You searched for:"Arnaldo Dubin"
We found (12) results for your search.-
Original Article
Lack of agreement between different observers and methods in the measurement of capillary refill time in healthy volunteers: an observational study
Rev Bras Ter Intensiva. 2014;26(3):269-276
Abstract
Original ArticleLack of agreement between different observers and methods in the measurement of capillary refill time in healthy volunteers: an observational study
Rev Bras Ter Intensiva. 2014;26(3):269-276
DOI 10.5935/0103-507X.20140038
Views0See moreObjective:
Peripheral perfusion abnormalities are relevant manifestations of shock. Capillary refill time is commonly used for their evaluation. However, the reproducibility of capillary refill time measurements and their correlation with other variables of peripheral perfusion, have not been comprehensively evaluated. Our goal was to determine, in healthy volunteers, the agreement between different methods of capillary refill time quantification and different observers, as well as their correlation with other markers of peripheral perfusion.
Methods:
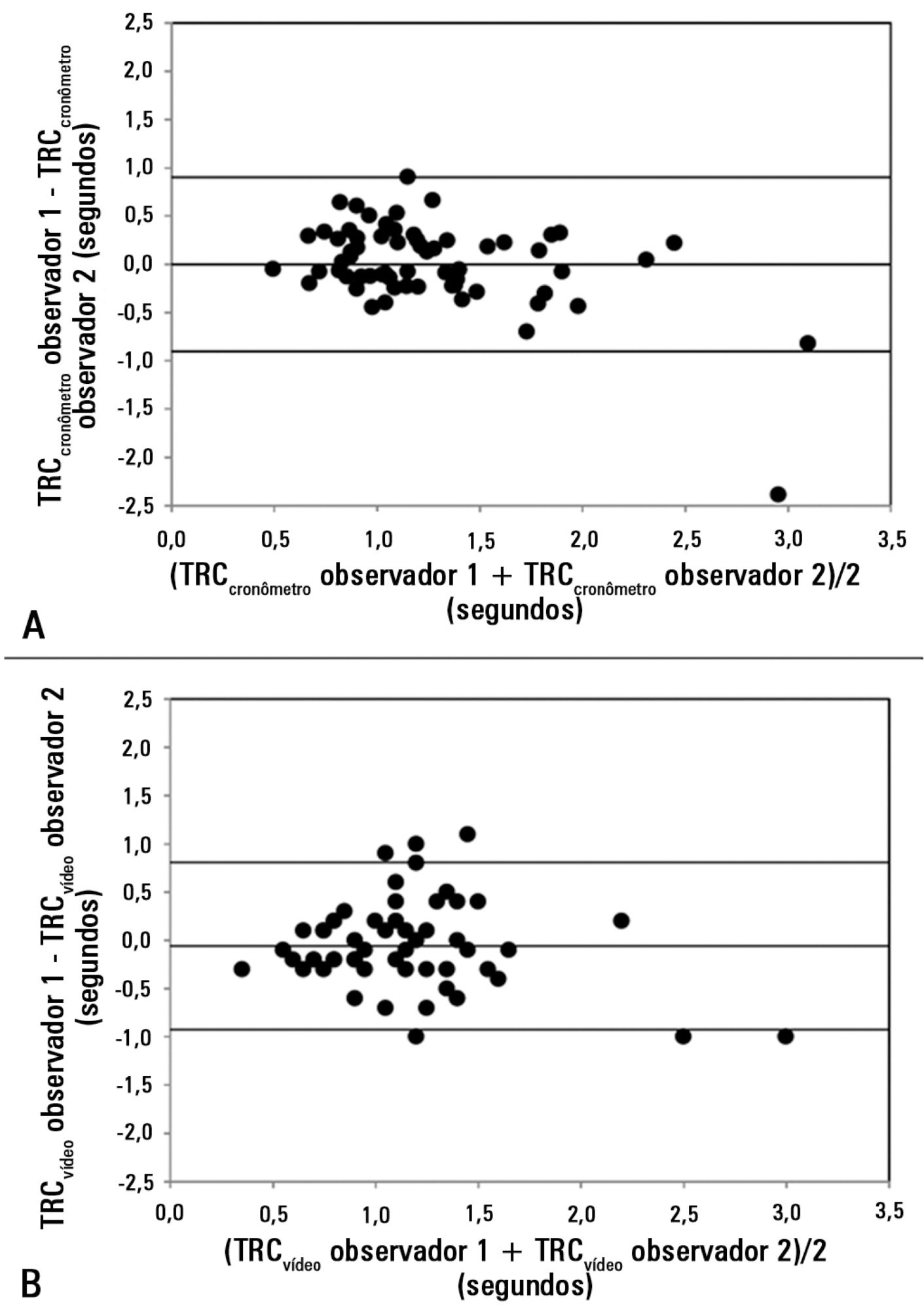
We studied 63 healthy volunteers. Two observers measured capillary refill time by means of two methods, direct view (CRTchronometer) and video analysis (CRTvideo). We also measured perfusion index (PI) derived from pulse plethysmography and finger pad temperature (Tºperipheral). The agreement between observers and methods was assessed using the Bland and Altman method. Correlations were calculated using Pearson’s correlation. A p-value<0.05 was considered significant.
