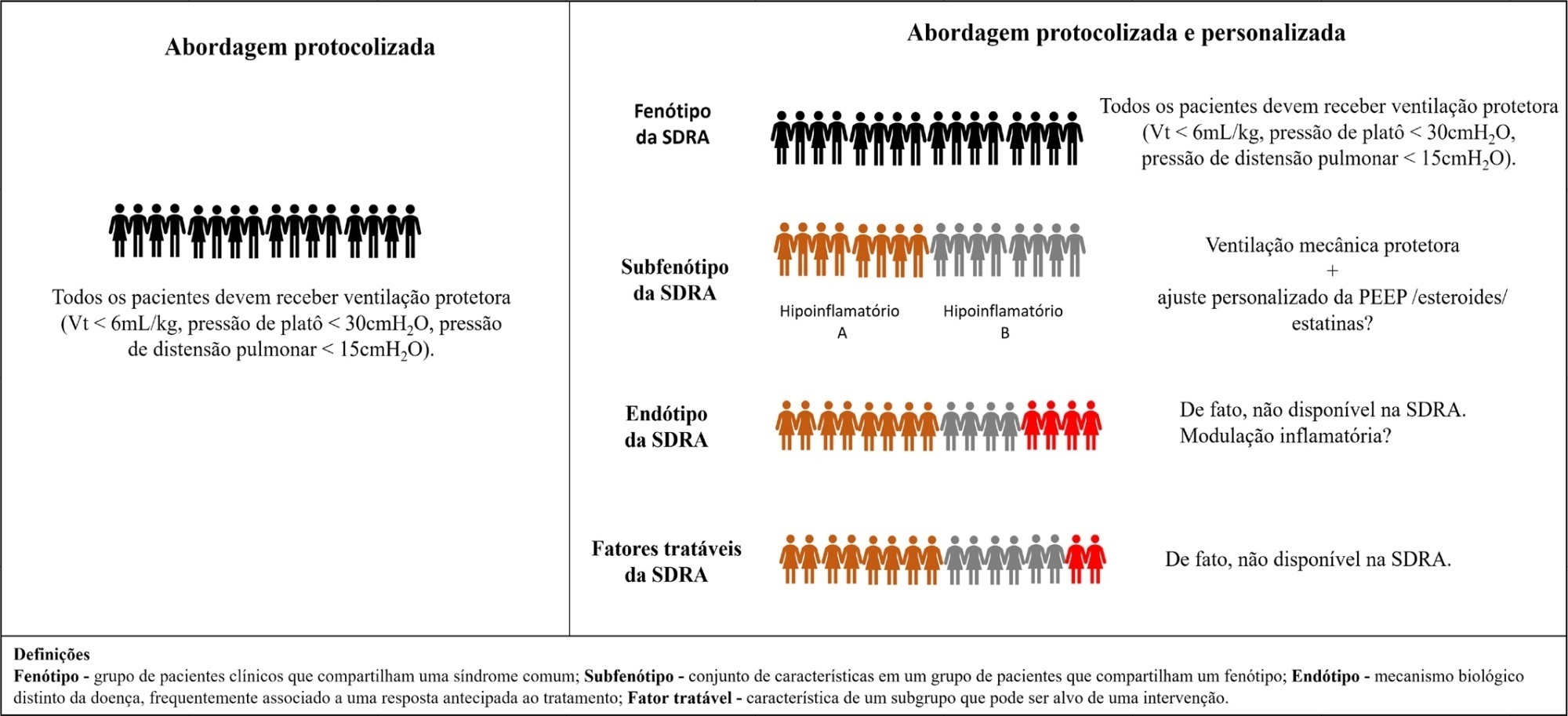
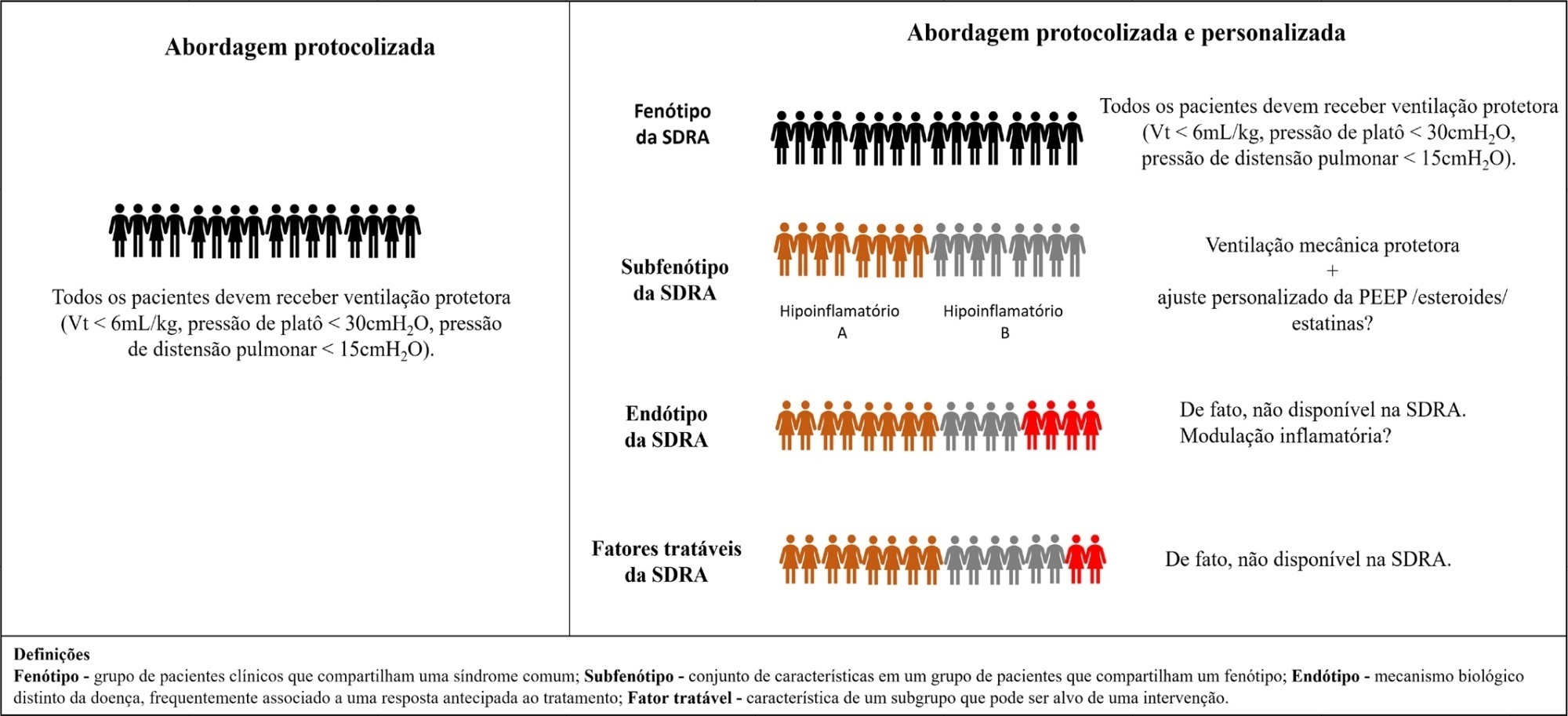
In recent decades, successful quality improvement initiatives in critical care have been tested, and among the included principles were to “do no harm” (which means to prevent intensive care unit-acquired complications and to avoid overtreatment) and to provide early interventions for acute conditions (i.e., antibiotics for sepsis, as well as reperfusions for stroke and myocardial infarction). However, a degree of imbalance is present in the abovementioned premises. Most of the improved outcomes that have been observed in critical care in the past decades can be attributed to the prevention of complications (i.e., nosocomial infections, protective ventilation and deep vein thrombosis) and to the treatment of well-defined etiologic conditions (i.e., stroke and myocardial infarction), thus resulting in very prevalent syndromes (i.e., acute respiratory distress syndrome – ARDS and sepsis) comprising a minor portion of the effective treatments, which partially explains their current elevated mortality rates. Proponents of the protocolized care have used these arguments to promote the broad implementation of well-standardized, evidence-based practices aiming to reduce variations of care and to improve outcomes. Furthermore, those individuals proposing personalized care state that a physiology-based approach would hold the key to improving outcomes in patients with shock, acute respiratory failure (ARF), brain injury and other conditions.
Studies concerning psychology and decision-making show that when we evaluate and compare a range of data points, we tend to neglect the relative strength of the evidence and its spectrum and treat the evidence as being simply binary. This is known as the “binary bias”. Somehow, this approach (coupled with the tendency in critical care to group heterogeneous patient populations under syndromes (i.e., ARF, ARDS, sepsis and delirium) is well represented in the treatment protocols that are available in intensive care units (i.e., sepsis and ventilator-associated pneumonia bundles). In contrast, the pure physiology-based approach has been the basis of several failed interventions in ventilatory support, glucose control and delirium, among other interventions.
[…]
Search
Search in:

Comments