Abstract
Rev Bras Ter Intensiva. 2017;29(2):222-230
DOI 10.5935/0103-507X.20170031
Some patients admitted to an intensive care unit may face a terminal illness situation, which usually leads to death. Knowledge of palliative care is strongly recommended for the health care providers who are taking care of these patients. In many situations, the patients should be evaluated daily as the introduction of further treatments may not be beneficial to them. The discussions among health team members that are related to prognosis and the goals of care should be carefully evaluated in collaboration with the patients and their families. The adoption of protocols related to end-of-life patients in the intensive care unit is fundamental. A multidisciplinary team is important for determining whether the withdrawal or withholding of advanced care is required. In addition, patients and families should be informed that palliative care involves the best possible care for that specific situation, as well as respect for their wishes and the consideration of social and spiritual backgrounds. Thus, the aim of this review is to present palliative care as a reasonable option to support the intensive care unit team in assisting terminally ill patients. Updates regarding diet, mechanical ventilation, and dialysis in these patients will be presented. Additionally, the hospice-model philosophy as an alternative to the intensive care unit/hospital environment will be discussed.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):197-206
DOI 10.1590/S0103-507X2012000200017
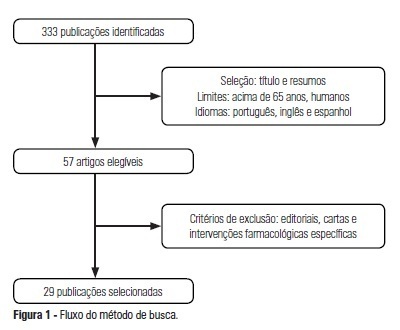
OBJECTIVE: The use of interventionist medical technology in terminal elderly patients must be associated with palliative care as a measure of clinical support in intensive care units. Palliative care is an important component of end-of-life care, and the assistance provided by the healthcare team should be guided by decisions made by patients and their family members. Prolongation of life not accompanied by therapies aimed at relieving symptoms, such as pain and dyspnea, contributes to patient and family member stress suffering. The aim of the present study was to survey advances made in the application of palliative care in intensive care units. METHODS: Medline and Bireme were used to perform a systematic literature review of intensive care units-based palliative care for elderly patients. RESULTS: A total of 29 articles describing palliative care in intensive care units were analyzed according to the variables "satisfaction of relatives when they participate in the discussions on palliative care" and "difficulties to implement such type of care due to lack of technical skills of the health caregivers." CONCLUSION: Palliative care for elderly patients in intensive care units must be more thoroughly investigated to improve the relationships and communication among patients, their relatives, and the healthcare team. As greater numbers of elderly patients are admitted to intensive care units, the skills of health caregivers must improve to meet the challenges posed by the end-of-life care.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):24-29
DOI 10.1590/S0103-507X2011000100005
Palliative care is aimed to improve the quality of life of both patients and their family members during the course of life-threatening diseases through the prevention, early identification and treatment of the symptoms of physical, psychological, spiritual and social suffering. Palliative care should be provided to every critically ill patient; this requirement renders the training of intensive care practitioners and education initiatives fundamental. Continuing the Technical Council on End of Life and Palliative Care of the Brazilian Association of Intensive Medicine activities and considering previously established concepts, the II Forum of the End of Life Study Group of the Southern Cone of America was conducted in October 2010. The forum aimed to develop palliative care recommendations for critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):141-147
