Abstract
Rev Bras Ter Intensiva. 2006;18(2):204-206
DOI 10.1590/S0103-507X2006000200016
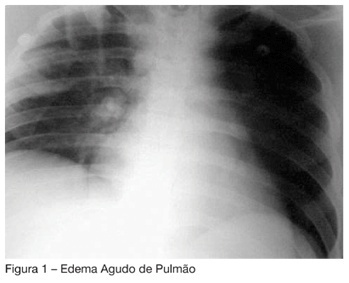
BACKGROUND AND OBJECTIVES: To present the first case reported in the Brazilian literature of liquid nitrogen intoxication. The objective of this report was to present a case of severe intoxication by liquid nitrogen, with acute lung edema and ischemic encephalopathy, which a good outcome, due to a fast diligence and a proper therapy administration. CASE REPORT: Male patient, 26 years, unconscious for one hour, in a close room with a machine to keep frozen the ice-roller ring. There was evidence of gastric aspiration and laryngeal edema. The intubation was difficult. The patient developed acute lung edema and brain edema due to hypoxia. There was a slow lung resolution with a protective ventilatory strategy for ARDS (VT 5 mL/kg, PEEP de 15 cmH2O) and corticotherapy with hydrocortisone (200 mg) every 6 h to treat bronchospasm. CONCLUSIONS: This the first case published in Brazil of nitrogen intoxication. In the international literature there are several reports of similar cases occurred in gymnasiums for hockey game. There are reports of bronchospasm exacerbations in people after the matches, even up to 10h after exposal to the gases riches in nitrogen.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):77-81
DOI 10.1590/S0103-507X2008000100012
BACKGROUND AND OBJECTIVES: Weaning patients from mechanical ventilation is a challenge in the intensive care unit (ICU) practice and is related to some complications. One of these is the pos-extubation laryngospasm, an event that can be anticipated for the cuff leak test (CLT). The objective was demonstrate that the CLT is a simple, reliable and low costs method to available the presence of obstruction in high airway in patients under weaning ventilator. CONTENTS: It was made a systematic review in databases MedLine, SciElo and LILACS with articles from 1995 to 2007. The selected studies focused the use of the CLT to predict laryngospasm and extubation failure. It was excluded studies with animals and others literature reviews. It was looked correlates the CLT with mechanical ventilation's days, age and specific groups that could beneficiates with the application of this technique. CONCLUSIONS: The CLT can be considerate a good index to predict laryngospasm pos-extubation, when considerate the studied population characteristics.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):310-316
DOI 10.1590/S0103-507X2007000300007
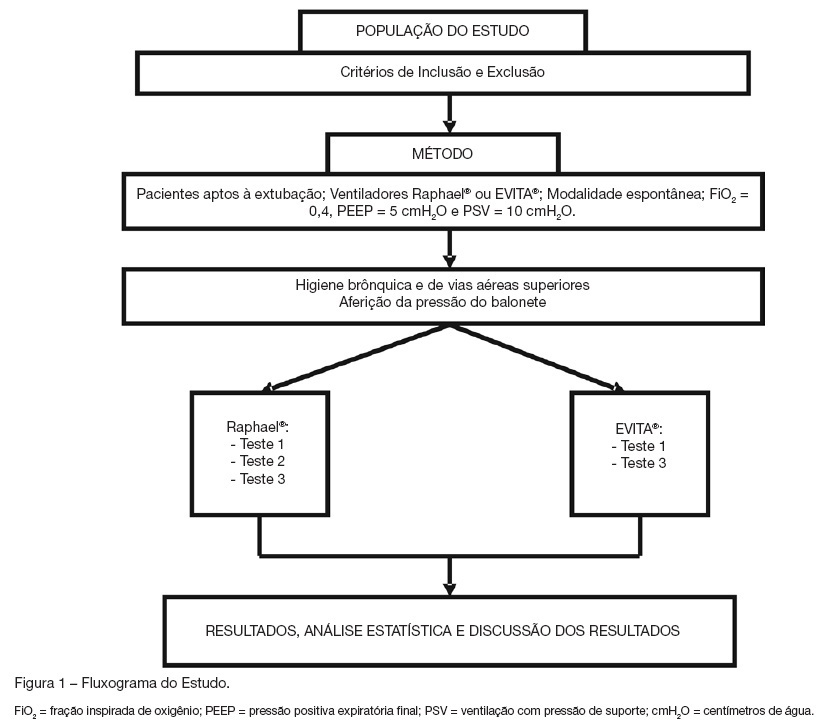
BACKGROUND AND OBJECTIVES: The cuff leak test aims to evaluate the presence of airway obstruction and normally is carried through in the controlled mode of mechanical ventilation. The objective of this study was to evaluate the cuff leak in patients breathing spontaneously, across three different methods, and to compare them. METHODS: Twenty intubated patients had been submitted to three different forms of cuff leak test, all of them in spontaneous respiration: measuring air leak buy using a ventilometer and with the patient connected to the mechanical ventilator (test 1); through the display of the mechanical ventilator (test 2); and with ventilometer and the patient detached from the mechanical ventilator (test 3). The air leak around the tracheal tube (TT) was defined as the percentage difference between the inspired tidal volume (insufflated cuff) and exhaled (deflated cuff). The air leak differences between the three tests were evaluated, as well as their correlations to three variables: cuff pressure, TT diameter and intubation time. RESULTS: Statistically significant (p < 0.05) air leak difference was observed between the tests 1 and 2 in relation to the test 3 in the general and regarding time intubation below 48h and cuff pressure below 20 cmH2O. Regarding the tube diameter, it had been difference only between tests 2 and 3 for 8.5 mm tubes. CONCLUSIONS: The cuff leak test in spontaneous ventilation seems to be more accurate when the patient is connected to the mechanical ventilator, and that additional studies are needed to determine the real contribution of the test in this ventilation mode to predict laryngeal edema.