continue or worsen during hospital stay. Its etiology is generally multifactorial. Red blood cell transfusion is the most common intervention for treating anemia. Approximately 12 million blood units are used for transfusions in the United States, 25% to 30% in the intensive care units. Due to reduction of transfusion infections the increased safety has allowed an expansion of clinical indications. However, transfusion therapy is associated with other adverse effects such as nosocomial infections, immunological impairment, lung injury, hemolytic reactions and higher cancer incidence. Various papers have tried to show an association between correction of anemia and mortality-morbidity, but no consensus has been reached in literature. One of the current World Health Organization’s proposals is to reduce potentially unnecessary transfusions, promoting a rational transfusion attitude. The primary objective of this narrative review is to approach controversies regarding the transfusion threshold according to recent studies, and as a secondary objective, it aims to discuss iatrogenic anemia aspects and the different behaviors among intensivists on the best practices for implementation of transfusion practices. It is not within our objectives to discuss transfusion complications, although they are mentioned. A search was conducted on electronic literature databases (PubMed – Clinical Queries), and UpToDate 16.2, and additional consultation to textbooks. It became clear that transfusion practices are widely variable among intensive care units. Evidence is scarce that routine transfusion in non-hemorrhagic patients should be used in those with > 7 g/dL hemoglobin. There is no consensus on the transfusion threshold in critically ill patients. Cardiovascular disease patients seem to present a higher risk of death than non-cardiovascular patients, for any level of hemoglobin. Transfusion guided by hemoglobin levels and individual oxy-hemodynamic physiologic parameters and clinical context is apparently, the current best accepted strategy, rather than arbitrary and isolated hemoglobin correction.
-
Original Articles
Epidemiology and outcomes of non-cardiac surgical patients in Brazilian intensive care units
Rev Bras Ter Intensiva. 2008;20(4):376-384
Abstract
Original ArticlesEpidemiology and outcomes of non-cardiac surgical patients in Brazilian intensive care units
Rev Bras Ter Intensiva. 2008;20(4):376-384
DOI 10.1590/S0103-507X2008000400010
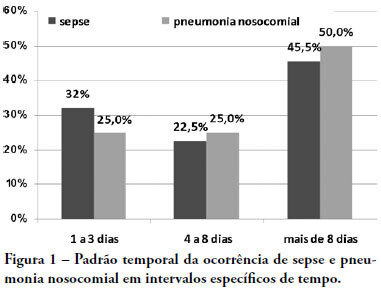
Views0See moreOBJECTIVES: Due to the dramatic medical breakthroughs and an increasingly ageing population, the proportion of patients who are at risk of dying following surgery is increasing over time. The aim of this study was to evaluate the outcomes and the epidemiology of non-cardiac surgical patients admitted to the intensive care unit. METHODS: A multicenter, prospective, observational, cohort study was carried out in 21 intensive care units. A total of 885 adult surgical patients admitted to a participating intensive care unit from April to June 2006 were evaluated and 587 patients were enrolled. Exclusion criteria were trauma, cardiac, neurological, gynecologic, obstetric and palliative surgeries. The main outcome measures were postoperative complications and intensive care unit and 90-day mortality rates. RESULTS: Major and urgent surgeries were performed in 66.4% and 31.7% of the patients, respectively. The intensive care unit mortality rate was 15%, and 38% of the patients had postoperative complications. The most common complication was infection or sepsis (24.7%). Myocardial ischemia was diagnosed in only 1.9% of the patients. A total of 94 % of the patients who died after surgery had co-morbidities at the time of surgery (3.4 ± 2.2). Multiple organ failure was the main cause of death (53%). CONCLUSION: Sepsis is the predominant cause of morbidity in patients undergoing non-cardiac surgery. In this patient population, multiple organ failure prevailed as the most frequent cause of death in the hospital.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