DOI 10.1590/S0103-507X2009000200005
OBJECTIVES: To evaluate the medical decisions at end-of-life of patients admitted at HU/UFSC and to compare these decisions and the profile of patients who died in the intensive care unit (ICU) to those who died in medical (MW) and surgical wards (SW). METHODS: This is a retrospective and observational study. Demographic data, clinical features, treatment and the end-of-life care decisions of adult patients who died in wards and the intensive care unit of HU/UFSC from July/2004 to December/2008 were analyzed . For statistical analysis the Student's t, χ2 and ANOVA tests were used: (significance p <0.05). RESULTS: An analysis was made of 1124 deaths: 404 occurred in ICU, 607 in MW and 113 in SW. The overall hospital mortality rate was 5.9% (ICU=24.49%, MW=7.2%, SW=1.69%). Mean ages of patients were: ICU=56.7, MW=69.3 and SW=70.4 years (p <0.01). Withholding/withdrawing life support was performed prior to 30.7% of deaths in the intensive care unit and 10% in the wards (p <0.01). Cardiopulmonary resuscitation was not carried out in 65% of cases in ICU, 79% in MW and 62% in SW. Besides cardiopulmonary resuscitation, the more frequent withholding/withdrawing life support in the intensive care unit were vasoactive drugs and in the wards refusal of admission to intensive care unit . Do-not-resuscitate order was documented in 2.4% of cases in ICU and 2.6% in MW. Palliative and comfort care were provided to 2% of patients in ICU, 11.5% in MW and 8% in SW. Terminality of the disease was recognized in 40% of cases in ICU, 34.6% in MW and 16.8% in SW. CONCLUSIONS: The profile of patients who died and medical decisions during the end-of-life process were different in the intensive care unit, clinical and surgical wards.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):422-428
DOI 10.1590/S0103-507X2008000400016
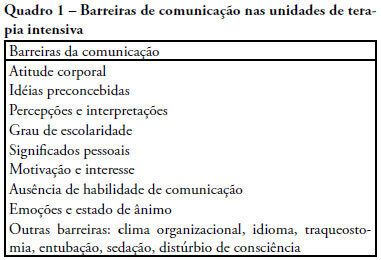
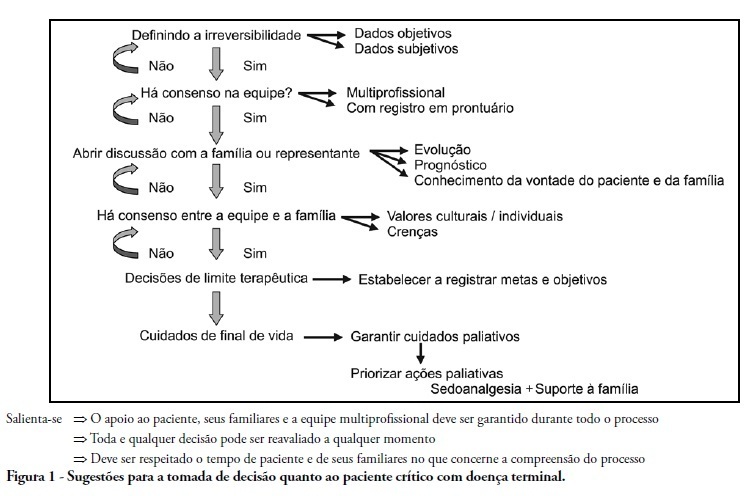
The objective of this review was to evaluate current knowledge regarding terminal illness and palliative care in the intensive care unit, to identify the major challenges involved and propose a research agenda on these issues The Brazilian Critical Care Association organized a specific forum on terminally ill patients, to which were invited experienced and skilled professionals on critical care. These professionals were divided in three groups: communication in the intensive care unit, the decision making process when faced with a terminally ill patient and palliative actions and care in the intensive care unit. Data and bibliographic references were stored in a restricted website. During a twelve hour meeting and following a modified Delphi methodology, the groups prepared the final document. Consensual definition regarding terminality was reached. Good communication was considered the cornerstone to define the best treatment for a terminally ill patient. Accordingly some communication barriers were described that should be avoided as well as some approaches that should be pursued. Criteria for palliative care and palliative action in the intensive care unit were defined. Acceptance of death as a natural event as well as respect for the patient's autonomy and the nonmaleficence principles were stressed. A recommendation was made to withdraw the futile treatment that prolongs the dying process and to elected analgesia and measures that alleviate suffering in terminally ill patients. To deliver palliative care to terminally ill patients and their relatives some principles and guides should be followed, respecting individual necessities and beliefs. The intensive care unit staff involved with the treatment of terminally ill patients is subject to stress and tension. Availability of a continuous education program on palliative care is desirable.