Abstract
Rev Bras Ter Intensiva. 2020;32(3):348-353
DOI 10.5935/0103-507X.20200062
A novel coronavirus emerged this year as a cause of viral pneumonia. The main characteristics of the virus are rapid transmission, high contagion capacity and potential severity. The objective of this case series study is to describe the clinical characteristics of patients with confirmed coronavirus disease (COVID-19) admitted to different intensive care units in Argentina for mechanical ventilation.
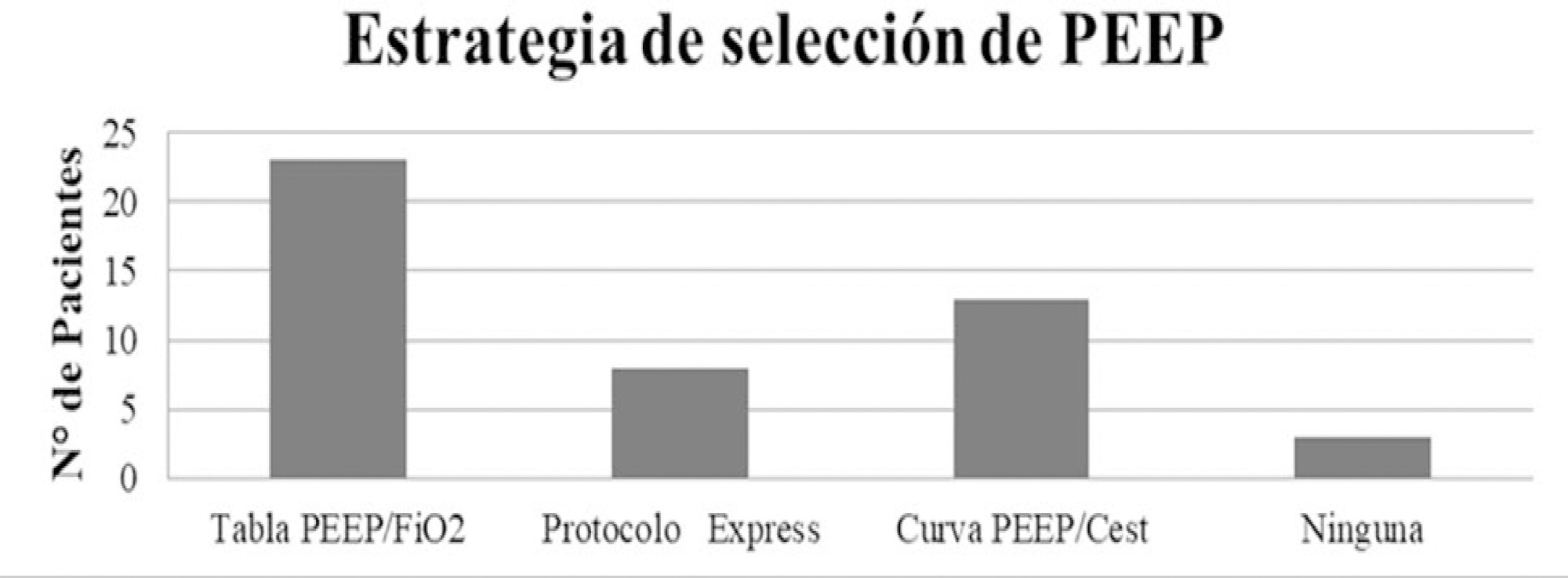
A descriptive, prospective, multicenter case series study was conducted between April 1 and May 8, 2020. Data from patients older than 18 years who were admitted to the intensive care unit for mechanical ventilation for acute respiratory failure with a positive diagnosis of COVID-19 were included.
The variables for 47 patients from 31 intensive care units were recorded: 78.7% were men (median age of 61 years), with a SAPS II score of 43 and a Charlson index score of 3. The initial ventilatory mode was volume control - continuous mandatory ventilation with a tidal volume less than 8mL/kg in 100% of cases, with a median positive end-expiratory pressure of 10.5cmH2O. At the end of the study, 29 patients died, 8 were discharged, and 10 remained hospitalized. The SAPS II score was higher among patients who died (p = 0.046). Charlson comorbidity index was associated with higher mortality (OR = 2.27, 95% CI 1.13 - 4.55, p = 0.02).
