Abstract
Rev Bras Ter Intensiva. 2021;33(4):557-564
DOI 10.5935/0103-507X.20210072
To describe health care providers’ knowledge about lung donation and donor lung management.
A descriptive, cross-sectional study based on an anonymous survey was conducted between March and September 2018 among health care professionals registered to Sociedad Argentina de Terapia Intensiva.
Of the 736 respondents, the mean age was 40.5 years (standard deviation 8.9), and 61.3% were female. Sixty percent were physicians, 21.5% were nurses, and 17.9% were physiotherapists. Seventy-eight percent considered themselves appropriately informed about organ procurement, and 79.8% stated that they knew potential organ donor critical care management. The lung donor criteria were answered correctly by 71.3% of the respondents. However, after the donor’s brain death, 51% made no changes to ventilator parameters, 22.9% were not aware of which parameters to reprogram, and 44.5% selected tidal volume of 6 - 8mL/kg and positive end expiratory pressure of 5cmH2O. For 85% of the health care providers, the type of apnea test chosen was disconnection from the ventilator, and only 18.5% used a lung management protocol. The most frequent interventions used in the case of arterial oxygen partial pressure/fractional inspired oxygen < 300 were positive end expiratory pressure titration, closed-circuit endotracheal suctioning, and recruitment maneuvers.
Health care professionals surveyed in Argentina correctly answered most of the questions related to lung donor criteria. However, they lacked detailed knowledge about ventilatory settings, ventilatory strategies, and protocols for lung donors. Educational programs are key to optimizing multiorgan donation and should be focused on protecting the donor lungs to increase the numbers of organs available for transplantation.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):571-577
DOI 10.5935/0103-507X.20200095
To describe the results from the implementation of a respiratory care and mechanical ventilation protocol on potential lung donors who met the conditions for procurement. The secondary objective is to compare the results with historical data.
This was a retrospective, observational study. It included potential donors suitable for procurement of organs who had brain death and were hospitalized in critical care units of the Autonomous City of Buenos Aires from April 2017 to March 2018. Main variables: number of potential lung donors that reached the objective of procurement, rate of lungs procured, and rate of implanted lungs. Values of p < 0.05 were considered significant.
Thirty potential lung donors were included, and 23 (88.5%; 95%CI 69.8 - 97.6) met the oxygenation objective. Twenty potential lung donors donated organs, of whom eight donated lungs, with which four double lung transplants and eight single lung transplants were performed. Seven of 12 lungs were procured and implanted in the preprotocol period, while all 12 were under the protocol (p = 0.38). The implantation rate was 58.3% (7/12) in the historical control period and 100% (12/12) (p = 0.04) in the study period.

Abstract
Rev Bras Ter Intensiva. 2020;32(3):405-411
DOI 10.5935/0103-507X.20200069
We investigated the frequency of apnea tests, and the use of ancillary tests in the diagnosis of brain death in our hospital, as well as the reasons for not being able to perform apnea testing and the reasons for using ancillary tests.
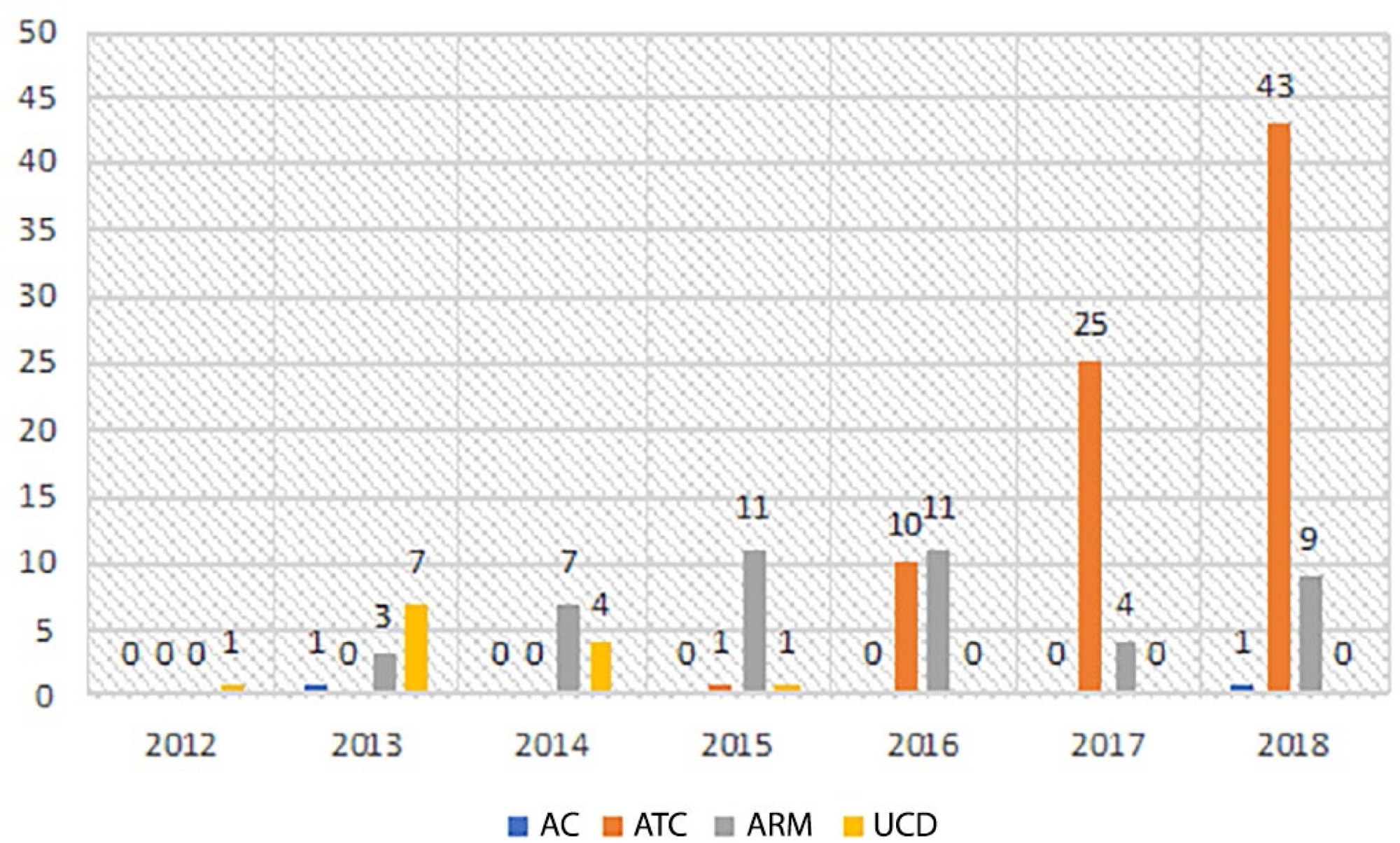
In this retrospective study, the files of patients diagnosed with brain death between 2012 - 2018 were examined. The preferred test was determined if an ancillary test was performed in the diagnosis of brain death. The rate and frequency of use of these tests were analyzed.
