Abstract
Rev Bras Ter Intensiva. 2006;18(1):38-44
DOI 10.1590/S0103-507X2006000100008
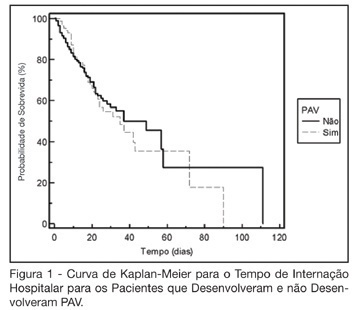
BACKGROUND AND OBJECTIVES: The ventilator-associated pneumonia (VAP) is a severe infection that presents multiple causes which can vary depending on the type of intensive care unit, type of patients, emphasizing the needs for vigilance measures with local data. The aim of this study is to describe the incidence, risk factors and mortality of VAP in patients in a surgical ICU. METHODS: Prospective cohort conducted from January 2004 to January 2005. It was included all the patients in mechanical ventilation, followed daily to collect data about demographics, diagnostic, APACHE II and TISS 28 scores, duration of mechanical ventilation, length of stay, incidence of VAP and mortality. RESULTS: 462 patients were studied; age 57.2 ± 16.6 years, 55% men. The mean APACHE II score was 18.3 and the incidence of VAP was 18.8%. The TISS score at admission OR = 1.050 (IC 95%: 1.003-1.050) and the enteral nutrition OR = 5.609 (IC 3.351-9.388) were factors associated with VAP and the prophylactic use of antibiotics was a factor of protection OR = 0.399 (IC95%: 0.177-0.902). The patients with VAP had longer length of stay in ICU (10.3 ± 10.7 vs 4.9 ± 3.3 days), higher median of duration of mechanical ventilation (4 vs 1 days), higher mean of TISS 28 (24.4 ± 4.6 vs 22.8 ± 4.5), and higher crude mortality (46 vs 28.8%) when compared with the patients without VAP. CONCLUSIONS: VAP was a frequent infection in surgical patients in mechanical ventilation. Enteral nutrition and admission TISS were risk factors and the previous use of antibiotics was protection factor to develop VAP. In our sample the results demonstrate that VAP is associated with higher duration in mechanical ventilation, longer length of stay and higher mortality.
Abstract
Rev Bras Ter Intensiva. 2006;18(2):148-153
DOI 10.1590/S0103-507X2006000200008
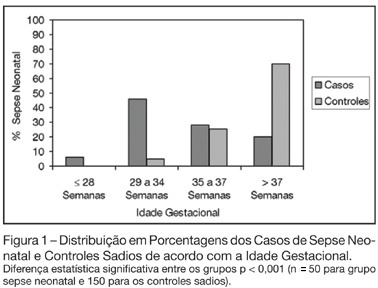
BACKGROUND AND OBJECTIVES: The determination of the risk factors to early-onset neonatal sepsis in our country is essential to prevent and reduce the mortality associated with this syndrome. Thus, the objective of this study was to determine the frequency and associated risk factors to early-onset neonatal sepsis in public hospital in Southern Brazil. METHODS: Observational, case-control study. Were included neonates with diagnostic of early-onset neonatal sepsis and as controls, neonates without neonatal infection. Were included 50 cases and 3 controls for each case resulting in a total sample of 200 patients. Associations were considered significant when p < 0.05. RESULTS: The sepsis frequency was 50.3 per 1000 born-alive. Risk factors associated to the development of neonatal sepsis were prematurity (OR 9.33; p < 0.001), low birth weight (OR 11.74; p < 0.001), maternal infection (OR 2.28; p = 0.009), mother with history of previous infant with neonatal sepsis (OR 6.43; p = 0.035) and rupture of the membranes more than 18 hours before delivery (OR 9.33; p = 0.001). CONCLUSIONS: Neonatal sepsis was very frequent in the study. Prematurity, low birth weight, maternal infection and mother’s having had a previous infant with neonatal sepsis are risk factors for early-onset neonatal sepsis.