Results:
The 95% limits of agreement between the two observers were 1.9 sec for CRTchronometer and 1.7 sec for CRTvideo. The 95% limits of agreement between CRTchronometer and CRTvideo were 1.7 sec for observer 1 and 2.3 sec for observer 2. Measurements of CRTchronometer performed by the two observers were correlated with Tºperipheral. Measurements of CRTvideo performed by the two observers were correlated with Tºperipheral and perfusion index.
Conclusion:
In healthy volunteers, measurements of capillary refill time performed by either different observers or different methods showed poor agreement. Nevertheless, capillary refill time still reflected peripheral perfusion as shown by its correlation with objective variables of peripheral perfusion.
-
Microcirculation in the intensive care unit
Rev Bras Ter Intensiva. 2011;23(3):249-251
-
Fluids in the postoperative period: effects of lack of adjustment to body weight
Rev Bras Ter Intensiva. 2011;23(2):170-175
Abstract
Fluids in the postoperative period: effects of lack of adjustment to body weight
Rev Bras Ter Intensiva. 2011;23(2):170-175
DOI 10.1590/S0103-507X2011000200009
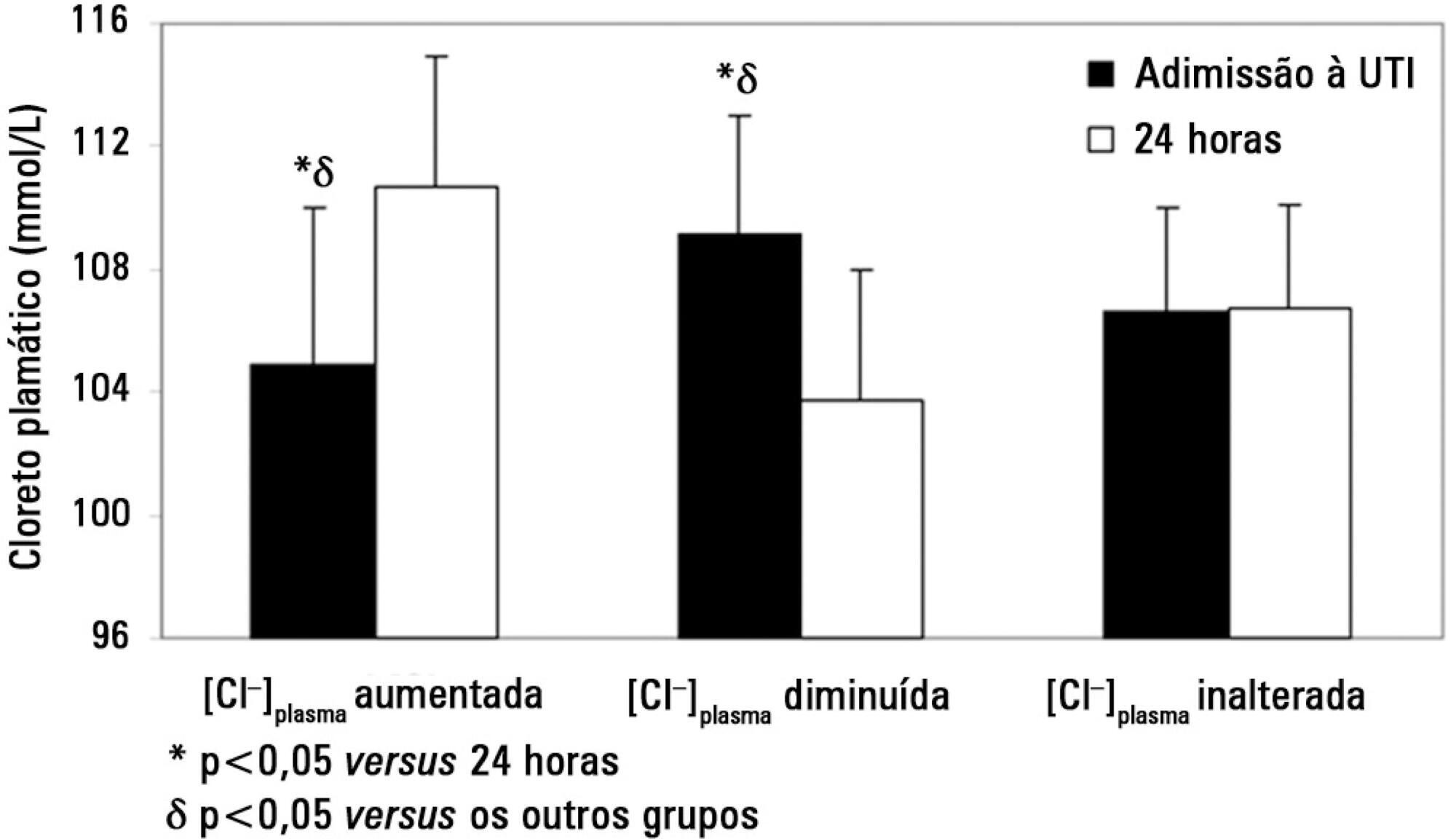