During the diagnosis of brain death, an apnea test was performed on 104 (61.5%) patients and was not or could not be performed on 65 (38.5%) patients. Ancillary tests were performed on 139 (82.8%) of the patients. The most common ancillary test was computed tomography angiography (79 patients, 46.7%). Approval for organ donation was received in the meetings with the family following the diagnosis of brain death for 55 (32.5%) of the 169 patients.
We found an increase in the rate of incomplete apnea tests and concordantly, an increase in the use of ancillary tests in recent years. Ancillary tests should be performed on patients when there is difficulty in reaching a decision of brain death, but it should not be forgotten that there is no worldwide consensus on the use of ancillary tests.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):303-311
DOI 10.5935/0103-507X.20190055
To evaluate the medical knowledge regarding the application of the diagnostic criteria for brain death and to correlate it with training parameters for this diagnosis according to Federal Council of Medicine resolution 2,173 of 2017.
We interviewed 174 physicians with experience with comatose patients. A structured questionnaire adapted from previous studies was used. The associations of the variables were tested using the chi-square test for independence. A multivariate logistic model was fitted for associations with p values ≤ 0.20.
Among the interviewees, 40% had been working for more than 1 year in intensive care, and 23% had initiated ten or more brain death protocols complying with the new resolution. Forty-five percent of the interviewees reported having difficulty following the criteria, 94% acknowledged the need for complementary tests for diagnosis, and 8% of them reported the existence of incorrect tests. The difficulty with these criteria decreased with an increase in the number of years of medical training (OR = 0.487; p = 0.045; 95%CI 0.241 - 0.983) and with a higher number of initiated brain death protocols (OR = 0.223; p = 0.0001; 95%CI 0.117 - 0.424).
Difficulties in the application of brain death criteria were identified by a significant portion of the sample. However, among other factors, more years of training and a greater number of initiated brain death protocols were associated with greater ease in the application of brain death criteria according to the guidelines provided in Resolution 2,173 of the Federal Council of Medicine.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):285-293
DOI 10.5935/0103-507X.20160043
To evaluate the knowledge and acceptance of the public and professionals working in intensive care units regarding organ donation after cardiac death.
The three hospitals with the most brain death notifications in Curitiba were selected, and two groups of respondents were established for application of the same questionnaire: the general public (i.e., visitors of patients in intensive care units) and health professionals working in the same intensive care unit. The questionnaire contained questions concerning demographics, intention to donate organs and knowledge of current legislation regarding brain death and donation after cardiac death.
In total, 543 questionnaires were collected, including 442 from family members and 101 from health professionals. There was a predominance of women and Catholics in both groups. More females intended to donate. Health professionals performed better in the knowledge comparison. The intention to donate organs was significantly higher in the health professionals group (p = 0.01). There was no significant difference in the intention to donate in terms of education level or income. There was a greater acceptance of donation after uncontrolled cardiac death among Catholics than among evangelicals (p < 0.001).
Most of the general population intended to donate, with greater intentions expressed by females. Education and income did not affect the decision. The type of transplant that used a donation after uncontrolled cardiac death was not well accepted in the study population, indicating the need for more clarification for its use in our setting.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):279-283
DOI 10.5935/0103-507X.20130048
To evaluate the level of knowledge of medical students about transplantation and brain death.
An anonymous self-administered questionnaire answered by medical students from the first through the sixth year that was based on information from the Associação Brasileira de Transplante de Órgãos e Tecidos, the Registro Brasileiro de Transplantes and the resolution that defines the criteria for brain death.
Of the 677 medical students asked, 310 (45.8%) agreed to answer the questionnaire. In total, 22 (7.0%) subjects were excluded. Of the students who participated, 41.3% reported having already attended a class on organ transplantation and 33% on brain death; 9.7% felt able to diagnose brain death (p<0.01); only 66.8% indicated the kidney as the most transplanted solid organ in Brazil.
The level of knowledge of medical students at this institution regarding brain death and transplantation is limited, which may be the result of an inadequate approach during medical school.