Patients with COVID-19 and on mechanical ventilation in this series presented clinical variables similar to those described to date in other international reports. Our findings provide data that may predict outcomes.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):354-362
DOI 10.5935/0103-507X.20200063
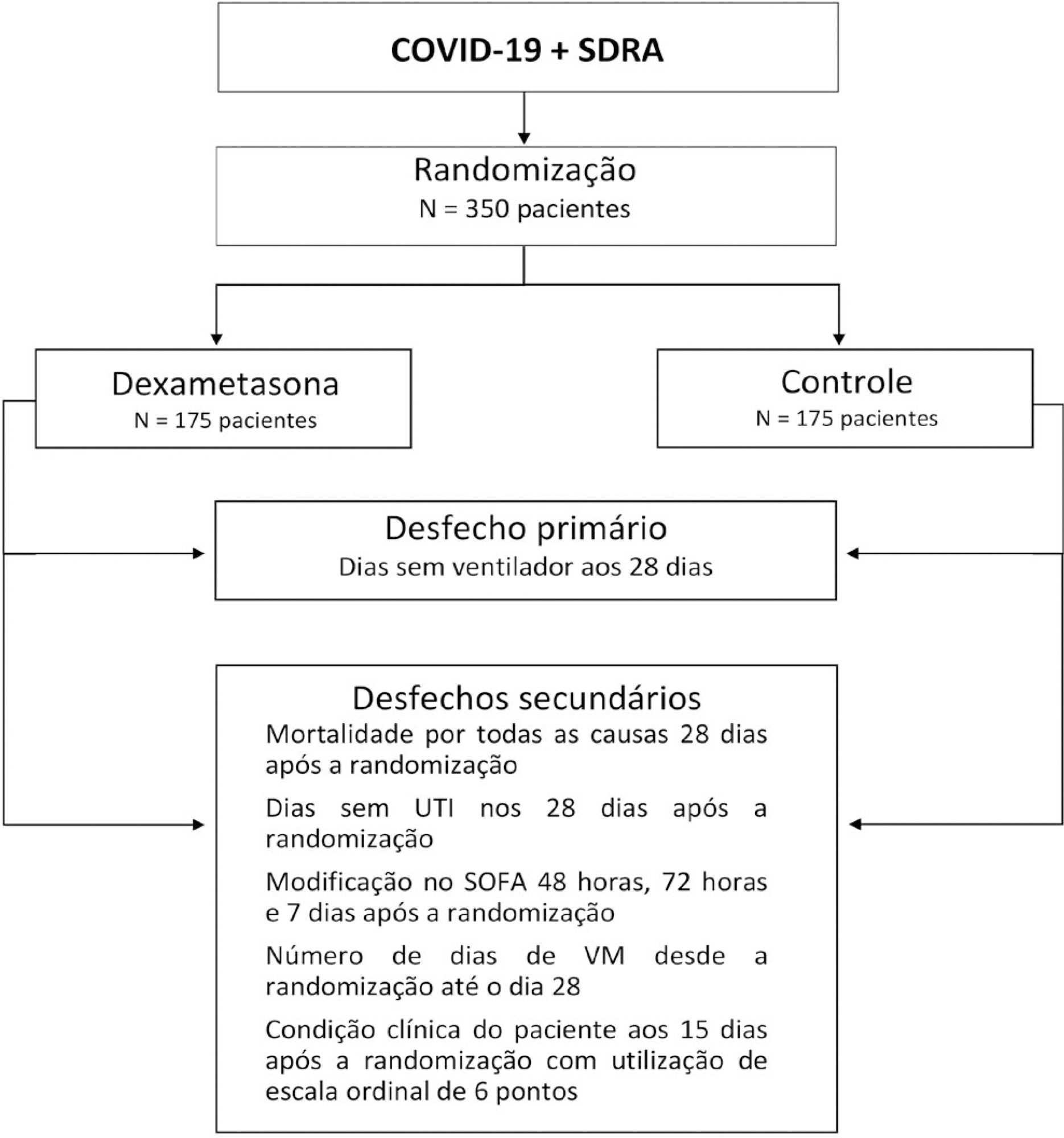
The infection caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads worldwide and is considered a pandemic. The most common manifestation of SARS-CoV-2 infection (coronavirus disease 2019 - COVID-19) is viral pneumonia with varying degrees of respiratory compromise and up to 40% of hospitalized patients might develop acute respiratory distress syndrome. Several clinical trials evaluated the role of corticosteroids in non-COVID-19 acute respiratory distress syndrome with conflicting results. We designed a trial to evaluate the effectiveness of early intravenous dexamethasone administration on the number of days alive and free of mechanical ventilation within 28 days after randomization in adult patients with moderate or severe acute respiratory distress syndrome due to confirmed or probable COVID-19.