Views0See moreOBJECTIVE: To compare the differences in fluid and electrolyte balance in patients with low and high weight in the first postoperative day. METHODS: Over a period of 18 months, we prospectively evaluated 150 patients in the first 24 hours after surgery, in a university-affiliated hospital intensive care unit. Patients with low weight (< 60 kg) and high body weight (> 90 Kg) were compared in terms of fluid intake and output. RESULTS: No significant differences were observed in the volume (4334 ± 1097 vs. 4644 ± 1957 ml/24 h) and composition of the fluids administered (481 ± 187 vs. 586 ± 288 mEq [Na+]administered/24 h). The 24 h urine output was similar (2474 ± 1597 vs.2208 ± 678 ml/24 h) but low weight group showed higher electrolyte elimination (296 ± 195 vs.192 ± 117 mEq [Na+]urine /24 h, p = 0.0246). When the administered fluids were adjusted for body weight, the volume and amount of electrolytes of fluids administered were higher in the low weight group (79 ± 21 vs. 47 ± 22 ml/kg/24 h, p < 0.0001 and 8.8 ± 3.4 vs. 5.8 ± 3.3 mEq [Na+]administered/kg/24 h, p = 0.017, respectively). This group also showed higher urine output and electrolyte elimination (45 ± 28 vs. 22 ± 7 ml/kg/24 h, p = 0.0002 and 5.3 ± 3.5 vs. 1.8 ± 1.2 mEq [Na+]urine/kg/24 h, p < 0.0001, respectively). CONCLUSIONS: The lack of adjustment of the fluid therapy to body weight determined that low weight patients received more fluid than high weight patients according to their body weight. This fluid overload could be compensated by increased urine output and electrolyte elimination.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis