To report on the currently available prediction models for the development of acute kidney injury in heterogeneous adult intensive care units.
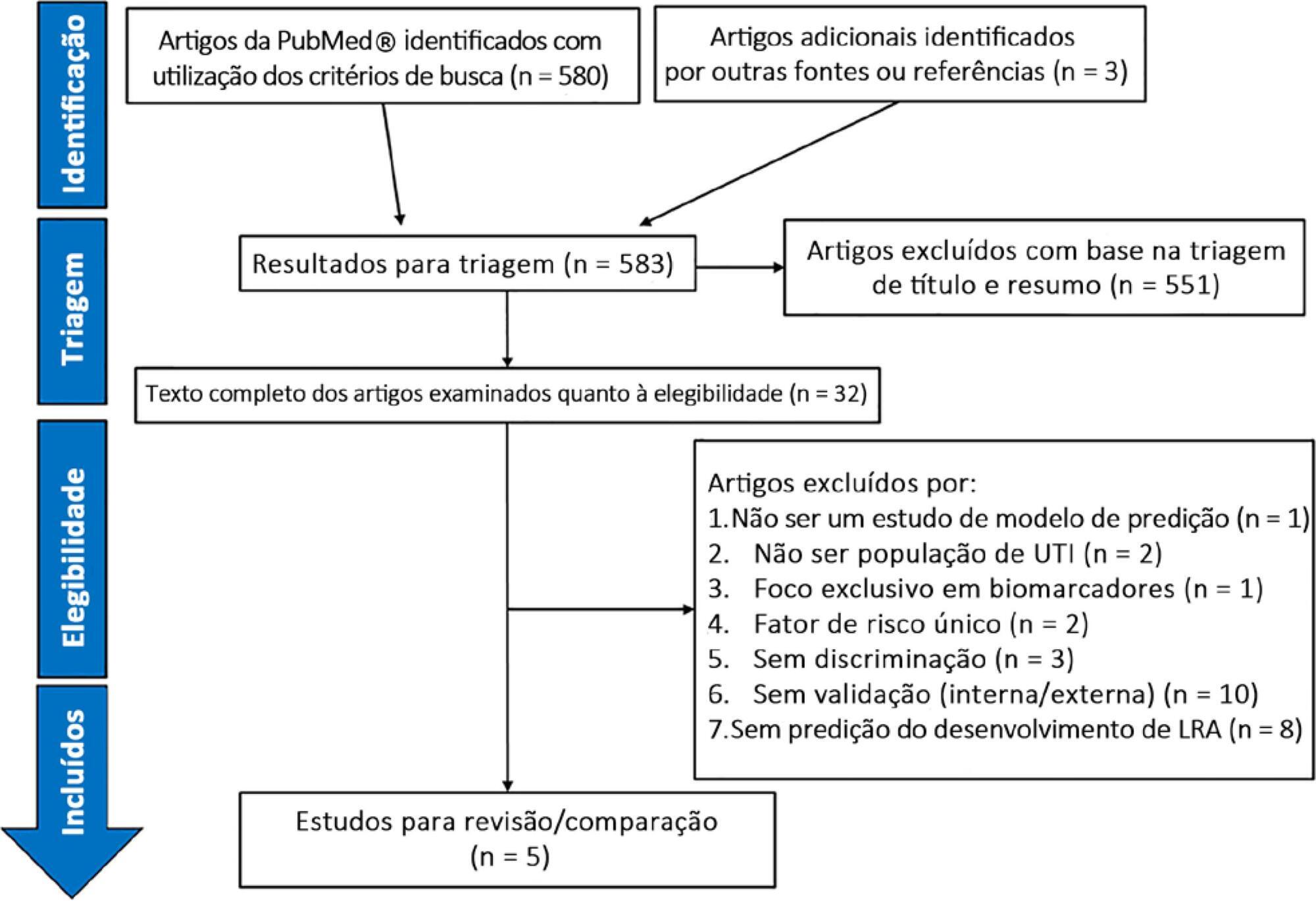
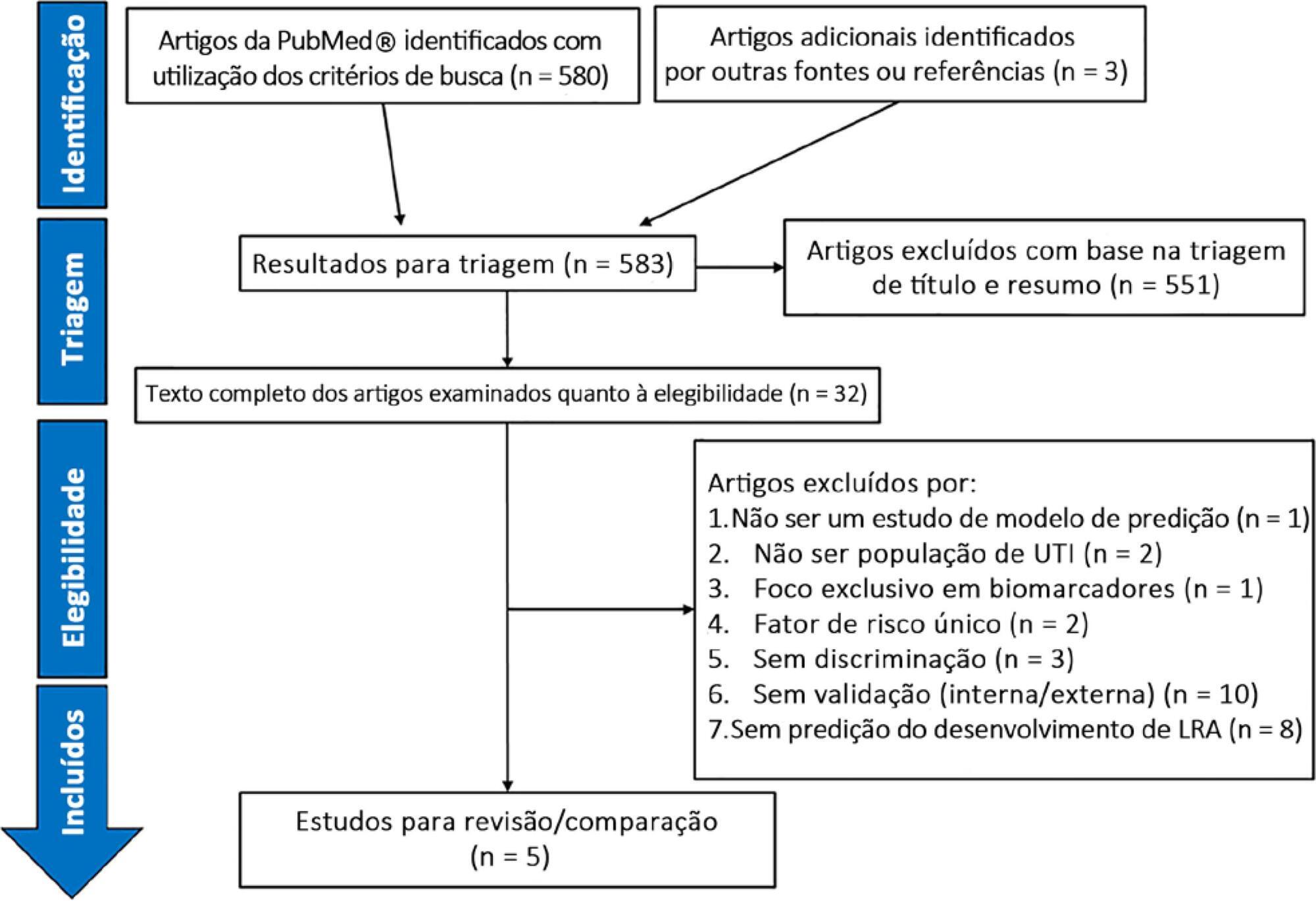
A systematic review of clinical prediction models for acute kidney injury in adult intensive care unit populations was carried out. PubMed® was searched for publications reporting on the development of a novel prediction model, validation of an established model, or impact of an existing prediction model for early acute kidney injury diagnosis in intensive care units.
We screened 583 potentially relevant articles. Among the 32 remaining articles in the first selection, only 5 met the inclusion criteria. The nonstandardized adaptations that were made to define baseline serum creatinine when the preadmission value was missing led to heterogeneous definitions of the outcome. Commonly included predictors were sepsis, age, and serum creatinine level. The final models included between 5 and 19 risk factors. The areas under the Receiver Operating Characteristic curves to predict acute kidney injury development in the internal validation cohorts ranged from 0.78 to 0.88. Only two studies were externally validated.
Clinical prediction models for acute kidney injury can help in applying more timely preventive interventions to the right patients. However, in intensive care unit populations, few models have been externally validated. In addition, heterogeneous definitions for acute kidney injury and evaluation criteria and the lack of impact analysis hamper a thorough comparison of existing models. Future research is needed to validate the established models and to analyze their clinical impact before they can be applied in clinical practice.
Search
Search in:

Comments