This is a pragmatic, prospective, randomized, stratified, multicenter, open-label, controlled trial including 350 patients with early-onset (less than 48 hours before randomization) moderate or severe acute respiratory distress syndrome, defined by the Berlin criteria, due to COVID-19. Eligible patients will be randomly allocated to either standard treatment plus dexamethasone (Intervention Group) or standard treatment without dexamethasone (Control Group). Patients in the intervention group will receive dexamethasone 20mg intravenous once daily for 5 days, followed by dexamethasone 10mg IV once daily for additional 5 days or until intensive care unit discharge, whichever occurs first. The primary outcome is ventilator-free days within 28 days after randomization, defined as days alive and free from invasive mechanical ventilation. Secondary outcomes are all-cause mortality rates at day 28, evaluation of the clinical status at day 15 assessed with a 6-level ordinal scale, mechanical ventilation duration from randomization to day 28, Sequential Organ Failure Assessment Score evaluation at 48 hours, 72 hours and 7 days and intensive care unit -free days within 28.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):251-260
DOI 10.5935/0103-507X.20200036
To assess the prevalence of and factors associated with Burnout syndrome among intensive care unit professionals.
In this cross-sectional population-based study, a questionnaire assessing sociodemographic, behavioral, and occupational data was administered to 241 nurses and physicians working in 17 public intensive care units in São Luis (MA), Brazil. The Maslach Burnout Inventory - Human Services Survey was used to identify Burnout syndrome based on Maslach’s and Grunfeld’s criteria. The prevalence of each dimension of the syndrome was estimated with a 95% confidence interval. Associations were estimated by the odds ratios via multiple logistic regression analyses (α = 5%).
