Tissue hypoperfusion and subsequent limited oxygen transport are critical features conducting to organ failure during shock states. Therefore, early identification of tissue hypoperfusion and adequate resuscitation are key for improving the probability of survival after septic shock.(,) However, how to identify organ perfusion abnormalities at the bedside and select the type and amount of fluids required to improve tissue hypoxia remain highly controversial. Traditionally, clinical signs, such as reduced blood pressure and urinary output, altered consciousness, and mottled skin, have been used to identify tissue perfusion abnormalities. Consequently, current hemodynamic monitoring during shock states mainly focuses on detection of pressure-derived hemodynamic variables related to systemic circulation. However, it has been largely recognized that monitoring these macro-hemodynamic variables is not sufficient to rule out persistent abnormalities of tissue oxygenation. Indeed, the usefulness of resuscitation targets, such as global oxygen-derived parameters, has been strongly questioned,() and recent data have failed to demonstrate beneficial effects of using central venous oxygen saturation as a goal of resuscitation.(–)
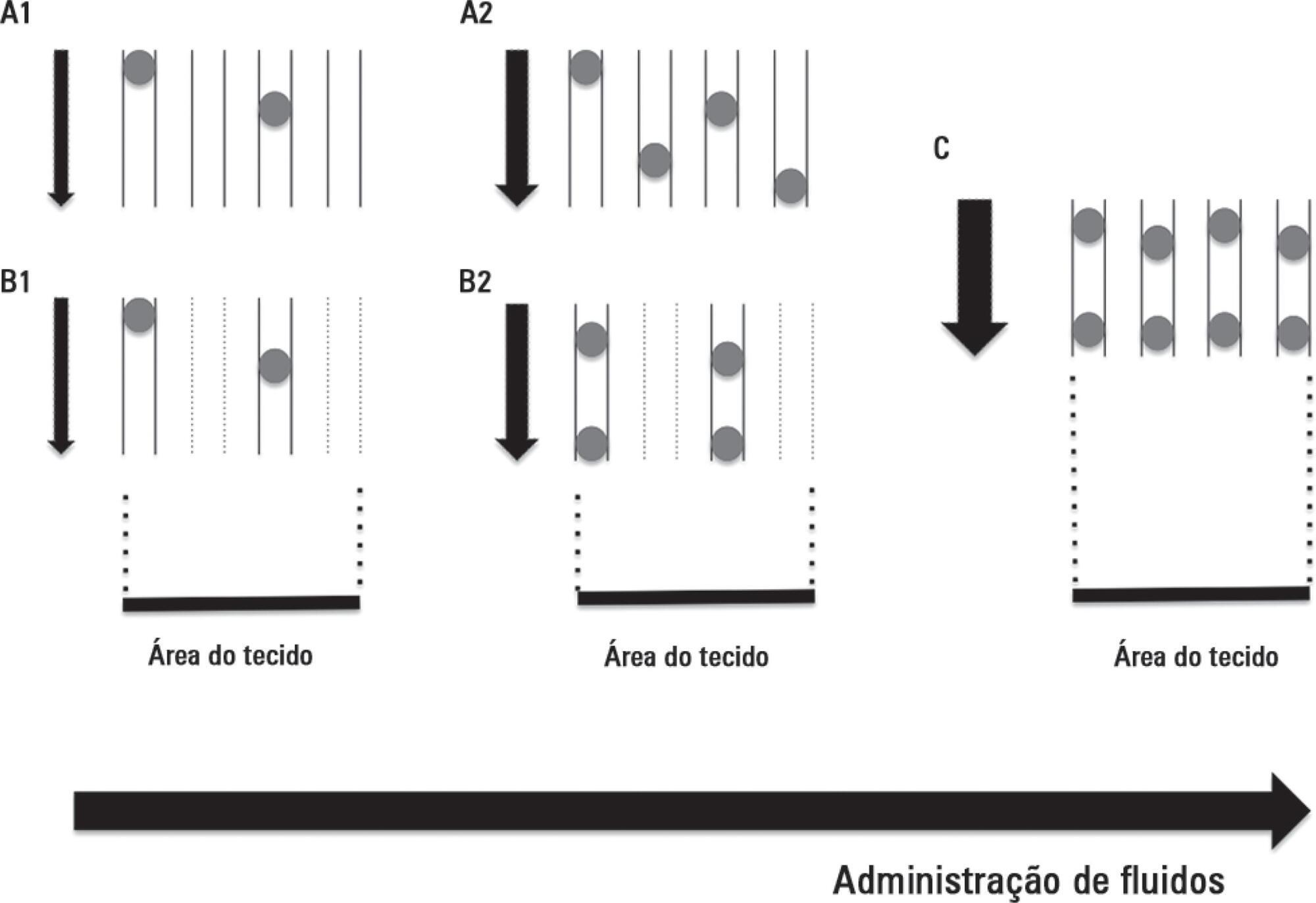
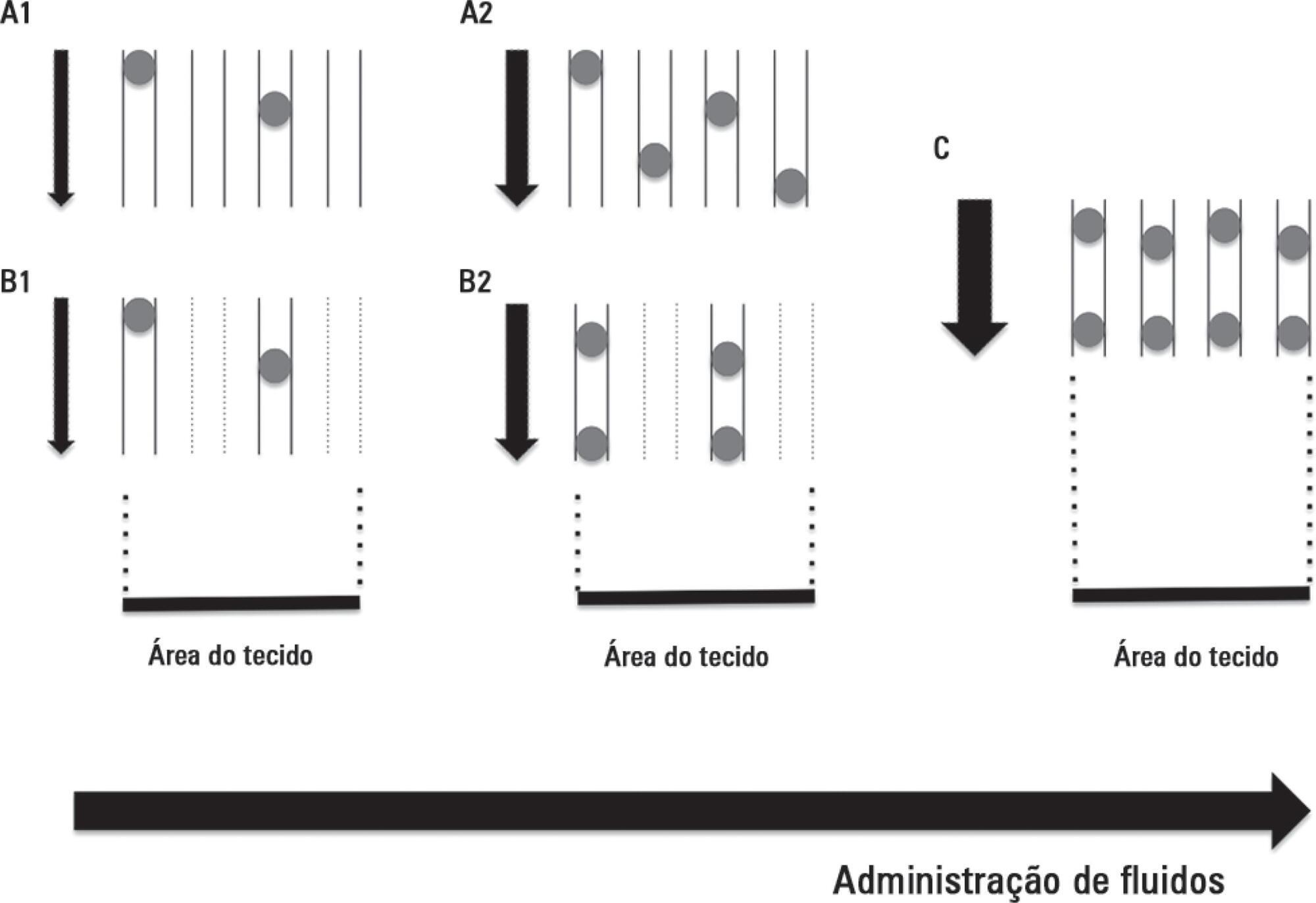
Fluid resuscitation therapy primarily aims to optimize cardiac output on the assumption that increasing macro blood flow can improve the convective transport of oxygen to the tissues and, therefore, maintain cellular respiration and support organ function.(,) Thus, fluid therapy targeting central venous pressure has been widely recommended to achieve adequate cardiac performance.() However, high positive fluid balances have also been associated with unfavorable clinical outcomes.() In this sense, dynamic approaches to assessing volume responsiveness to fluid administration seem to be superior to static variables.(,) Unfortunately, macro-hemodynamic optimization guided by either dynamic or static variables does not guarantee adequate tissue perfusion or adequate cellular respiration.
[…]
Search
Search in:

Comments