The prevalence of Burnout syndrome was 0.41% (0.01 - 2.29) according to Maslach’s criteria and 36.9% (30.82 - 43.36) according to Grunfeld’s criteria. Infant intensive care unit professionals were more likely to develop emotional exhaustion than other intensive care professionals (OR = 3.16). Respondents over the age of 35 were less likely to develop emotional exhaustion (OR = 0.32) and depersonalization (OR = 0.06). Longer working hours in intensive care units were associated with a reduced sense of personal accomplishment (OR = 1.13). Among nurses, males had a lower sense of professional accomplishment, and not exercising regularly was associated with more emotional exhaustion and less depersonalization. Among physicians, working in infant and cardiology intensive care units made them less likely to have a reduced sense of personal accomplishment, and physicians without a postgraduate degree who worked in intensive care units had a higher chance of having a lower sense of personal accomplishment.
This study demonstrated the low prevalence of Burnout syndrome. Most of the professionals reported low levels for each dimension of Burnout, including low levels of emotional exhaustion, low levels of depersonalization, and a lower likelihood of having a reduced sense of personal accomplishment. Nurses and physicians have different characteristics associated with Burnout syndrome.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):301-307
DOI 10.5935/0103-507X.20200047
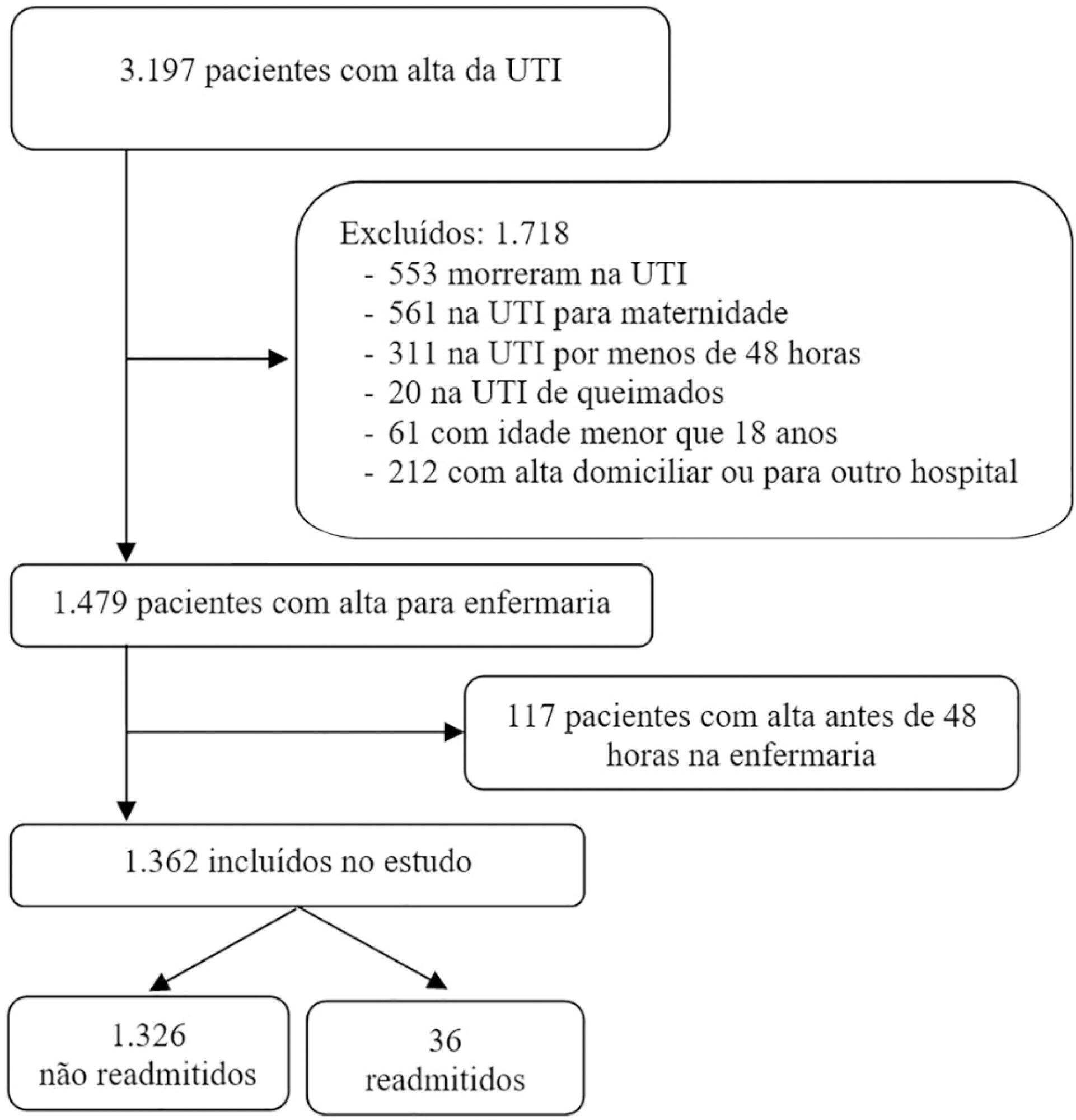
To evaluate the hypothesis that the Modified Early Warning Score (MEWS) at the time of intensive care unit discharge is associated with readmission and to identify the MEWS that most reliably predicts intensive care unit readmission within 48 hours of discharge.
This was a retrospective observational study of the MEWSs of discharged patients from the intensive care unit. We compared the demographics, severity scores, critical illness characteristics, and MEWSs of readmitted and non-readmitted patients, identified factors associated with readmission in a logistic regression model, constructed a Receiver Operating Characteristic (ROC) curve of the MEWS in predicting the probability of readmission, and presented the optimum criterion with the highest sensitivity and specificity.
The readmission rate was 2.6%, and the MEWS was a significant predictor of readmission, along with intensive care unit length of stay > 10 days and tracheostomy. The ROC curve of the MEWS in predicting the readmission probability had an AUC of 0.82, and a MEWS > 6 carried a sensitivity of 0.78 (95%CI 0.66 - 0.9) and specificity of 0.9 (95%CI 0.87 - 0.93).
The MEWS is associated with intensive care unit readmission, and a score > 6 has excellent accuracy as a prognostic predictor.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):229-234
DOI 10.5935/0103-507X.20200041
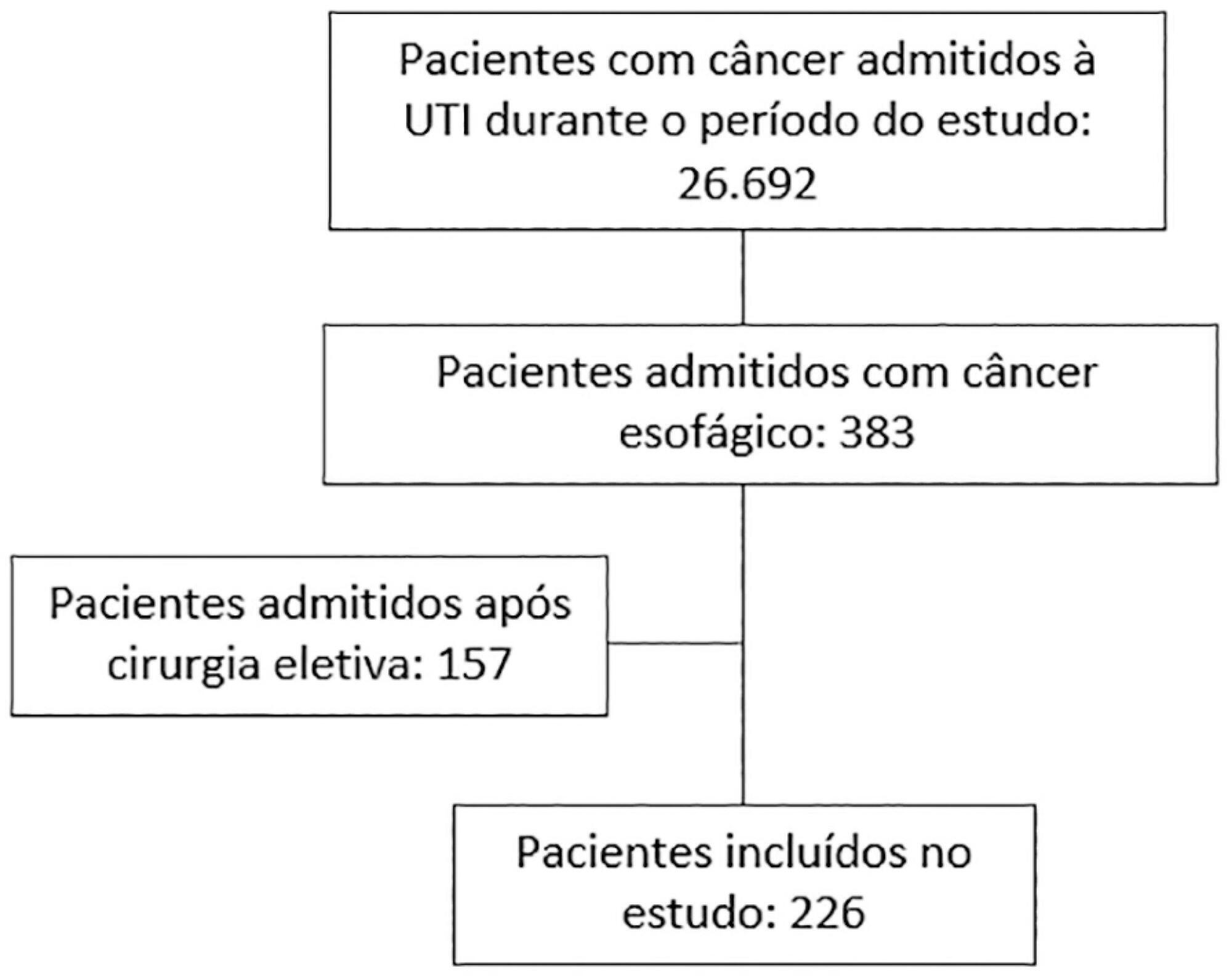
To depict the clinical presentation and outcomes of a cohort of critically ill patients with esophageal cancer.
We carried out a multicenter retrospective study that included patients with esophageal cancer admitted to intensive care units with acute illness between September 2009 and December 2017. We collected the demographic and clinical characteristics of all included patients, as well as organ-support measures and hospital outcomes. We performed logistic regression analysis to identify independent factors associated with in-hospital mortality.
Of 226 patients included in the study, 131 (58.0%) patients died before hospital discharge. Squamous cell carcinoma was more frequent than adenocarcinoma, and 124 (54.9%) patients had metastatic cancer. The main reasons for admission were sepsis/septic shock and acute respiratory failure. Mechanical ventilation (OR = 6.18; 95%CI 2.86 - 13.35) and metastatic disease (OR = 7.10; 95%CI 3.35 - 15.05) were independently associated with in-hospital mortality.
In this cohort of patients with esophageal cancer admitted to intensive care units with acute illness, the in-hospital mortality rate was very high. The requirement for invasive mechanical ventilation and metastatic disease were independent prognostic factors and should be considered in discussions about the short-term outcomes of these patients.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):37-42
DOI 10.5935/0103-507X.20200007
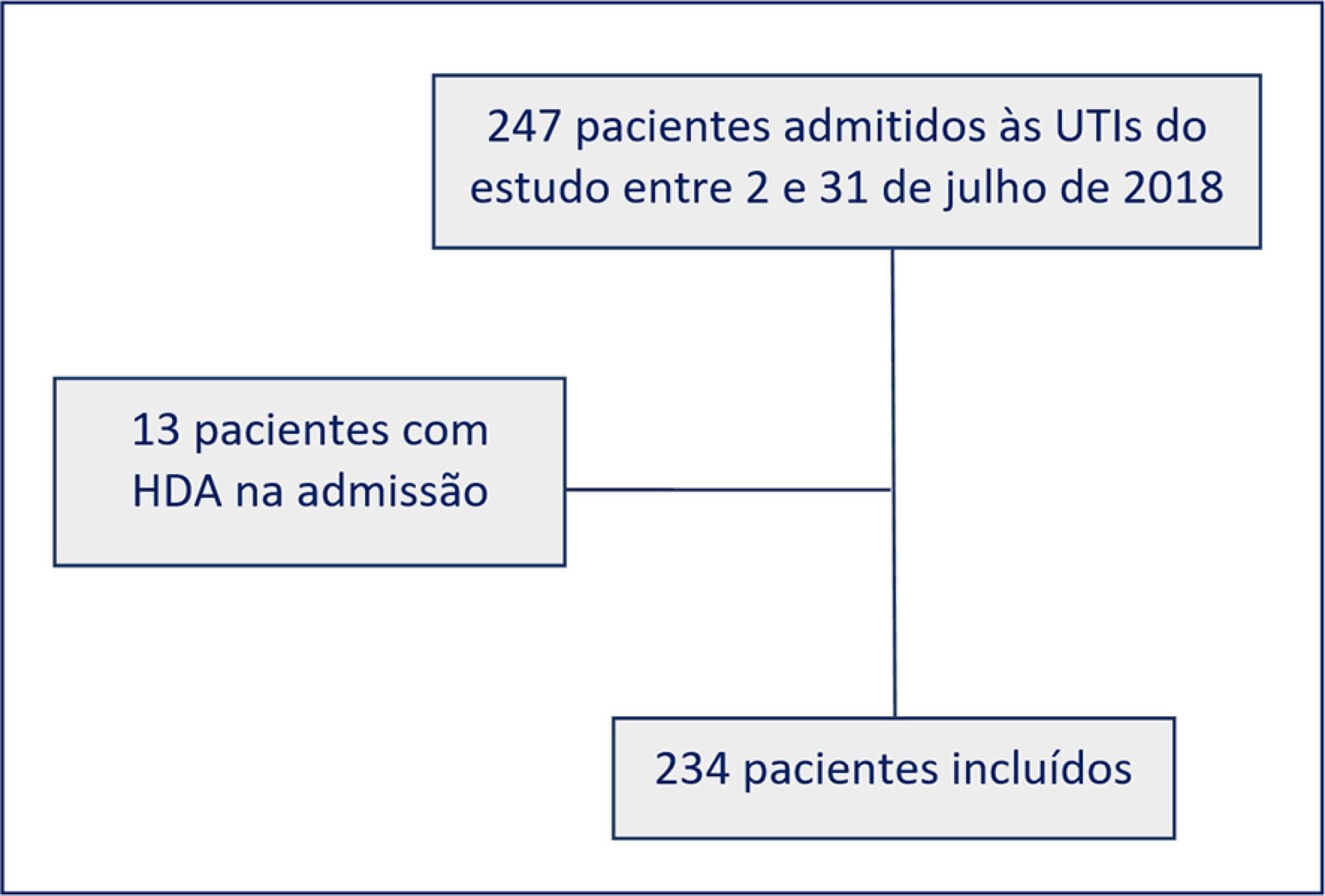
To evaluate adherence to the stress ulcer prophylaxis protocol in critically ill patients at a tertiary university hospital.
In this prospective cohort study, we included all adult patients admitted to the medical and surgical intensive care units of an academic tertiary hospital. Our sole exclusion criterion was upper gastrointestinal bleeding at intensive care unit admission. We collected baseline variables and stress ulcer prophylaxis indications according to the institutional protocol and use of prophylaxis. Our primary outcome was adherence to the stress ulcer prophylaxis protocol. Secondary outcomes were appropriate use of stress ulcer prophylaxis, upper gastrointestinal bleeding incidence and factors associated with appropriate use of stress ulcer prophylaxis.
Two hundred thirty-four patients were enrolled from July 2nd through July 31st, 2018. Patients were 52 ± 20 years old, 125 (53%) were surgical patients, and the mean SAPS 3 was 52 ± 20. In the longitudinal follow-up, 1499 patient-days were studied; 1069 patient-days had stress ulcer prophylaxis indications, and 777 patient-days contained prophylaxis use (73% stress ulcer prophylaxis protocol adherence). Of the 430 patient-days without stress ulcer prophylaxis indications, 242 involved prophylaxis (56% inappropriate stress ulcer prophylaxis use). The overall appropriate use of stress ulcer prophylaxis was 64%. Factors associated with proper stress ulcer prophylaxis prescription were mechanical ventilation OR 2.13 (95%CI 1.64 - 2.75) and coagulopathy OR 2.77 (95%CI 1.66 - 4.60). The upper gastrointestinal bleeding incidence was 12.8%.
Adherence to the stress ulcer prophylaxis protocol was low and inappropriate use of stress ulcer prophylaxis was frequent in this cohort of critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):92-98
DOI 10.5935/0103-507X.20200014
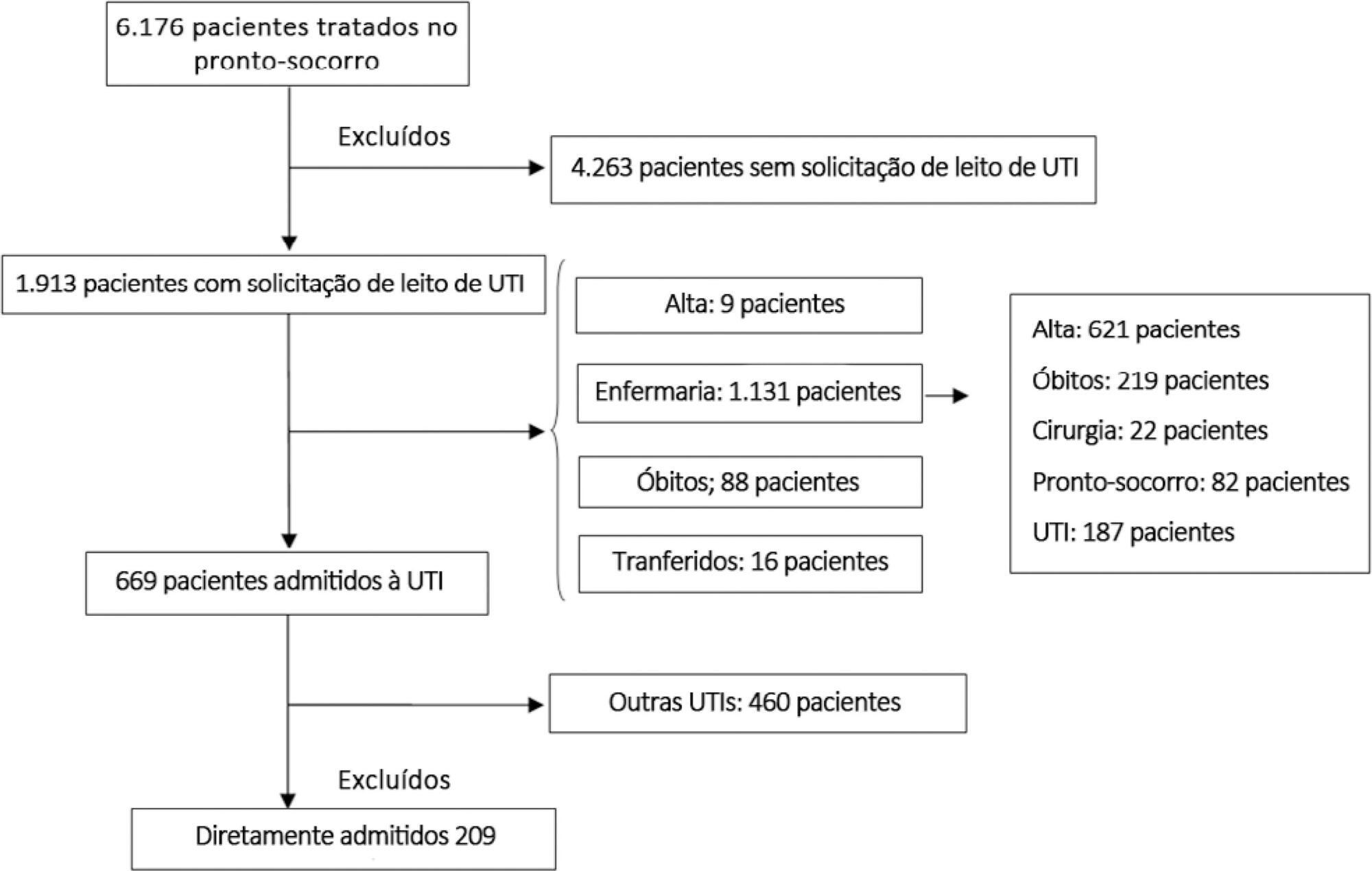
To examine the impact of delayed transfer from the emergency room into the intensive care unit on the length of intensive care unit stay and death.
This prospective, cohort study performed in a tertiary academic hospital obtained data from 1913 patients admitted to the emergency room with a documented request for admission into the intensive care unit. The patients admitted directly into the medical-surgical intensive care unit (n = 209) were categorized into tertiles according to their waiting time for intensive care unit admission (Group 1: < 637 min, Group 2: 637 to 1602 min, and Group 3: > 1602 min). Patients who stayed in the intensive care unit for longer than 3.2 days (median time of intensive care unit length of stay of all patients) were considered as having a prolonged intensive care unit stay.
A total of 6,176 patients were treated in the emergency room during the study period, among whom 1,913 (31%) required a bed in the intensive care unit. The median length of stay in the emergency room was 17 hours [9 to 33 hours]. Hospitalization for infection/sepsis was an independent predictor of prolonged intensive care unit stay (OR 2.75 95%CI 1.38 - 5.48, p = 0.004), but waiting time for intensive care unit admission was not. The mortality rate was higher in Group 3 (38%) than in Group 1 (31%) but the difference was not statistically significant.
Delayed admission into the intensive care unit from the emergency room did not result in an increased intensive care unit stay or mortality.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):571-581
DOI 10.5935/0103-507X.20190070
Descrever a adequação de duas escalas comportamentais, a Behavioral Pain Scale e a Critical Care Pain Observation Tool, para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidades de terapia intensiva.
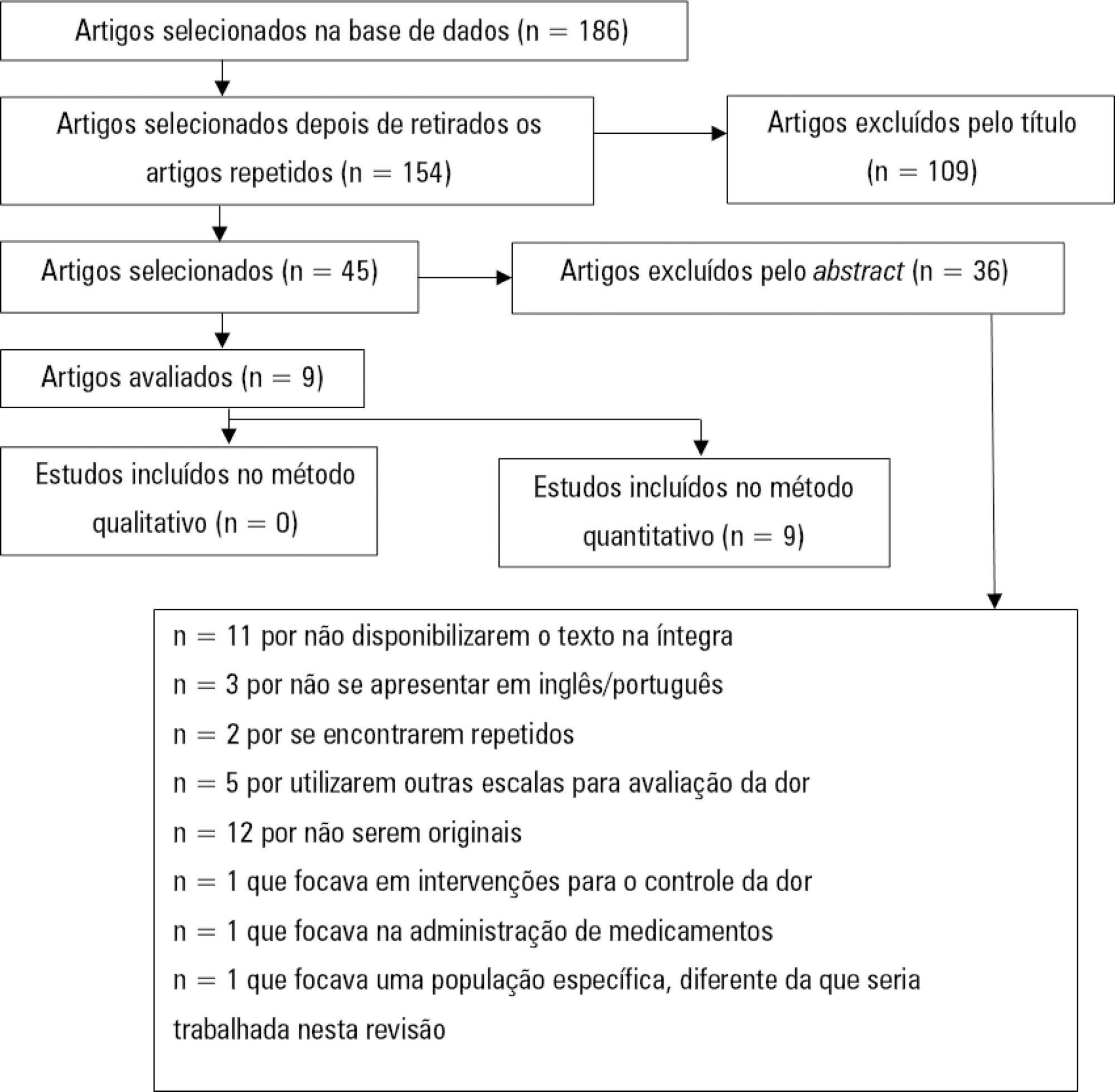
Utilizando a metodologia recomendada pelo Centro Cochrane, foi realizada revisão sistemática da literatura, na base de dados eletrônica EBSCO host (CINAHL Complete, MEDLINE®Complete, Nursing & Allied Health Collection: Comprehensive, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Library, Information Science & Technology Abstracts, MedicLatina). Foram realizadas duas pesquisas com os seguintes termos em inglês no campo de pesquisa: "behavioral pain scale" AND "critical care pain observation tool" AND "behavioral pain scale" OR "critical care pain observation tool". Dois revisores independentes realizaram a avaliação crítica, a extração e a síntese dos dados.
Foram incluídos 15 estudos que evidenciaram que a Behavioral Pain Scale e a Critical Care Pain Observation Tool eram duas escalas válidas e confiáveis para a avaliação da dor em pacientes intubados orotraquealmente e internados em unidade de terapia intensiva. As escalas apresentaram propriedades psicométricas semelhantes, bem como boa confiabilidade.
Ambas as escalas são adequadas para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidade de terapia intensiva, contudo, apresentam limitações em populações específicas como doentes vítimas de trauma, queimados e do foro neurocirurgico. É sugerida a realização de mais estudos sobre o tema e em populações específicas.